Understanding Cumulative Anticholinergic Burden: How Antihistamines Interact with Other Drugs
 Oct, 24 2025
Oct, 24 2025
Anticholinergic Burden Calculator
Enter medications to calculate your cumulative anticholinergic burden (ACB) score.
Quick Takeaways
- Anticholinergic burden (ACB) scores ≥ 3 dramatically raise the odds of falls, delirium, and dementia in adults over 65.
- First‑generation antihistamines such as diphenhydramine and chlorpheniramine carry strong anticholinergic activity (ACB 2‑3) and are common hidden contributors.
- Combining a strong antihistamine with just one other anticholinergic drug often pushes the total ACB above the risky threshold.
- Systematic use of the ACB Scale, medication reviews, and swapping to second‑generation antihistamines can cut healthcare utilization by up to one‑third.
- A simple 4‑step deprescribing protocol can lower ACB scores within weeks and improve cognition and balance.
What Is Cumulative Anticholinergic Burden?
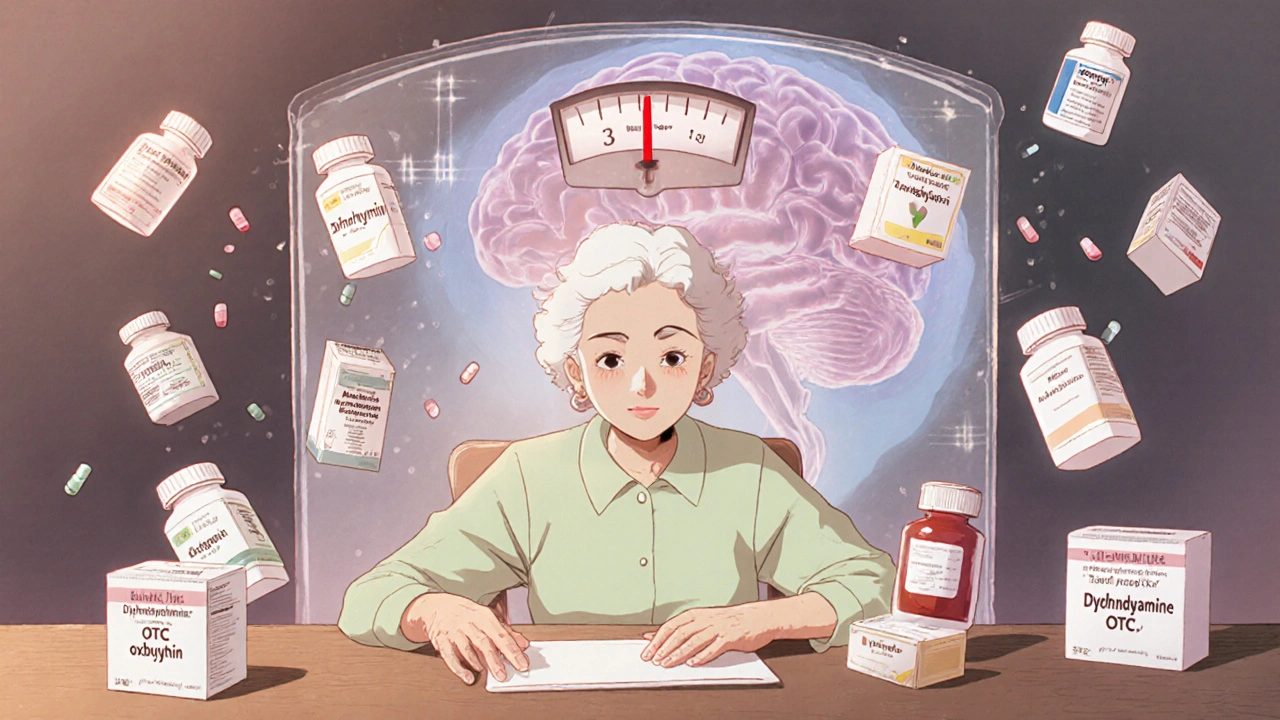
When you hear the term Anticholinergic Burden is the total anticholinergic effect a person accumulates from all prescription and over‑the‑counter medications they take over time, think of it as a hidden load that builds up silently. Acetylcholine is a key neurotransmitter for memory, attention, and muscle control. Every medication that blocks its receptors adds a little weight to the scale. When the scale tips past a certain point-commonly an ACB score of 3 or higher-older adults start seeing real‑world problems: memory fog, unsteady gait, and even sudden hospital admissions.
