Goiter: Understanding Thyroid Enlargement and the Role of Iodine Supplementation
 Nov, 17 2025
Nov, 17 2025
A goiter isn’t just a lump in the neck-it’s a sign your thyroid is struggling. The thyroid, a small butterfly-shaped gland at the base of your throat, works nonstop to regulate your metabolism, energy, and body temperature. When it swells, it’s trying to compensate for something missing-or something going wrong inside. For millions around the world, that missing piece is iodine.
What Causes a Goiter?
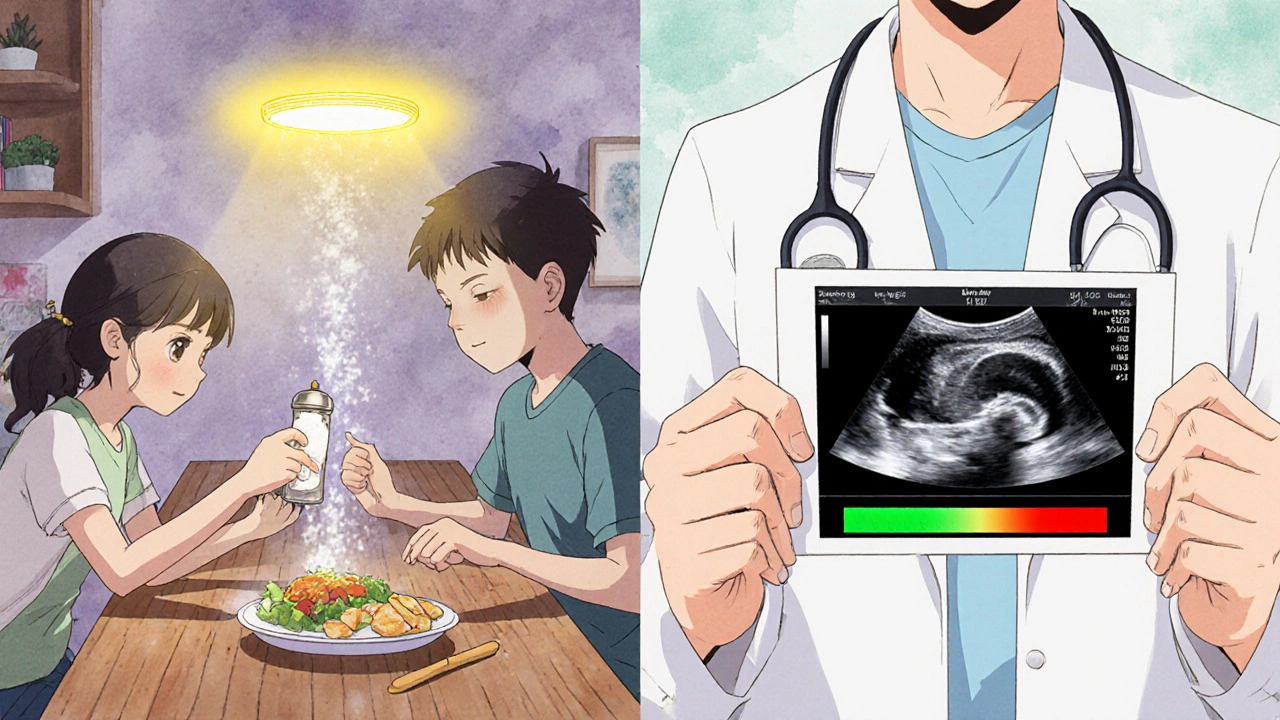
The most common cause of goiter worldwide? Not genetics. Not stress. Not toxins. It’s iodine deficiency. In places without access to iodized salt, up to 90% of goiter cases come from not getting enough iodine in the diet. The thyroid needs iodine to make thyroid hormones. Without it, the gland grows bigger, trying to trap every bit of iodine it can find. That’s why, in parts of Africa, South Asia, and even some remote mountain regions, goiters were once so common they became part of everyday life.
In the U.S. and other countries that have used iodized salt since the 1920s, the story changes. Here, autoimmune diseases are the main culprits. Hashimoto’s thyroiditis-the body attacking its own thyroid-is the number one cause. The immune system slowly destroys thyroid tissue, and the gland swells in response. Another cause is Graves’ disease, where the thyroid goes into overdrive, producing too much hormone and growing larger as a result.
Age and gender matter too. Women are three times more likely than men to develop a goiter. After age 40, the risk climbs. That’s not because of diet alone-it’s hormonal shifts, immune changes, and decades of accumulated stress on the gland.
How Big Is Too Big?
