GERD and Acid Reflux: How PPIs and Lifestyle Changes Work Together
 Jan, 17 2026
Jan, 17 2026
What Exactly Is GERD?
GERD isn’t just occasional heartburn. It’s when stomach acid keeps flowing back into your esophagus-often enough to cause damage. This happens because the lower esophageal sphincter (LES), the muscle that acts like a door between your stomach and esophagus, doesn’t close right. Instead of staying shut, it lets acid escape. That acid burns the lining of your esophagus, which isn’t built to handle it. The result? A burning feeling in your chest, a sour taste in your mouth, or even a chronic cough.
Doctors define GERD when symptoms like heartburn or regurgitation happen at least twice a week. It’s not something you just live with. Left untreated, it can lead to serious problems like esophageal strictures, ulcers, or even Barrett’s esophagus-a condition that increases your risk of esophageal cancer. About 10-15% of people with long-term GERD develop Barrett’s. That’s why managing it properly matters.
Why Lifestyle Changes Are the First Step
Before reaching for a pill, the best thing you can do is change how you live. Studies show that losing just 5-10% of your body weight cuts GERD symptoms in half. If you’re carrying extra weight, especially around your belly, it puts pressure on your stomach and pushes acid upward. That’s why even small weight loss makes a big difference.
What you eat matters too. Coffee, tomatoes, alcohol, chocolate, and fatty or spicy foods trigger reflux in 70-80% of people with GERD. You don’t have to eliminate them forever, but cutting them out for a few weeks helps you see what’s really causing your symptoms. Keep a food diary. Write down what you eat and when symptoms hit. You might be surprised-maybe it’s not the spicy tacos, but the late-night ice cream.
Timing matters just as much as what you eat. Eating within two or three hours of bedtime is a major mistake. When you lie down, gravity stops helping keep acid in your stomach. Studies show avoiding food before sleep reduces nighttime acid exposure by 40-60%. Elevating the head of your bed by 6 inches helps too. It’s simple, cheap, and works better than many people expect.
How PPIs Actually Work
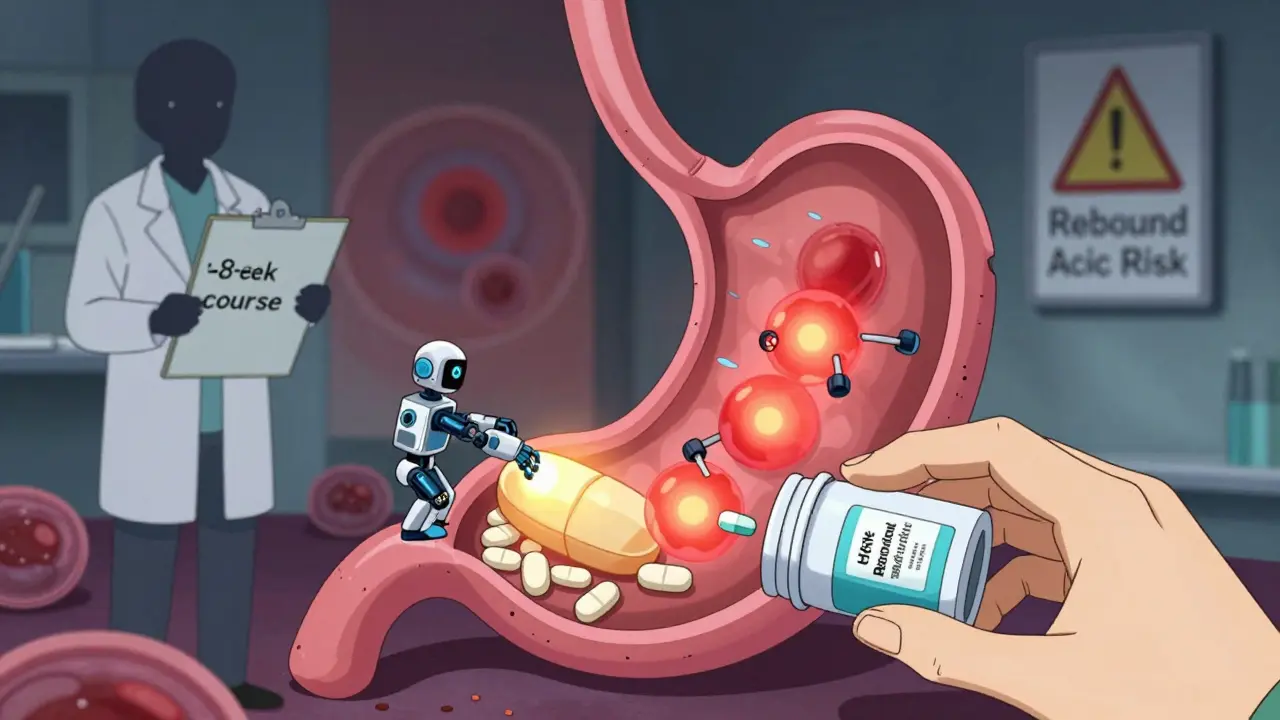
If lifestyle changes alone aren’t enough, proton pump inhibitors (PPIs) are the strongest medication available. Drugs like omeprazole (Prilosec), esomeprazole (Nexium), and pantoprazole (Protonix) stop your stomach from making acid at its source. They target the proton pumps in stomach cells-the final step in acid production. That means they reduce acid by 90-98%, far more than older drugs like H2 blockers (Pepcid, Tagamet), which only block about 60-70%.