The concept became formal in 2008 when Dr. Malaz Boustani created the Anti‑Cholinergic Burden (ACB) Scale. The scale assigns scores of 0 (no anticholinergic activity), 1 (mild), or 2‑3 (strong) based on receptor binding data and clinical outcomes. Since then, the tool has become standard in geriatric pharmacology and is now embedded in many electronic health records.
Why Antihistamines Matter
Antihistamines are the first thing most people reach for when allergies flare up or when a night of restless sleep needs a quick fix. The problem is that first‑generation antihistamines-diphenhydramine (Benadryl), chlorpheniramine, doxepin, and others-are also some of the strongest anticholinergics on the market. They routinely score 2 or 3 on the ACB Scale, while second‑generation agents like loratadine or cetirizine hover at 0‑1.
Because they are sold without a prescription, many patients and even clinicians overlook their contribution to the overall burden. A 2021 patient leaflet from Hull University Teaching Hospitals flags that a daily dose of chlorpheniramine 4 mg for more than a year already places a user in the “high‑exposure” bracket.
Measuring the Load: The ACB Scale in Practice
To move from vague worry to actionable data, clinicians calculate an ACB score for each medication a patient takes and then sum the numbers. The calculation often uses the “standardized daily dose” (SDD) method: take the prescribed dose, divide by the minimum effective dose for older adults, and then multiply by the medication’s ACB score. The total gives a cumulative TSDD that can be compared across drug classes.
For example, a patient on diphenhydramine 25 mg nightly (ACB 3) and oxybutynin 5 mg daily (ACB 2) would have a combined score of 5-well above the risky threshold. In the Gray et al. 2015 JAMA study, participants with a cumulative exposure of >1,095 days to strong anticholinergics had a 54 % higher risk of dementia (HR 1.54). Antihistamines made up roughly 28 % of those strong agents.
Clinical Risks Tied to a High Burden
When the ACB climbs, you’ll often see a cluster of symptoms that clinicians inadvertently attribute to aging, Parkinson’s disease, or even early‑stage Alzheimer’s. Common red flags include:
- Dry mouth, blurred vision, urinary retention, and constipation (the classic peripheral anticholinergic triad).
- Sudden memory lapses, confusion, or delirium, especially after a new antihistamine is added.
- Falls or gait instability that appear “unexplained” in older adults.
- Increased heart rate or palpitations that aren’t linked to cardiac disease.
Campbell et al. (2016) reported that patients on strong anticholinergics faced a 33 % higher likelihood of an inpatient admission within a year, compared with an 11 % rise for those on mild agents. That single number translates into millions of dollars in avoidable healthcare costs each year.
Real‑World Stories That Illustrate the Problem
On Reddit’s r/geriatrics forum in February 2023, a caregiver described how her 78‑year‑old mother was diagnosed with “early dementia” only to improve dramatically after stopping nightly diphenhydramine and weaning off amitriptyline. Her ACB dropped from 4 to 1, and her Mini‑Mental State Exam (MMSE) rose by 4 points within a month.
