Heart Failure Management: From Diagnosis to Living Well
 Nov, 16 2025
Nov, 16 2025
Heart failure isn’t a single event-it’s a journey
You might hear someone say, "I was diagnosed with heart failure," and think it means the end. But that’s not true. Heart failure is a condition that can be managed, slowed, and sometimes even reversed-if you know what to do and when to do it. The latest guidelines from the American Heart Association and American College of Cardiology (2023) have completely changed how we treat it. No longer is it just about pills for swelling or oxygen tanks. Today, we have treatments that don’t just ease symptoms-they save lives.
Understanding the stages: Are you at risk, or already in trouble?
Heart failure doesn’t show up overnight. It builds over time, and doctors now divide it into four clear stages:
- Stage A: You’re at risk-maybe you have high blood pressure, diabetes, or a family history-but your heart still looks normal on tests.
- Stage B: Your heart has structural damage-a past heart attack, thickened walls, or a leaky valve-but you still feel fine. No shortness of breath, no swelling.
- Stage C: Now you have symptoms. Getting tired fast, swelling in your legs, needing extra pillows to sleep. This is where most people get diagnosed.
- Stage D: Your heart is severely weakened. Even at rest, you’re breathless. You may need a device, a transplant, or comfort-focused care.
Knowing your stage isn’t just a label. It tells your doctor exactly what treatments you need. Someone in Stage B might only need an ACE inhibitor. Someone in Stage C? They need a full combo-four medicines, all working together.
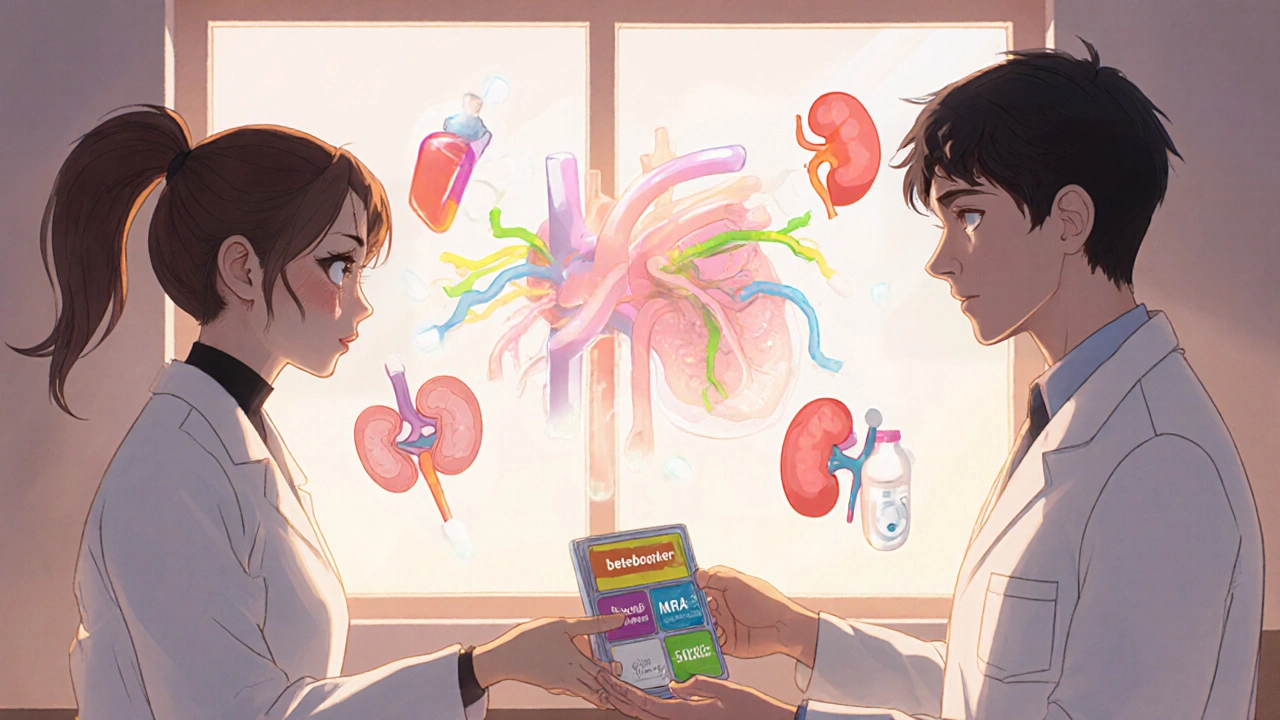
The four-pillar treatment for HFrEF: What works now
If your heart’s pumping ability is low (ejection fraction ≤40%), you have HFrEF. For this type, the 2023 guidelines say you need four key medicines, taken together:
- ARNI (sacubitril/valsartan): This replaces older ACE inhibitors for most people. It’s more effective at lowering death and hospitalization rates. The number needed to treat to save one life over three years? Just 12 people.