PPIs are not quick fixes. They take 1-4 hours to start working and need to be taken 30-60 minutes before your first meal of the day. That’s because they work best when your stomach is preparing to produce acid. Taking them after you eat won’t help much. Most people take them once a day, but some with severe symptoms need twice-daily dosing.
They’re incredibly effective at healing damage. In clinical trials, 70-90% of people with erosive esophagitis saw their esophagus heal after 8 weeks on a PPI. That’s why doctors recommend them as first-line treatment for moderate to severe GERD or when there’s visible damage.
The Hidden Risks of Long-Term PPI Use
Just because PPIs work doesn’t mean you should take them forever. The FDA and major medical groups warn about risks tied to long-term use-especially beyond a year. Studies link prolonged PPI use to a 20-50% higher risk of intestinal infections like Clostridium difficile, vitamin B12 deficiency, and kidney problems like acute interstitial nephritis.
Older adults face another risk: bone fractures. Taking high-dose PPIs for three or more years increases hip fracture risk by 35%. That’s because reduced stomach acid affects calcium absorption. And here’s something many don’t know: stopping PPIs cold turkey can cause rebound acid hypersecretion. Your stomach overcompensates, making even more acid than before. Symptoms get worse-sometimes worse than they were originally. That’s why people think the drug stopped working, when really, they just stopped it too fast.
That’s why experts like Dr. David Johnson say you should regularly ask: Do I still need this? If your symptoms are under control, try stepping down. Switch to an H2 blocker like famotidine, or take the PPI only when you need it-on-demand dosing. Many people can cut their dose in half or skip days without symptoms returning.
Real People, Real Results
On Reddit’s r/GERD community, 72% of users said PPIs gave them major relief. But 68% also reported side effects-headaches, diarrhea, or low magnesium levels that caused muscle cramps. One woman stopped taking omeprazole after six months and developed severe heartburn. She thought it was her GERD coming back. It turned out to be rebound acid. She had to slowly taper off with the help of her doctor, using Pepcid for a few weeks while reducing the PPI dose.
On the flip side, people who stuck with lifestyle changes saw real wins. In a 2022 survey, 58% of users who eliminated trigger foods and stopped eating before bed reported moderate to complete symptom control. One man in Ohio cut out coffee, alcohol, and late-night snacks. He lost 12 pounds. Within three months, he was off his PPI. He still eats pizza once a month-but never after 7 p.m.
There are failures too. A 55-year-old patient in Wisconsin developed Barrett’s esophagus despite taking PPIs daily. Why? He kept eating dinner at 10 p.m. and lying down right after. Medication can’t fix bad habits.