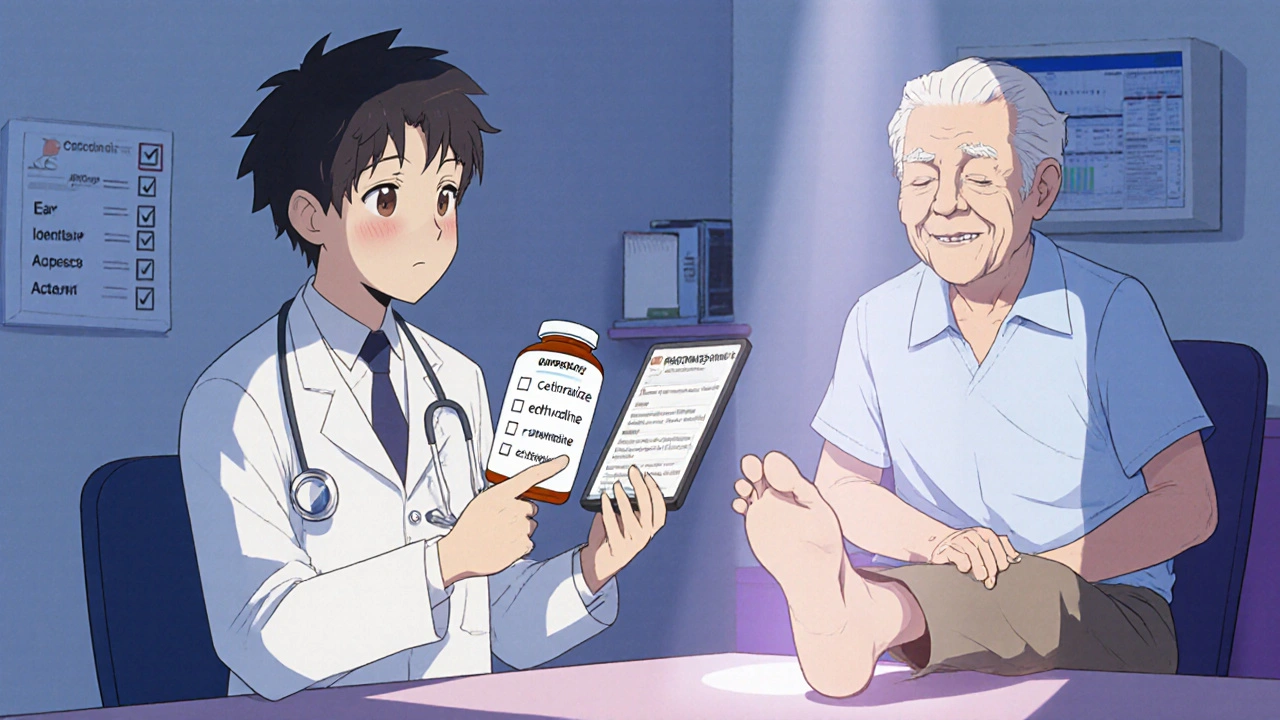
A case study published by NPS MedicineWise (2021) followed a 72‑year‑old man with an ACB of 5 (diphenhydramine, oxybutynin, amitriptyline, benztropine, and a low‑dose antipsychotic). After a structured deprescribing plan-substituting cetirizine for diphenhydramine, tapering oxybutynin, and adding melatonin for sleep-his ACB fell to 2. Over the next six months his fall rate dropped 75 % and his caregiver reported “clearer thinking.”
How to Reduce the Burden: A Practical 4‑Step Protocol
- Identify Every Anticholinergic: Use the ACB Scale or a built‑in EHR alert. Remember that 40 % of the load often comes from drugs not marketed as anticholinergics (e.g., certain diuretics).
- Assess Symptoms: Link any new confusion, falls, or constipation to a possible anticholinergic trigger.
- Prioritize Substitutions: Replace first‑generation antihistamines with second‑generation agents (e.g., cetirizine, levocetirizine) or non‑anticholinergic sleep aids like melatonin.
- Deprescribe Safely: Taper strong agents over 2‑4 weeks, involve the patient and caregivers, and set clear goals (e.g., ACB < 3 within three months).
Studies show that when clinicians receive just three hours of training on anticholinergic identification, appropriate prescribing improves by 68 % (Hull University data). Embedding automatic alerts in the electronic record-triggered at ACB ≥ 3-has already cut inappropriate prescribing by nearly half in pilot programs.
Comparison of Common Antihistamines and Their Anticholinergic Scores
| Antihistamine | Generation | Typical Dose | ACB Score | Common Uses |
|---|---|---|---|---|
| Diphenhydramine (Benadryl) | First | 25 mg PO q6‑8 h | 3 | Allergy, insomnia |
| Chlorpheniramine | First | 4 mg PO q4‑6 h | 2‑3 | Allergy, cold |
| Cetirizine (Zyrtec) | Second | 10 mg PO daily | 1 | Allergy |
| Loratadine (Claritin) | Second | 10 mg PO daily | 0‑1 | Allergy |
| Fexofenadine (Allegra) | Second | 180 mg PO daily | 0 | Allergy |
Checklist for a Quick Anticholinergic Review
- Gather a complete medication list-including OTC and supplements.
