How Smoking Increases the Risk of Pancreatic Duct Blockage
 Sep, 26 2025
Sep, 26 2025
Pancreatic duct blockage is a condition where the main conduit that carries digestive enzymes from the pancreas to the duodenum becomes narrowed or obstructed, often leading to severe abdominal pain, inflammation, and impaired digestion. While gallstones and chronic pancreatitis are well‑known culprits, growing evidence shows that smoking is a silent accelerator. In this article we unpack why cigarettes matter for your pancreas, compare smoking to other lifestyle risks, and outline practical steps to keep the duct flowing freely.
What Is the Pancreatic Duct?
Pancreatic duct is a thin tube that transports bile‑rich pancreatic juices from the glandular tissue to the small intestine. It works hand‑in‑hand with the pancreas, an elongated organ tucked behind the stomach that produces digestive enzymes and hormones like insulin. When the duct narrows, enzymes back‑up, triggering inflammation (pancreatitis) and, over time, fibrosis that cements the blockage permanently.
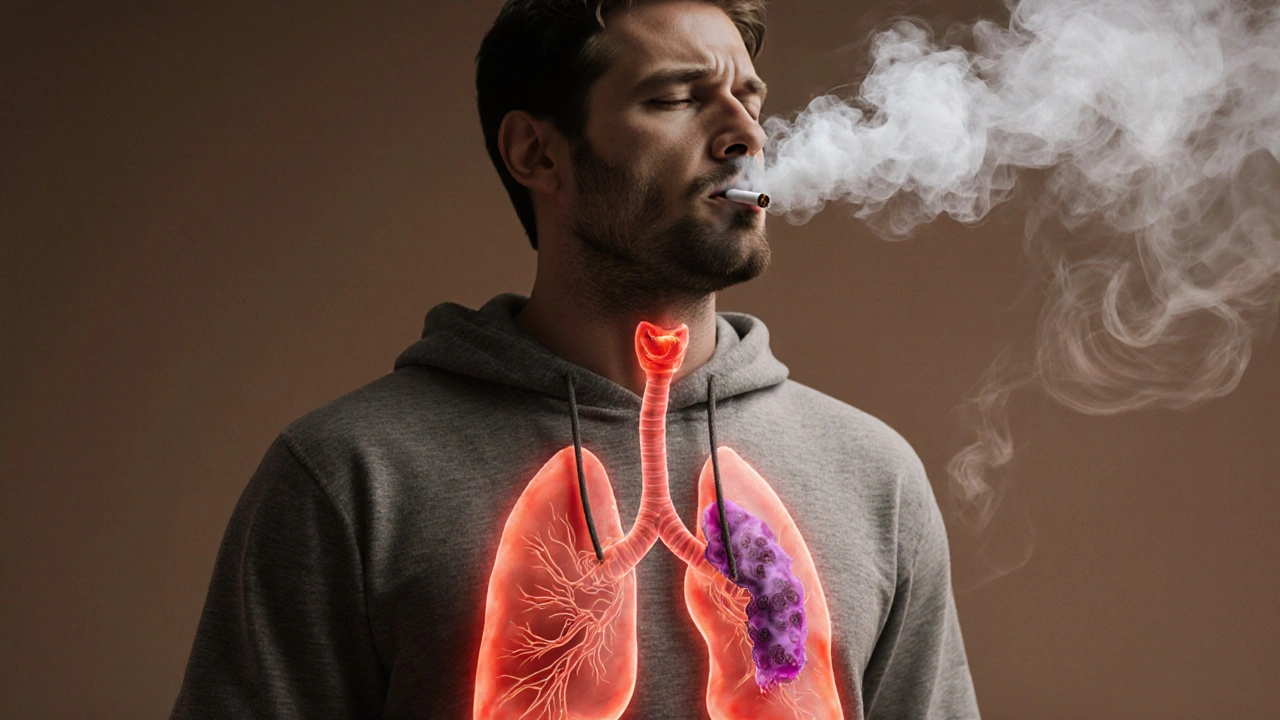
Smoking: More Than a Lung Hazard
Smoking is a behavior involving inhalation of tobacco smoke, which delivers nicotine, tar, and hundreds of carcinogenic chemicals into the bloodstream. In South Africa, the National Department of Health reports that roughly 15% of adults smoke daily, and these toxins circulate far beyond the lungs.
