Furosemide and Dental Health: What You Need to Know for a Healthy Smile
 Oct, 27 2025
Oct, 27 2025
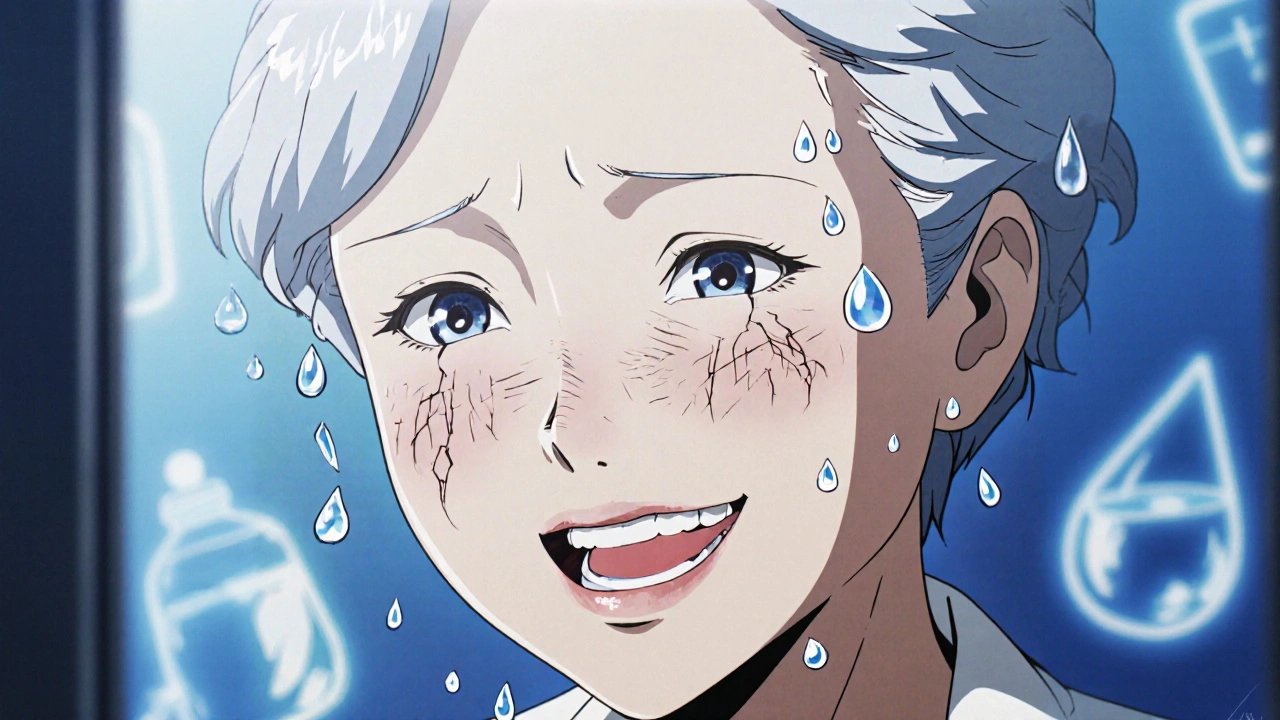
If you’re taking furosemide for high blood pressure, heart failure, or fluid retention, you might not think twice about your teeth. But this common diuretic can quietly affect your oral health - and many people don’t realize it until they start noticing dry mouth, gum issues, or tooth sensitivity. The truth? Furosemide doesn’t directly rot your teeth, but it creates conditions that make dental problems much more likely.
How Furosemide Affects Your Mouth
Furosemide works by making you pee more. That’s how it reduces swelling and lowers blood pressure. But every time you urinate, you’re also losing electrolytes - sodium, potassium, magnesium - and water. And when your body loses too much water, your saliva production drops. Saliva isn’t just for comfort; it’s your mouth’s natural defense system.