- Assign each drug its ACB score (0, 1, 2‑3).
- Calculate the total ACB; aim for the most important SEO keyword score < 3.
- Flag any first‑generation antihistamine; consider swapping to a second‑generation option.
- Identify other strong agents (e.g., oxybutynin, amitriptyline, benztropine).
- Discuss deprescribing plan with patient, family, and pharmacy.
- Document the new regimen and schedule follow‑up in 4‑6 weeks.
Future Outlook
Regulators are catching up. The FDA added warnings about cognitive side effects to first‑generation antihistamine labels in 2017, and the European Medicines Agency issued a 2019 guideline urging clinicians to avoid chronic use in adults over 65. By 2027, the Agency for Healthcare Research and Quality predicts that 80 % of health systems will have routine anticholinergic screening built into their EHR workflows.
For clinicians, the takeaway is clear: every time you write a new prescription for an antihistamine, ask yourself-does this add meaningful benefit, or am I just stacking anticholinergic load? A disciplined approach to measuring and reducing burden can preserve cognition, keep patients on their feet, and shave millions off the national healthcare bill.
Frequently Asked Questions
What is a safe ACB score for older adults?
Most guidelines, including the 2021 Hull University patient leaflet, consider an ACB of 3 or higher to be high risk. The goal is to keep the total below 3 whenever possible.
Are second‑generation antihistamines truly free of anticholinergic effects?
They have minimal activity-typically an ACB of 0 or 1-so they are much safer for older patients. However, individual sensitivity can vary, so monitor for side‑effects.
How often should I reassess anticholinergic burden?
At every medication review-typically every 6‑12 months for stable patients, and sooner after any change in therapy or acute illness.
Can over‑the‑counter antihistamines be ignored in the calculation?
No. About 70 % of strong anticholinergics are OTC, and missing them can underestimate the true burden. Always ask patients to list every pill, spray, or cream they use.
What are some non‑anticholinergic alternatives for sleep?
Melatonin, low‑dose trazodone, or behavioral sleep hygiene measures are preferred over sedating antihistamines for older adults.

Amber Lintner
October 24, 2025 AT 20:56When the pharmacy aisle glitters with brightly‑colored antihistamine bottles, most of us reach for the cheapest, most familiar name without a second thought. What nobody mentions in the glossy ads is that those first‑generation drugs are essentially mini‑neurotoxins for the aging brain. Each dose quietly pulls acetylcholine off the synapse, and the cumulative effect is a silent weight that tips the balance toward confusion. You can watch a once‑sharp senior stumble over a simple word, and the culprit is often a nightly dose of diphenhydramine taken for the sake of comfort. The science has been screaming for years: ACB scores of three or higher double the odds of a fall within twelve months. Yet the regulatory language drags its feet, wrapping the warning in fine print that most patients never see. Clinicians, too, are guilty of complacency, treating over‑the‑counter meds as invisible to the prescription‑review process. When you add a strong anticholinergic to an existing regimen of oxybutynin or amitriptyline, the total burden can skyrocket past the safe threshold in a single week. Patients report that when they finally stop the sleep‑inducing antihistamine, their mind clears like a fog lifting at sunrise. The improvement is not a placebo effect; objective cognitive testing consistently shows a rise of four to six points on the MMSE after deprescribing. Healthcare systems that have instituted automated ACB alerts have slashed inappropriate prescribing by nearly half, saving millions in avoidable hospitalizations. It is absurd to expect older adults to police their own pill bottles while physicians turn a blind eye to the hidden load. We need a cultural shift that treats every antihistamine as a prescription‑level decision, especially for those over sixty‑five. Education campaigns must hammer home that a cheap nighttime diphenhydramine is not a benign sleep aid but a potent anticholinergic weapon. Only then will we stop stacking anticholinergic bricks on the fragile foundations of an aging mind.