- Heart failure beta-blockers: Not just any beta-blocker. You need carvedilol, metoprolol succinate, or bisoprolol. These are the only ones proven to help in heart failure. They slow your heart, reduce strain, and can even help your heart heal.
- Mineralocorticoid receptor antagonist (MRA): Spironolactone or eplerenone. These block hormones that make your body hold onto salt and fluid. They reduce hospital stays by nearly 30%.
- SGLT2 inhibitors: Originally for diabetes, now a cornerstone of heart failure care. Dapagliflozin and empagliflozin cut hospitalizations and death-even if you don’t have diabetes. They work by helping your kidneys flush out extra sugar and salt.
This quadruple therapy isn’t optional anymore. It’s the standard. And the benefits are real: people on all four drugs live longer, feel better, and end up in the hospital far less often.
HFpEF: The forgotten type that finally has hope
For years, doctors had almost nothing to offer if your heart’s pumping normally (ejection fraction ≥50%). That’s HFpEF. It’s more common in older adults, especially women, and often linked to high blood pressure, obesity, or diabetes. Until 2020, the main treatment was diuretics-water pills-to reduce swelling.
Then came the breakthroughs. The EMPEROR-PRESERVED and DELIVER trials showed that SGLT2 inhibitors-same ones used in HFrEF-cut hospitalizations by 18-21%. That’s not a cure, but it’s the first real drug therapy that works for HFpEF. Today, guidelines say: if you have HFpEF, start an SGLT2 inhibitor. No waiting. No second-guessing.
One patient in Durban, 72, with HFpEF and type 2 diabetes, started empagliflozin. Within three months, her 6-minute walk distance went from 320 meters to 410. She hasn’t been hospitalized in 18 months. That’s the power of this new approach.
Monitoring your heart at home: The CardioMEMS difference
What if you could know your heart is failing before you feel it? That’s what the CardioMEMS device does. It’s a tiny sensor placed in your pulmonary artery during a short procedure. It sends daily pressure readings to your doctor. High pressure? That’s a warning sign-fluid is building up before you’re swollen or breathless.
The 2025 MONITOR-HF trial confirmed what earlier studies hinted at: patients with CardioMEMS had 28% fewer hospitalizations and reported much better quality of life. You don’t need to guess how much fluid to cut back. Your doctor sees the data, adjusts your meds, and you stay out of the ER.
It’s not for everyone. It’s expensive-around $20,000 for the device plus quarterly monitoring. But for people who keep ending up in the hospital, it’s life-changing.
Why so many people aren’t getting the right treatment
Here’s the hard truth: even though we have better treatments than ever, most people aren’t getting them. A 2024 study found only 38.7% of eligible HFrEF patients were on all four recommended drugs within a year of diagnosis. Why?
- Doctors are afraid of low blood pressure. Many think giving all four drugs will make patients dizzy or faint. But real-world data shows only 1.8% of heart failure patients have truly dangerous low BP. Clinicians overestimate this risk by five times.
- Too many pills. The average HFrEF patient takes 7.3 medications daily. Add in diabetes, kidney disease, or arthritis meds, and it’s overwhelming. One caregiver on HeartFailureMatters.org said, "My husband forgets which pill is which. I have to sort them into daily boxes."
- Knowledge gaps. Not all providers know the latest guidelines. Especially in smaller clinics or rural areas.
The ACC’s "HF in a Box" toolkit helps. It gives doctors checklists, patient handouts in 17 languages, and step-by-step titration plans. Clinics using it saw a 27% jump in quadruple therapy use in just six months.
What about side effects? Can you really take all these pills?
Yes-but you need to do it right.
Each medicine has potential side effects:
- ARNI can cause swelling in the face (angioedema)-rare, but serious. Stop it immediately if you notice this.
- MRAs can raise potassium. Your doctor will check your blood levels every few weeks.
- SGLT2 inhibitors can cause yeast infections or dehydration. Drink water. Don’t skip meals.
But here’s what matters: the benefits outweigh the risks. For every 25 people treated with an SGLT2 inhibitor, one hospitalization is prevented in two years. For every 12 on ARNI, one death is avoided over three years.
Start low. Go slow. Your doctor will increase doses over 3-6 months. Don’t stop because you feel worse at first. That’s your body adjusting. Talk to your provider before quitting.

The hidden gap: Race, access, and inequality
Heart failure doesn’t affect everyone equally. A 2025 AHA statement found Black patients are 37% less likely to get guideline-recommended therapy and have nearly 30% higher death rates-even after adjusting for income, education, or insurance.
Why? Systemic issues: fewer referrals to specialists, longer wait times, mistrust in the system, and less access to advanced devices like CardioMEMS. This isn’t about individual choices. It’s about broken systems.