A healthy thyroid weighs about 15 to 20 grams-roughly the size of a walnut. When it hits 50 grams or more, you’re looking at a goiter. Ultrasound can measure it more precisely: anything over 25 mL is considered abnormal. In severe cases, the gland can swell to the size of a lemon or even bigger.
That growth doesn’t just look strange-it can press on your windpipe, esophagus, or vocal cords. People with large goiters often report trouble swallowing food, especially bread or meat. Some notice their voice gets hoarse. Others feel like they can’t take a full breath, especially when lying down. These aren’t rare side effects. They’re warning signs that the goiter has outgrown its space.
Iodine Supplementation: The Simple Fix for Many
If your goiter is from iodine deficiency, the fix is surprisingly straightforward: take iodine. The recommended daily dose for adults is 150 micrograms (mcg). Pregnant women need 220 mcg. Breastfeeding moms need 290 mcg. That’s not a lot-about the amount in one teaspoon of iodized salt.
Studies show that taking 150 mcg of iodine daily for 6 to 12 months reduces thyroid size by 30 to 40% in most cases. In 70 to 85% of people with simple iodine-deficient goiters, the swelling disappears completely within two years. No surgery. No drugs. Just a daily supplement.
Iodized salt is the most common public health tool. In the U.S., each gram of iodized salt contains about 45 mcg of iodine. That means a quarter teaspoon gives you nearly the full daily need. But not everyone uses it. Some people switch to sea salt, Himalayan salt, or kosher salt-none of which are iodized. Others avoid salt entirely for health reasons. That’s where supplements come in.
Potassium iodide tablets, available over the counter or by prescription, deliver the right dose without the sodium. For children in high-risk areas, doses of 90-150 mcg daily are standard. For adults, 150-250 mcg. Pregnant women are often given higher doses under medical supervision.
When Iodine Doesn’t Help
But here’s the catch: iodine won’t fix everything. If your goiter is from Hashimoto’s or Graves’ disease, extra iodine won’t shrink it-and in some cases, it can make things worse. In Hashimoto’s, the immune system is already attacking the thyroid. Adding iodine can sometimes trigger more inflammation. In Graves’ disease, iodine can fuel overproduction of thyroid hormone, making hyperthyroidism worse.
For Hashimoto’s-related goiters, the treatment is levothyroxine-a synthetic thyroid hormone. It replaces what the gland can’t make anymore. It also tells the brain to stop signaling the thyroid to grow. The result? A 10 to 20% reduction in size, not because the gland shrinks dramatically, but because the swelling from immune activity calms down. But if the gland has been damaged for years, it turns fibrous. That’s scar tissue. And scar tissue doesn’t shrink.
For Graves’ disease, doctors use antithyroid drugs like methimazole. These block hormone production. Over 12 to 18 months, the goiter shrinks by 40 to 60%. But even then, the gland doesn’t return to normal size. That’s why some people eventually need radioactive iodine or surgery.
Surgery and Radioactive Iodine: When to Consider Them
When a goiter grows too large-usually over 80 to 100 mL-or starts pressing on vital structures, doctors recommend intervention. Surgery (thyroidectomy) removes part or all of the gland. On average, surgeons remove 30 to 40 grams of tissue. It’s effective, but not without risks. About 15% of patients experience voice changes because the nerves near the thyroid get irritated. About 8% develop low calcium levels because the parathyroid glands, which sit behind the thyroid, get affected.
Radioactive iodine is another option, especially for toxic goiters caused by Graves’ disease. You swallow a capsule. The radiation targets only the thyroid. Within 6 to 12 months, the gland shrinks by 50 to 60%. But here’s the trade-off: 75 to 80% of people end up with permanent hypothyroidism. That means taking levothyroxine for the rest of your life.
Patients report high satisfaction with iodine supplements for deficiency-related goiters-78% say it worked well. But only 42% are happy with surgical outcomes, mostly because of voice changes and the need for lifelong hormone therapy.

What About Selenium?
You might have heard selenium helps with thyroid health. It’s true that selenium is involved in thyroid hormone metabolism. Some studies suggest it might reduce thyroid antibodies in Hashimoto’s patients. But a major 2021 Cochrane Review looked at 11 clinical trials and found no clear benefit for reducing goiter size. The odds of improvement were almost the same with or without selenium. The European Thyroid Association says it might help in specific autoimmune cases, but it’s not a standard treatment. Don’t waste money on selenium supplements unless your doctor confirms a deficiency.
What’s New in Research?
Scientists are now looking beyond iodine and autoimmunity. The NIH-funded TRIPOD study, tracking 5,000 people across 10 countries, has identified 37 genetic locations linked to thyroid size. That means some people are born with a tendency to develop goiters-even with enough iodine. This could lead to personalized screening in the future.