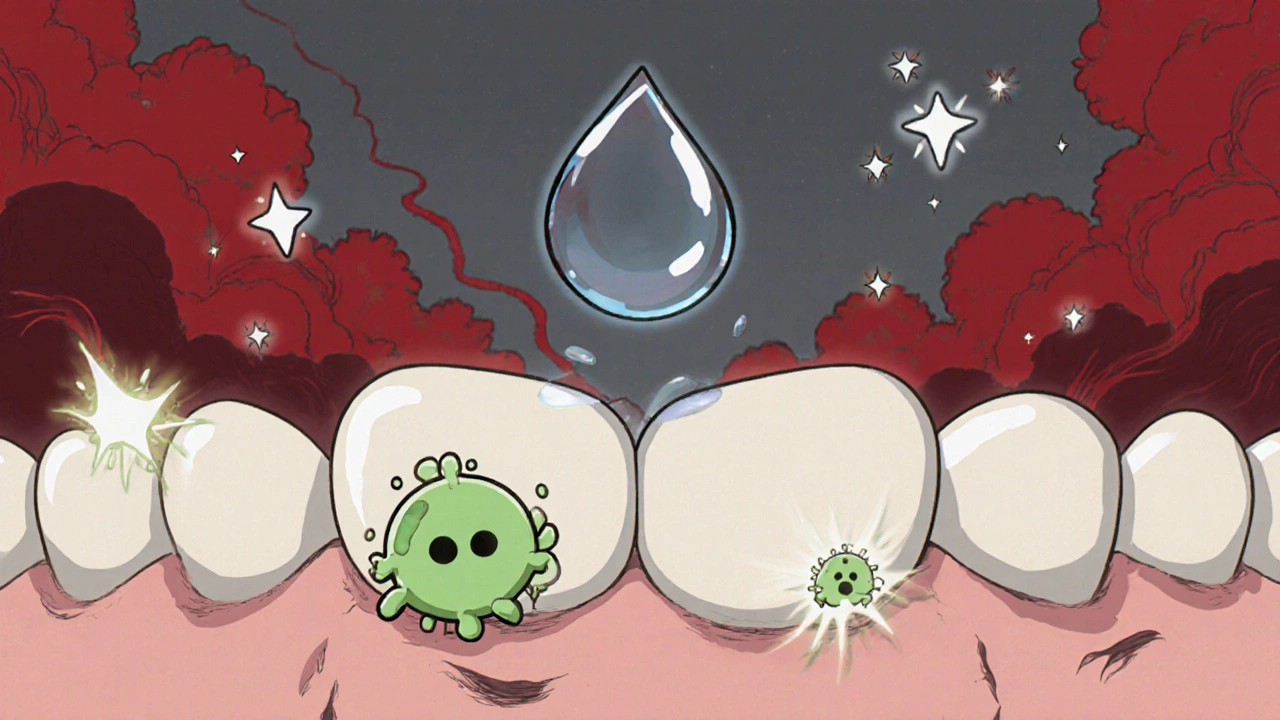
Without enough saliva, your mouth becomes dry. That’s called xerostomia. Dry mouth means bacteria aren’t washed away as they should be. Sugar from food sticks around longer. Acid builds up. Plaque hardens into tartar. And suddenly, cavities appear where none existed before. Gum disease follows quickly - inflamed, bleeding gums, receding tissue, even loose teeth.
A 2023 study in the Journal of Clinical Pharmacy and Therapeutics found that patients on long-term furosemide were 2.3 times more likely to report moderate to severe dry mouth than those not taking diuretics. And among those patients, 41% developed new cavities within 18 months - even if they brushed twice daily.
Why Dry Mouth Is More Dangerous Than You Think
Most people think dry mouth is just annoying. It’s not. It’s a silent dental emergency.
Saliva does three critical jobs:
- Washes away food particles and sugars
- Neutralizes acids from bacteria and drinks
- Re-mineralizes tooth enamel with calcium and phosphate
When saliva dries up, all three functions fail. Your teeth start to demineralize. Enamel weakens. Sensitivity to hot, cold, or sweet foods creeps in. You might notice a sticky feeling in your mouth when you wake up. Or your tongue feels rough, like sandpaper.
And here’s something few doctors mention: furosemide can also alter the pH of your saliva. Normally, saliva is slightly alkaline - around 7.0 to 7.5. When it becomes more acidic - below 6.5 - your enamel begins to dissolve. This isn’t just about drinking soda. Even a normal diet can become harmful when saliva can’t buffer the acid.
5 Practical Tips to Protect Your Teeth on Furosemide
You don’t have to stop taking furosemide. But you do need to adjust your dental routine. Here’s what works:
- Drink water - but not all at once. Sip water throughout the day. Don’t wait until you’re thirsty. Aim for at least 2 liters daily, unless your doctor says otherwise. Keep a bottle by your bed and take a sip before you sleep.
- Use fluoride toothpaste and rinse. Look for toothpaste with at least 1,350 ppm fluoride. Brush twice a day, but don’t rinse with water after. Spit out the excess - let the fluoride sit on your teeth. Use a fluoride mouthwash once a day, preferably at night.
- Chew sugar-free gum with xylitol. Xylitol doesn’t feed bacteria. In fact, it reduces them. Chewing gum for 10-15 minutes after meals boosts saliva flow naturally. Try Spry or Epic gum - both are widely available and proven effective.
- Avoid sugary drinks and acidic snacks. Even "healthy" options like fruit juice, dried fruit, and energy bars can wreck your teeth when saliva is low. Stick to whole fruits, nuts, cheese, and vegetables. If you drink coffee or tea, avoid adding sugar. Use a straw for anything sugary or acidic.