The key offender for the pancreas is nicotine, a stimulant that induces vasoconstriction, raises blood pressure, and stimulates the release of stress hormones. Nicotine’s impact on tiny blood vessels feeding the pancreas reduces oxygen delivery, creating a hypoxic environment that encourages scar tissue formation.
How Smoking Triggers Duct Obstruction
- Fibrosis and scarring: Chronic exposure to tobacco‑derived free radicals stimulates pancreatic stellate cells, which lay down collagen. The resulting fibrosis stiffens the duct walls and narrows the lumen.
- Enzyme activation: Carcinogens such as nitrosamines alter the pH of pancreatic secretions, prompting premature activation of enzymes like trypsin. These enzymes digest ductal tissue from the inside out, forming strictures.
- Calcification: Heavy metals in smoke (e.g., cadmium) precipitate calcium salts within the duct, creating hard plugs that block flow.
- Reduced bicarbonate secretion: Nicotine interferes with ductal bicarbonate‑producing cells, lowering the fluid’s ability to flush debris, which then accumulates.
Collectively, these mechanisms raise the odds of blockage by up to three‑fold in long‑term smokers, according to a 2023 cohort study from the University of Cape Town.
Risk Comparison: Smoking vs. Alcohol Consumption
| Risk Factor | Primary Harmful Agent | Odds Ratio (Adjusted) | Typical Mechanism |
|---|---|---|---|
| Smoking | Nicotine, nitrosamines | 3.1 | Fibrosis, enzyme activation, calcification |
| Alcohol consumption (≥30g/day) | Ethanol, acetaldehyde | 2.4 | Pancreatic inflammation, protein plug formation |
| Combined smoking & alcohol | Both nicotine and ethanol | 4.8 | Synergistic fibrosis and ductal injury |
The table shows that while heavy drinking is a clear danger, smoking alone carries a higher independent odds ratio. When the two habits coexist, risk skyrockets, underlining the importance of addressing both.

Clinical Consequences of a Blocked Duct
A blocked pancreatic duct doesn’t stay quiet. Patients often report:
- Steady, gnawing epigastric pain that worsens after meals.
- Episodes of acute pancreatitis, marked by nausea, vomiting, and elevated serum amylase.
- Long‑term malabsorption, leading to weight loss and vitamin deficiencies.
- Secondary diabetes, as the islets of Langerhans lose function amid chronic inflammation.
Radiologists detect obstruction via magnetic resonance cholangiopancreatography (MRCP) or a contrast‑enhanced computed tomography (CT) scan. Endoscopic examination often confirms the finding.
Diagnosis and Therapeutic Options
Endoscopic retrograde cholangiopancreatography (ERCP) is a minimally invasive procedure that injects contrast into the pancreatic duct and allows physicians to visualize strictures, stones, or tumors. During ERCP, a specialist can place a pancreatic stent, a tiny tube that props the duct open, restoring flow of enzymes. In cases where stone fragments are present, lithotripsy or balloon dilation may be employed.
For smokers, the most effective long‑term strategy is cessation. Studies demonstrate that quitting reduces the progression of ductal fibrosis within two years, even if partial strictures already exist.
Prevention: Lifestyle Modifications that Matter
Beyond quitting, the following habits lower the chance of blockage:
- Adopt a low‑fat diet: Excess fat overloads enzyme production, increasing the risk of protein plugs.
- Maintain healthy weight: Obesity fuels systemic inflammation that aggravates pancreatic tissue.
- Limit alcohol: Stick to moderate consumption (≤1 drink per day for women, ≤2 for men).
- Regular medical check‑ups: Early imaging in high‑risk smokers can catch narrowing before symptoms appear.
Support programs such as the South African Tobacco Control Programme provide counseling, nicotine‑replacement therapy, and community groups that have helped over 20,000 smokers quit in the past five years.
Related Topics in the Pancreatic Health Cluster
Understanding duct blockage sits within a broader health cluster:
- Pancreatic cancer: Chronic inflammation from blockage raises malignant transformation risk.
- Chronic pancreatitis: Persistent duct obstruction is a major driver of this debilitating disease.
- Diabetes mellitus type3c: Secondary diabetes caused by pancreatic exocrine damage.
- Genetic predisposition: Mutations in PRSS1 or CFTR can amplify the impact of smoking.
Readers interested in any of these areas can explore dedicated articles on our site for deeper insight.
Frequently Asked Questions
Can occasional smoking still cause pancreatic duct blockage?
