H2 Blockers and PPIs: When Combining Acid Medications Does More Harm Than Good
 Nov, 14 2025
Nov, 14 2025
Acid Medication Combination Checker
Is Your Combination Therapy Necessary?
Based on current medical guidelines, combination therapy (H2 blocker + PPI) is rarely recommended. This tool helps you assess if you should discuss stopping one of your medications with your doctor.
Most people think taking two stomach meds together means better relief. But when it comes to H2 blockers and PPIs, combining them often does more harm than good. These drugs are meant to calm stomach acid, but using them at the same time isn’t just unnecessary-it’s risky. In hospitals and clinics across the U.S., doctors still prescribe both drugs together, even though studies show little to no extra benefit-and a lot more side effects.
How H2 Blockers and PPIs Actually Work
H2 blockers like famotidine (Pepcid) and cimetidine (Tagamet) work by blocking histamine, a chemical that tells your stomach to make acid. They start working within an hour and last 6 to 12 hours. That’s why some people take them before bed-to stop nighttime heartburn.
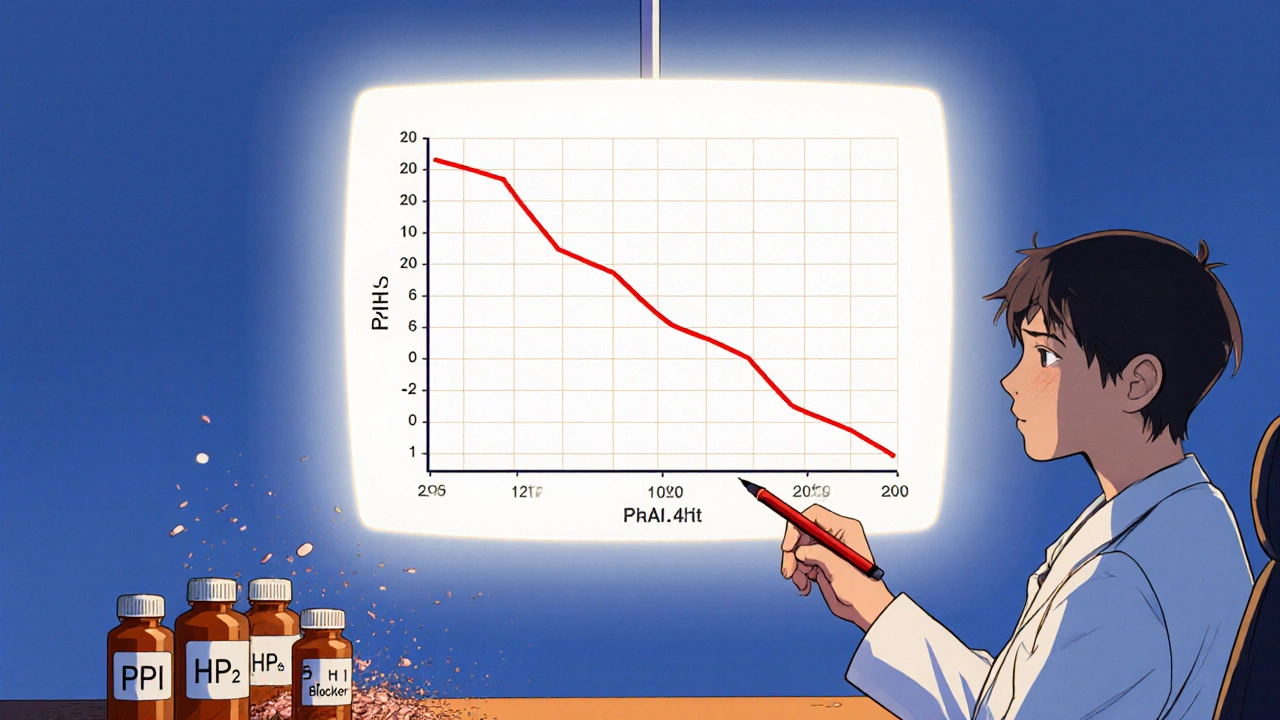
PPIs like omeprazole (Prilosec) and esomeprazole (Nexium) go deeper. They shut down the actual acid pumps in your stomach cells. But they don’t work right away. It takes 2 to 5 days for them to reach full power. Once they do, they suppress acid by 90% or more, all day long.
Here’s the catch: PPIs make histamine almost useless. If your stomach isn’t making acid, then blocking histamine doesn’t matter much. That’s why adding an H2 blocker to a PPI often does almost nothing extra. One study found that adding ranitidine to omeprazole only reduced nighttime acid by 5%. Not enough to notice. Not enough to justify the risk.
Why Doctors Still Prescribe Both
It’s not because the science supports it. It’s because old habits die hard. Years ago, doctors thought combining the two would give faster, stronger relief. Some still believe it helps with severe GERD or nighttime symptoms. But modern guidelines say otherwise.
The American College of Gastroenterology reviewed 12 clinical trials with nearly 3,000 patients. Their 2022 report was clear: "Long-term combination therapy offers no additional benefit for GERD." The American Gastroenterological Association went further, calling routine dual therapy "unjustified" due to cost, complexity, and side effects.