Regulations are catching up too. In 2022, the FDA required all salt products sold in the U.S. to list iodine content on the label. That’s a big step. People need to know what’s in their salt. The European Medicines Agency also updated its guidelines in 2023 to standardize radioactive iodine doses, making treatment safer and more predictable.
What Should You Do?
If you notice a swelling in your neck, don’t ignore it. See a doctor. Get a blood test for TSH, free T4, and thyroid antibodies. An ultrasound will show the size and structure of the gland. If iodine levels are low, supplementation can work wonders. If it’s autoimmune, medication can manage it. If it’s huge and pressing on your airway, surgery may be necessary.
Don’t self-treat with iodine pills unless you know you’re deficient. Too much iodine can cause its own problems-hyperthyroidism, thyroiditis, or even trigger a goiter in people with underlying conditions.
Check your salt. If you’re using sea salt, Himalayan salt, or kosher salt, you’re likely missing iodine. Switch to iodized table salt-or take a daily 150 mcg supplement. For pregnant women, that’s not optional. It’s critical for the baby’s brain development.
Goiter isn’t a death sentence. It’s not even rare. But it’s a signal. Listen to your body. Get tested. Treat the cause-not just the bump.
Can iodine supplementation shrink a goiter?
Yes-if the goiter is caused by iodine deficiency. Taking 150 mcg of iodine daily for 6 to 12 months typically reduces thyroid size by 30 to 40%. In 70 to 85% of cases, the swelling resolves completely within two years. But iodine won’t help if the goiter is from Hashimoto’s, Graves’ disease, or other autoimmune causes.
Is iodized salt enough to prevent goiter?
For most people, yes. One gram of iodized salt contains about 45 mcg of iodine. A half-teaspoon provides nearly the full daily requirement of 150 mcg. But if you avoid salt, use non-iodized salt, or follow a strict low-sodium diet, you may need a supplement. Pregnant and breastfeeding women should always take an iodine supplement unless their doctor advises otherwise.
Can too much iodine cause a goiter?
Yes. While iodine deficiency is the most common cause, too much iodine can also trigger thyroid enlargement-especially in people with underlying thyroid conditions like Hashimoto’s or nodules. This is called the Jod-Basedow phenomenon. It’s rare, but it happens. That’s why you shouldn’t take iodine supplements without testing your levels first.
Does selenium help reduce goiter size?
Not reliably. A 2021 Cochrane Review of 11 studies found no significant benefit from selenium supplementation in reducing goiter size. While selenium supports thyroid hormone production, it doesn’t shrink the gland. Some European guidelines suggest it might help lower antibodies in Hashimoto’s, but it’s not a standard treatment for goiter.
When is surgery needed for a goiter?
Surgery is recommended when the goiter is larger than 80-100 mL, causes trouble breathing or swallowing, or compresses the voice box. It’s also considered if the goiter grows rapidly or if there’s suspicion of cancer. About 15% of patients experience voice changes after surgery, and 8% develop low calcium levels. It’s effective but carries risks.
Can a goiter come back after treatment?
Yes. If the underlying cause isn’t addressed, it can return. If you stop iodine supplements after a deficiency-related goiter, the swelling may come back. In autoimmune cases, even with medication, the thyroid can continue to change over time. Long-term monitoring with blood tests and ultrasounds is key, especially for people with Hashimoto’s or Graves’ disease.
Are goiters dangerous?
Most goiters aren’t cancerous. But they can become dangerous if they grow large enough to block your airway or esophagus. A sudden increase in size, pain, or voice changes should be checked immediately. Also, goiters linked to Graves’ disease or Hashimoto’s can lead to serious hormone imbalances-hyperthyroidism or hypothyroidism-which affect your heart, energy, mood, and metabolism.

Riohlo (Or Rio) Marie
November 18, 2025 AT 10:00Oh sweet mercy, another ‘iodine is the panacea’ post. Darling, if you think a teaspoon of salt fixes autoimmune thyroid chaos, you’ve been reading wellness blogs written by people who think ‘detox’ is a verb. The thyroid isn’t a clogged drain-it’s a biological orchestra conductor that’s been screaming for decades. Iodine? Cute. But if your immune system’s already staging a coup, you’re not fixing it with sea salt and optimism. You need a damn immunologist, not a TikTok nutritionist.