What’s New in GERD Treatment
There’s a shift happening. In 2023, the FDA approved Vonoprazan (Voquezna), the first new acid-blocking drug class in 30 years. It works faster than PPIs and may be more effective for some people. Early studies show 89% healing rates in erosive esophagitis-slightly better than PPIs.
Also, new guidelines from the American Gastroenterological Association (January 2024) now say lifestyle changes should be the foundation of treatment-not just an add-on. PPIs should be reserved for confirmed esophageal damage or severe symptoms.
At Johns Hopkins, a 12-week program combining diet, sleep hygiene, and stress reduction helped 65% of patients stop PPIs completely without symptom return. That’s more than double the success rate of standard care.
Apps like RefluxMD are helping people track triggers with more precision. AI tools are learning individual patterns-like how one person reacts to wine but not beer, or how stress triggers reflux even without food. These tools are making management more personal.
When to Consider Surgery
Most people don’t need surgery. But if you’ve tried lifestyle changes and medications, and you’re still struggling, it’s worth talking about. Fundoplication-a surgery that wraps the top of the stomach around the esophagus-has a 90% success rate at 10 years. The LINX® device, a tiny ring of magnetic beads placed around the LES, helps it stay closed but still opens for swallowing. About 85% of users report major symptom reduction after five years.
Less invasive options like transoral incisionless fundoplication (TIF) are also gaining traction. Patients report better quality of life than with ongoing PPI use. These aren’t magic fixes, but for some, they’re life-changing.
What You Should Do Now
Start here: track your symptoms for two weeks. Note what you eat, when you eat, and when symptoms happen. Cut out the top three triggers: coffee, alcohol, and late-night meals. Try elevating your bed. Aim to lose 5% of your body weight if you’re overweight.
If symptoms persist, talk to your doctor about a short course of a PPI-no longer than 8 weeks. Then reevaluate. Don’t just refill the prescription. Ask: Can I try H2 blockers? Can I take it only when I need it? Can I get off it entirely?
GERD isn’t a life sentence. It’s a condition you manage. The right mix of simple habits and smart medication can get you back to living without constant discomfort.
Can I stop taking PPIs cold turkey?
No. Stopping PPIs suddenly can cause rebound acid hypersecretion, where your stomach makes even more acid than before. This leads to worse heartburn and can make you think the medication stopped working. Instead, work with your doctor to taper off slowly-usually over 4-8 weeks-while using an H2 blocker like famotidine to manage symptoms during the process.
Are PPIs safe for long-term use?
PPIs are very effective, but long-term use (over a year) carries risks. Studies link them to higher chances of intestinal infections, vitamin B12 deficiency, kidney problems, and bone fractures in older adults. The FDA recommends using the lowest dose for the shortest time needed. Regularly review your need for PPIs with your doctor-don’t just keep taking them because "it’s what you’ve always done."
Will losing weight help my GERD?
Yes. Losing just 5-10% of your body weight can reduce GERD symptoms by up to 50%. Extra belly fat puts pressure on your stomach, pushing acid upward. Weight loss reduces that pressure and often improves LES function. Even small, consistent changes-like walking 30 minutes a day and cutting sugary drinks-can make a big difference over time.
What foods should I avoid with GERD?
Common triggers include coffee, tomatoes, alcohol, chocolate, fatty or fried foods, spicy foods, citrus, and carbonated drinks. But triggers vary by person. Keep a food diary for two weeks to find your personal triggers. Eliminate the top three for 3-4 weeks, then reintroduce them one at a time to see what causes symptoms.
Is heartburn relief the same as healing?
No. Feeling better doesn’t mean your esophagus is healed. PPIs can stop symptoms quickly, but inflammation may still be present. That’s why doctors recommend a full 8-week course-even if you feel fine after two weeks. Skipping the full course increases your risk of complications like strictures or Barrett’s esophagus.
Can I manage GERD without medication?
Yes, for many people. Lifestyle changes alone-weight loss, avoiding trigger foods, not eating before bed, and elevating the head of your bed-can control symptoms in over half of patients. Some people never need medication. Others use it temporarily while building better habits. The goal isn’t to rely on pills forever-it’s to reduce dependence over time.