Still, about 15-20% of hospitalized patients get both drugs. That’s over 1.2 million people a year in the U.S. alone. And it’s costing the system $1.5 billion annually. Why? Because many patients are started on both drugs in the ER or ICU, and no one ever stops one.
The Hidden Dangers of Stacking Acid Drugs
More acid suppression doesn’t mean better outcomes. It means more risks.
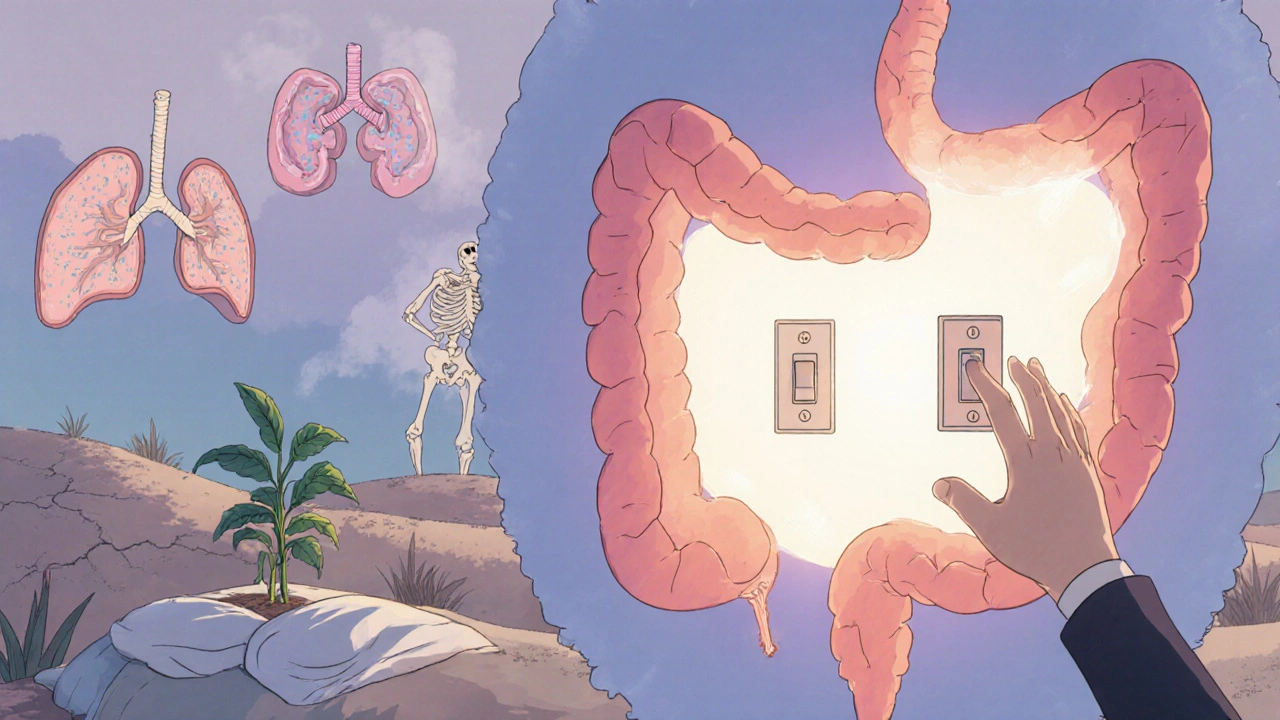
A 2014 study of nearly 80,000 ICU patients found that those on PPIs had a 30% higher chance of getting hospital-acquired pneumonia than those on H2 blockers. Why? Stomach acid kills bacteria. When you turn it off, bacteria can creep up into your lungs.
PPIs also raise the risk of Clostridium difficile infections by 32%. That’s a nasty gut bug that causes severe diarrhea and can be life-threatening in older adults. H2 blockers don’t carry the same level of risk.
And it gets worse. A 2021 study of over 3,600 people with chronic kidney disease found that those taking PPIs were 28% more likely to progress to kidney failure than those on H2 blockers. This isn’t a small concern. Kidney damage from long-term PPI use is real-and often silent until it’s advanced.
Even stranger, PPIs were linked to a 22% higher risk of gastrointestinal bleeding compared to H2 blockers. That’s the opposite of what you’d expect. More acid suppression should protect the stomach, right? Not always. The body adapts. The lining changes. The balance shifts. And sometimes, it backfires.
What Patients Are Really Experiencing
Patients aren’t just following doctor orders-they’re living with the consequences.
On Drugs.com, 68% of people who took PPIs reported side effects: headaches, diarrhea, bloating, and vitamin deficiencies. Low B12, low magnesium, low calcium-these aren’t rare. They’re common. And they show up slowly. You might not notice until you’re dizzy, weak, or getting bone fractures.
On Reddit’s r/GERD community, 42% of users say they can’t stop PPIs. They get rebound heartburn when they try. That’s not addiction-it’s physiology. Your stomach ramps up acid production to compensate for the suppression. When you stop, it overcompensates. It feels like the drug stopped working. But really, your body just got used to it.