Organizations are trying to fix this. The "HF in a Box" toolkit includes culturally tailored materials. Some hospitals now assign patient navigators to help with appointments, prescriptions, and transportation. But progress is slow. You need to be your own advocate-ask: "Am I getting the full treatment?" If the answer isn’t clear, seek a second opinion.
What’s next? The future of heart failure care
Science is moving fast. Researchers are now studying a hidden risk factor called CHIP-Clonal Hematopoiesis of Indeterminate Potential. It’s a blood condition where mutated cells cause inflammation, damaging the heart. About 1 in 5 people over 70 have it. The INTERCEPT-HF trial is testing whether blocking inflammation with canakinumab can help.
Another big question: should blood pressure targets be different for HFrEF vs. HFpEF? A 2025 meta-analysis found low BP (<90 mmHg) is riskier for HFpEF patients. That means what’s safe for one person might be dangerous for another. The TARGET-HF trial, starting in 2025, is testing personalized BP goals. Results won’t come until 2027, but it’s a step toward truly individualized care.
Living well with heart failure: Real-life tips
Medicines help-but your daily choices matter just as much.
- Watch your salt. Less than 2,000 mg a day. Read labels. Avoid canned soups, processed meats, and restaurant food.
- Weigh yourself daily. A 2-pound gain in one day? That’s fluid. Call your doctor.
- Move, but don’t overdo it. Walking 20-30 minutes most days helps. Talk to your care team about a cardiac rehab program. They’re proven to extend life.
- Get vaccinated. Flu, pneumonia, and COVID-19 hit heart failure patients harder. Stay up to date.
- Use a pill organizer. Or ask for a medication review with your pharmacist. Eight pills a day? You’re not alone. But you don’t have to manage it alone.
Heart failure doesn’t mean giving up. It means adapting. Many people live 10, 15, even 20 years with it-especially if they’re on the right treatment and stay engaged with their care.
Can heart failure be cured?
Heart failure is usually a lifelong condition, but it can be managed so well that symptoms disappear for years. In rare cases-like when it’s caused by a treatable valve problem or severe alcohol use-remission is possible. But for most people, the goal is to slow progression, reduce hospital visits, and live as fully as possible.
Do I need to stop all my other medications?
No. Most people with heart failure also take medicines for high blood pressure, diabetes, or arthritis. Your doctor will review everything to avoid dangerous interactions. Some older diabetes drugs like pioglitazone may need to be stopped, but others like metformin or SGLT2 inhibitors are actually helpful. Always talk to your provider before changing anything.
Is it safe to exercise with heart failure?
Yes-when done safely. Inactivity makes heart failure worse. Start with short walks, 5-10 minutes at a time. Build up gradually. Cardiac rehab programs are ideal-they monitor your heart while you exercise and teach you how to recognize warning signs. If you feel dizzy, chest pain, or extreme shortness of breath, stop and rest. Don’t push through pain.
Why do I need four medicines when I only feel one symptom?
Heart failure affects your body in multiple ways: fluid buildup, nerve overactivity, inflammation, and kidney stress. Each medicine targets a different problem. Taking them together is like fixing a leaky roof, fixing the gutters, and cleaning the drains-all at once. One pill won’t do it all. The science shows you get the best results when you take all four.
What if I can’t afford these medicines?
SGLT2 inhibitors and ARNIs can be expensive, but help exists. Many drug companies offer patient assistance programs. Medicare Part D and private insurers often cover them. Ask your pharmacist or care team about generic alternatives, co-pay cards, or nonprofit foundations that help with medication costs. Never skip doses because of cost-there’s always a solution if you ask.
Final thought: You’re not alone in this
Heart failure is complex, but the tools to manage it are better than ever. The journey isn’t easy-it takes daily effort, regular check-ups, and sometimes hard conversations with your doctor. But millions of people are living well with it. They’re walking their grandchildren to school, traveling, gardening, and enjoying life. You can too. Start with the right treatment. Stay consistent. Ask questions. And don’t let fear stop you from getting the care you deserve.

shubham seth
November 16, 2025 AT 19:23Also, CardioMEMS? If your hospital doesn’t offer it and you’re a frequent flyer, demand it. It’s not luxury. It’s survival.
Kathryn Ware
November 18, 2025 AT 18:20kora ortiz
November 19, 2025 AT 19:38Jeremy Hernandez
November 21, 2025 AT 18:23Tarryne Rolle
November 22, 2025 AT 23:41Kyle Swatt
November 23, 2025 AT 19:28saurabh lamba
November 24, 2025 AT 18:18Kiran Mandavkar
November 25, 2025 AT 08:47Eric Healy
November 25, 2025 AT 17:28Shannon Hale
November 26, 2025 AT 02:10satya pradeep
November 27, 2025 AT 01:51Prem Hungry
November 28, 2025 AT 22:52