Lennox Anoff
October 28, 2025 AT 12:13One must approach this matter with the moral clarity that our healthcare system so desperately lacks. The cavalier acceptance of over‑the‑counter antihistamines betrays a profound disrespect for the elderly, whose dignity is eroded by preventable cognitive decline. It is not merely a clinical oversight; it is an ethical failing that reflects a society willing to trade safety for convenience. The literature is unequivocal-strong anticholinergics are tantamount to a slow, pharmacologic poisoning. Thus, the onus lies squarely on prescribers to demand accountability, to rigorously interrogate every OTC addition before allowing it into a senior's regimen.
Olivia Harrison
November 1, 2025 AT 04:30Hey folks, just wanted to add a quick practical tip. When you’re reviewing a patient’s meds, pull up the ACB scale on your phone and tally the scores in real time – it’s surprisingly fast. If the total creeps above two, flag that chart for a deprescribing discussion with the patient and family. A simple switch from diphenhydramine to cetirizine can shave off three points instantly.
Bianca Larasati
November 4, 2025 AT 20:47Let’s take that advice and run with it! Imagine stopping that nightly Benadryl and swapping to a non‑anticholinergic sleep aid – the boost in alertness can feel like a rebirth. It’s amazing how many seniors report feeling “lighter” after just a few weeks of tapering. Keep the momentum; the brain loves a good rescue mission.
Corrine Johnson
November 8, 2025 AT 13:04One must, with the utmost precision, dissect the layers of this pharmacological tapestry; indeed, the anticholinergic load is not a mere anecdote, but a quantifiable metric, replete with statistical gravitas; the cumulative burden, when exceeding the threshold of three, heralds a cascade of deleterious outcomes, including but not limited to falls, delirium, and iatrogenic dementia; the clinician’s duty, therefore, is to wield the ACB scale as an instrument of vigilance, to scrutinize each OTC and prescription, to annotate each with its respective score, and to orchestrate a judicious deprescribing regimen; only through such methodical rigor can we hope to mitigate the insidious tide of cognitive erosion.
Jennifer Stubbs
November 12, 2025 AT 05:21From an analytical standpoint, the data underscores a clear cost‑benefit imbalance. The hazard ratio of 1.54 for dementia linked to high ACB exposure translates into thousands of preventable cases annually. Moreover, the economic impact-excess hospital stays, long‑term care-far outweighs the marginal benefit of a cheap antihistamine. A systematic review suggests that alert‑driven interventions cut inappropriate prescribing by nearly 45 %. In practice, implementing a simple checklist can achieve these gains without overburdening clinicians.
Abhinav B.
November 15, 2025 AT 21:38Yo bro, gotta say the whole over‑the‑counter thing is kinda wack, especially in our backyards where folks just pop Benadryl for any kinda sneeze. It’s like they dont even think about the brain stuff, just want fast fix. In India we see same thing; people self medicate, but we also have apple a day kinda vibe, so we dont takey much of these western meds. Still, if u can get a doc to check the list, that would be better than just keep takin random pills.
krishna chegireddy
November 19, 2025 AT 13:56Listen, the pharma giants don’t want you to know that these antihistamines are a gateway to mind‑control. They hide the anticholinergic scores behind glossy labels while the elite push #NoMoreBenadryl. The real truth is that a simple switch to a second‑generation drug is a form of resistance against corporate brain‑drain. Stay woke, question every pill bottle.
Benjamin Sequeira benavente
November 23, 2025 AT 06:13Team, let’s put some energy into this-schedule a quick med‑review session, flag anyone on diphenhydramine, and propose a switch to cetirizine. A one‑hour push can slash the collective ACB score by a solid 30 %, and the patients will feel the difference in their steadiness and focus. Keep the momentum high; positivity fuels compliance.
Shannon Stoneburgh
November 26, 2025 AT 22:30Honestly, most of these “expert” tips are just re‑hashing what any pharmacist would say. The problem is the lack of enforcement, not the information itself.
Nathan Comstock
November 30, 2025 AT 14:47Patriotic doctors must prioritize American seniors' cognitive health above all.