A survey by the American College of Gastroenterology found that 31% of patients on both drugs didn’t even know why they were taking them. And 64% couldn’t name a single side effect. That’s not informed consent. That’s passive medication use.
When Is Combining Them Actually Okay?
There’s one scenario where it might make sense: documented nocturnal acid breakthrough.
This means you’re on a full dose of PPI-usually twice daily-but your stomach pH still drops below 4 for more than an hour between midnight and 6 a.m. That’s when acid starts damaging your esophagus. If you’re waking up with heartburn despite taking your PPI, this could be the issue.
But here’s the catch: you need to prove it. That means a 24-hour pH monitoring test. Most doctors don’t order it. They just add an H2 blocker at bedtime and hope for the best.
If you’re on both drugs, ask: Has my acid been measured? Is there proof I need both? If not, you’re likely taking an unnecessary pill.
What You Should Do Instead
Start with the lowest effective dose of a PPI. For most people, once daily is enough. For mild symptoms, H2 blockers alone may be all you need.
Try lifestyle changes first: avoid late meals, cut back on caffeine and alcohol, lose weight if needed, and elevate the head of your bed. These work better than most people think.
If you’re on both drugs, ask your doctor for a "PPI time-out." The VA recommends stopping PPIs every 90 days to see if you still need them. Do the same with the H2 blocker. Cut it out for two weeks. See if symptoms come back. If they don’t, you’ve just saved yourself from months of unnecessary medication.
Don’t stop cold turkey if you’ve been on PPIs for years. Gradual tapering helps avoid rebound acid. Talk to your doctor about a plan.
The Bigger Picture
Acid-suppressing drugs are among the most overused medications in medicine. The U.S. spends $12.3 billion a year on them. PPIs make up 78% of prescriptions. But studies show that up to 70% of PPI prescriptions are inappropriate.
Now, adding an H2 blocker on top? That’s doubling down on a problem. The American Gastroenterological Association added "Don’t prescribe combination therapy for routine GERD" to its Choosing Wisely list in 2023. Medicare is now tracking hospitals that overprescribe this combo. Starting in 2024, hospitals with more than 15% inappropriate dual therapy could lose money.
It’s not about saving a few dollars. It’s about protecting your body from harm. Your stomach needs some acid. Your lungs need it kept down. Your kidneys need it balanced. Too much suppression isn’t safety-it’s a slow leak in your health.
Final Takeaway
Combining H2 blockers and PPIs is rarely the answer. For most people, one drug is enough. For most cases, even one isn’t needed. The real fix isn’t another pill-it’s reassessing why you’re taking it in the first place.
If you’re on both, ask your doctor: Is there proof I need this? What are the risks? Can we try stopping one? You don’t need to suffer through side effects because someone forgot to review your meds.
Can I take an H2 blocker and PPI together safely?
Only in rare cases, like documented nighttime acid breakthrough despite full-dose PPI therapy. Even then, it should be temporary-no longer than 4 to 8 weeks-and only after confirming the issue with pH monitoring. For most people, it’s unnecessary and risky.
Do H2 blockers have fewer side effects than PPIs?
Yes. H2 blockers like famotidine carry a lower risk of pneumonia, C. diff infections, kidney damage, and bone fractures compared to PPIs. They also don’t cause rebound acid as severely. For long-term use, H2 blockers are often safer, especially for older adults or those with kidney disease.
Why do I get heartburn when I stop my PPI?
Your stomach produces more acid to compensate for the suppression. When you stop the PPI, that extra acid surges back. This isn’t addiction-it’s a physiological rebound. Tapering slowly and using lifestyle changes can help manage it. An H2 blocker can be used short-term during tapering, but not as a long-term fix.
Are there natural alternatives to acid-suppressing drugs?
Yes. Avoid eating 3 hours before bed, reduce caffeine and spicy foods, lose excess weight, stop smoking, and elevate your head while sleeping. Many people find these changes eliminate symptoms without medication. For mild cases, they’re more effective than drugs.
How do I know if I’m on too many acid meds?
If you’ve been on a PPI for more than 3 months without a clear diagnosis (like ulcers or Barrett’s esophagus), you’re likely on it longer than needed. If you’re on both a PPI and H2 blocker, you’re almost certainly over-treated. Ask your doctor for a medication review. You may not need either.

Nicole Carpentier
November 15, 2025 AT 13:40Eric Pelletier
November 15, 2025 AT 17:32Hadrian D'Souza
November 16, 2025 AT 22:32Robert Spiece
November 18, 2025 AT 11:41Agha Nugraha
November 20, 2025 AT 00:53Rekha Tiwari
November 20, 2025 AT 20:28Marshall Pope
November 22, 2025 AT 10:34Howard Lee
November 24, 2025 AT 00:13Nonie Rebollido
November 24, 2025 AT 12:41Andy Smith
November 24, 2025 AT 21:45Vivian Quinones
November 25, 2025 AT 10:31Abhay Chitnis
November 27, 2025 AT 01:11Leah Beazy
November 27, 2025 AT 05:42Brandon Benzi
November 27, 2025 AT 06:07