- See your dentist every 4-6 months. Most people go once a year. If you’re on furosemide, go every 4-6 months. Tell your dentist you’re taking it. They can check for early signs of enamel erosion and apply professional fluoride treatments or sealants.
What Your Dentist Can Do for You
Your dentist isn’t just there to fill cavities. They can help you prevent them - especially when you’re on diuretics.
Ask for:
- Professional fluoride varnish - applied every 3-6 months. It’s thicker than regular fluoride gel and sticks to teeth longer.
- Saliva-stimulating treatments - some clinics offer low-level laser therapy to boost saliva production.
- Custom mouthguards - if you grind your teeth at night (common with dry mouth), a guard can protect enamel from wear.
- Oral microbiome testing - newer clinics can test your saliva for harmful bacteria levels. If Streptococcus mutans is high, they can recommend targeted rinses or probiotics.
Don’t wait for pain. By the time you feel discomfort, damage is often already done. Early detection saves teeth - and money.
What Not to Do
There are common mistakes people make when they’re on furosemide:
- Drinking alcohol - it dehydrates you further and increases dry mouth.
- Using alcohol-based mouthwashes - they burn and dry out your gums. Look for alcohol-free options like Crest Pro-Health or Colgate Total.
- Skipping flossing - plaque builds up between teeth faster when saliva is low. Floss daily, even if your gums bleed.
- Assuming "no cavities" means you’re fine - enamel erosion and gum recession don’t always hurt. They show up on X-rays first.

When to Talk to Your Doctor
If your dry mouth is so bad you can’t sleep, swallow food, or speak without clearing your throat, talk to your doctor. They might:
- Adjust your furosemide dose
- Switch you to a different diuretic like hydrochlorothiazide (which causes less dry mouth in some people)
- Prescribe a saliva substitute like pilocarpine (Salagen) or cevimeline (Evoxac)
Never stop or change your medication without consulting your doctor. But do bring up your dental symptoms. Many doctors don’t know about this side effect - your feedback helps them help you better.
Real-Life Example: Linda’s Story
Linda, 68, from Durban, took furosemide for heart failure. She brushed twice a day and thought she was doing fine. After 14 months, she noticed her front teeth looked yellow and felt sensitive. Her dentist found three cavities, severe gum recession, and early enamel erosion. She hadn’t changed her diet or routine - but her saliva flow had dropped by 60%.
After switching to xylitol gum, using fluoride rinse nightly, and seeing her dentist every 4 months, her symptoms improved in 6 months. Her teeth stopped hurting. Her gums healed. She didn’t need fillings - just prevention.
She didn’t stop furosemide. She just learned how to protect her mouth while taking it.
Final Thought: Your Mouth Is Part of Your Whole Health
Furosemide helps you live longer. But if your teeth go bad, your quality of life drops fast. Eating becomes painful. Smiling feels embarrassing. You might avoid social situations. Your overall health suffers - because oral health and heart health are deeply linked.
People with gum disease have a higher risk of heart attacks and strokes. If you’re on a heart medication like furosemide, your mouth isn’t a separate issue - it’s part of your treatment plan.
Take care of your teeth like you take care of your blood pressure. With the right habits, you can keep your smile healthy - no matter what meds you’re on.
Does furosemide cause cavities directly?
No, furosemide doesn’t directly cause cavities. But it reduces saliva flow, which creates an environment where bacteria thrive and enamel breaks down faster. This makes cavities much more likely, even with good brushing habits.
Can I use mouthwash while taking furosemide?
Yes, but avoid mouthwashes with alcohol. They dry out your mouth further. Use alcohol-free, fluoride-containing rinses like Crest Pro-Health or Colgate Total. These help protect enamel without adding dehydration.
Should I stop taking furosemide if my mouth feels dry?
Never stop taking furosemide without talking to your doctor. It’s prescribed for serious conditions like heart failure and high blood pressure. Instead, focus on managing dry mouth with hydration, fluoride, and dental visits. Your doctor may adjust your dose or suggest alternatives if needed.
How often should I see the dentist if I’m on furosemide?
Every 4 to 6 months. Regular cleanings and fluoride treatments can prevent cavities and gum disease before they start. Most people only go once a year - but if you’re on diuretics, you need more frequent monitoring.
Are there alternatives to furosemide that are gentler on teeth?
Hydrochlorothiazide is another common diuretic that may cause less dry mouth in some patients. But it’s not always a better option - it depends on your condition. Talk to your doctor about whether switching is safe and appropriate for you. Never switch meds on your own.

Rekha Tiwari
October 28, 2025 AT 15:44Andy Smith
October 29, 2025 AT 11:36Leah Beazy
October 31, 2025 AT 06:30John Villamayor
October 31, 2025 AT 21:45Jenna Hobbs
November 1, 2025 AT 23:12Ophelia Q
November 2, 2025 AT 16:33