Conor McNamara
November 19, 2025 AT 23:45wait so iodized salt is a gov mind control thing? i heard the chemtrails are in the salt too. they dont want us to be healthy so we stay docile. also my neighbor said the thyroid is just a portal to the 5th dimension and when it swells its because aliens are trying to communicate. i dont trust any of this science. they took my cat's microchip last tuesday.
steffi walsh
November 20, 2025 AT 23:45Y’all need to stop panicking and just get tested!! 😊 I had a tiny goiter last year and it was just low iodine-started taking a 150mcg pill and boom, 3 months later it was gone. No drama, no surgery, just a little care. You’re not broken, you’re just missing a tiny nutrient. Seriously, if you’re tired all the time or feel like your throat’s full of cotton, go see a doc. It’s not scary, I promise 💪❤️
Leilani O'Neill
November 22, 2025 AT 21:24Of course Americans think iodized salt is a solution. You don’t even know what real food is. In my village in County Clare, we ate seaweed with every meal since the 1800s. No pills. No lab-made salts. Just the ocean. Now you import salt from China and call it ‘iodized’ like it’s some miracle. Your thyroid is weak because you eat processed garbage and then think a supplement fixes your cultural decay. Grow up.
Sarah Frey
November 23, 2025 AT 16:31Thank you for this comprehensive and clinically grounded overview. The distinction between iodine-deficient goiter and autoimmune etiologies is critical, and too many patients self-prescribe iodine without understanding the potential for iatrogenic harm. The data on levothyroxine’s impact on gland size in Hashimoto’s, while modest, is consistent with decades of endocrinological practice. I would emphasize that even in cases of deficiency, supplementation should be monitored via TSH and urinary iodine levels to avoid excess. Precision medicine is not a buzzword-it’s a necessity here.
Katelyn Sykes
November 24, 2025 AT 15:37Just got my ultrasound back and my thyroid is 48 grams so yeah its definitely a goiter but my doc said its Hashimoto's so iodine is a no go. I was so mad I wasted 3 months taking those pills. Now I'm on levothyroxine and honestly my energy is way better. Also I switched to iodized salt just in case but I don't think it's doing much. Just wanted to say don't trust random internet advice like I did lol
Yash Nair
November 25, 2025 AT 16:14India has been using iodized salt since 1983 and we still have goiters so your american solution is bullshit. Our women eat sea salt from the coast and still have babies with low IQ because your so called fix doesn't work. You think a pill solves centuries of malnutrition? You don't know what poverty is. Stop preaching like you saved the world with your fancy lab salt.
Bailey Sheppard
November 26, 2025 AT 21:36Really appreciate this breakdown. I had a goiter back in college and thought it was just stress-turned out it was mild Hashimoto’s. Took me two years to get diagnosed because I was too scared to see a doctor. If you’re reading this and you’ve got a lump in your neck, just go. It’s not a big deal to get bloodwork done. I’m doing fine now, on meds, and I even started hiking again. You’re not alone.
Girish Pai
November 28, 2025 AT 17:07Let’s contextualize the epidemiological burden. In endemic iodine-deficient zones, the goiter prevalence rate exceeds 20% in school-aged children. The WHO recommends universal salt iodization (USI) as a cost-effective public health intervention with a cost-benefit ratio of 1:27. However, in autoimmune-dominant populations, the pathophysiological paradigm shifts from nutrient deficiency to molecular mimicry and epitope spreading. The therapeutic algorithm must therefore be stratified. Iodine supplementation in Graves’ disease constitutes a contraindication due to the Wolff-Chaikoff effect and subsequent escape phenomenon.
Kristi Joy
November 29, 2025 AT 00:23Hey, if you’re reading this and you’re scared about your thyroid, I get it. I’ve been there. But you’re not failing because you have a goiter-you’re just human. Your body is trying to tell you something. Whether it’s iodine, stress, or genetics, there’s help. Talk to your doctor. Ask questions. Don’t let fear silence you. You deserve to feel like yourself again. And if you need someone to walk through the next steps with you, I’m here. You’ve got this.
Hal Nicholas
November 29, 2025 AT 13:53They don’t want you to know the truth. The FDA knew about iodine’s risks since 1978 but pushed it anyway because Big Pharma makes more money selling levothyroxine. The real cure? Detox your liver, eat seaweed, and stop using plastic containers. Also, the thyroid is connected to your chakras. If you’re not meditating, no supplement will help. I’ve seen 30 people cure their goiters with just breathwork and crystal healing. Science is just a belief system anyway.
Louie Amour
November 29, 2025 AT 18:56You people are pathetic. You think a 150 mcg pill fixes decades of poor lifestyle choices? You eat gluten, drink soda, sit on your ass all day, and then blame your thyroid? I’ve seen 12-year-olds in rural China with zero goiters because they eat fish, rice, and walk five miles to school. Your problem isn’t iodine. It’s weakness. Get off your phone. Lift something. Eat real food. Stop looking for magic pills. Your body isn’t broken-it’s lazy.