Even light or social smoking introduces nicotine and carcinogens that trigger micro‑vascular changes in the pancreas. While the absolute risk is lower than with heavy use, studies show a 1.5‑fold increase in ductal strictures among occasional smokers compared with never‑smokers.
Is the blockage always permanent?
Early‑stage strictures can be dilated endoscopically or resolved with stenting. Lifestyle changes, especially quitting smoking, can halt further fibrosis and sometimes allow the duct to remodel naturally.
How long does it take for smoking cessation to lower the risk?
Risk begins to decline within 6‑12 months of quitting, with a 30‑40% reduction in new strictures after two years. Full risk normalization may take 10‑15 years, mirroring trends seen in lung disease.
Are there any screening tests for smokers?
High‑risk smokers (≥20 pack‑years) are advised to undergo annual MRCP or endoscopic ultrasound (EUS) to detect early ductal changes. Blood markers like serum lipase are not reliable for asymptomatic screening.
Can diet alone reverse a blocked duct?
Dietary adjustments can lessen enzyme overload and reduce inflammation, but they cannot physically clear an existing obstruction. They are most effective as adjuncts to medical intervention and smoking cessation.

Nikita Warner
September 26, 2025 AT 12:10Thanks for sharing this comprehensive breakdown. The article nicely outlines how nicotine induces vasoconstriction, activates pancreatic stellate cells, and promotes calcification, all of which contribute to ductal fibrosis. It also correctly highlights the three‑fold increase in blockage risk for long‑term smokers, which aligns with recent cohort data from Cape Town. Quitting smoking, therefore, isn’t just about lung health-it directly mitigates pancreatic injury.
For anyone tracking their risk, I’d recommend annual MRCP scans after 20 pack‑years, combined with a low‑fat diet and regular exercise to improve microvascular perfusion.
Liam Mahoney
September 26, 2025 AT 14:57Honestly, smooching a cigarette every day is just plain selfish. You think it’s just a “choice,” but you’re literally poisoning your own pancreas and, by extension, the whole nation’s health. If people cared less about their own selfish habits they’d quit already. Stop being a walking hazard and think about the folks around you who suffer because of your smoke‑filled lungs. This kind of behaviour is unacceptable.
Justin Ornellas
September 26, 2025 AT 17:44Behold, the tragedy of modern indulgence-smoking, a seemingly innocuous vice, that orchestrates a silent symphony of cellular demise within the pancreas. One must contemplate the philosophical absurdity of inhaling toxins that, like Faustian bargains, promise fleeting gratification while sealing one’s organ’s fate. Yet, the empirical evidence is unequivocal: nicotine’s vasoconstrictive grip paves the path to hypoxia, and in turn, to the fibrotic barricades that choke the pancreatic duct. Let this serve as a cautionary allegory for all who tread the nicotine‑laden path.
JOJO Yang
September 26, 2025 AT 20:30Yo, this is like the most dramatical thing ever-smoking turning your pancreas into a crumpled paper! I cant even believe how the nicotine just sprints into your blood and starts building scar tissue like a rogue artist. And the calcification? It's like your duct is turning into a stony monument dedicated to bad choices. Seriously, quit or watch your tummy scream.
Faith Leach
September 26, 2025 AT 23:17Wake up! The pharma companies and global elites don’t want you to know that smoking fuels pancreatic disease because it fills their pockets with treatment profits. It’s a coordinated assault on our bodies, especially in countries that prize independence. The moment you light up, you’re feeding an industry that thrives on your suffering. Stand strong for our nation’s health and reject this poison.
Eric Appiah Tano
September 27, 2025 AT 02:04Hey everyone, great read! If you’re a smoker, think of quitting as a power move for your overall wellness. Pair cessation with a balanced, low‑fat diet and a bit of daily movement, and you’ll give your pancreas a fighting chance. Remember, support groups and nicotine‑replacement therapy are there to help-don’t hesitate to reach out.
Ryan Torres
September 27, 2025 AT 04:50They don’t tell you that the tobacco giants secretly embed tracking chips in cigarettes to monitor your health decline! 🤯💣 Every puff is a data point they harvest while your pancreas deteriorates. Stay vigilant, question the narrative, and protect your body from these hidden agendas. 🚨🛡️
shashi Shekhar
September 27, 2025 AT 07:37Oh, so now we’re supposed to believe smoking is the only villain? Yeah, right. Maybe the real problem is the government keeping us in the dark about the real causes while they profit off our misery. 😂 But hey, if you want to keep lighting up, go ahead-just don’t expect anyone to care when your pancreas collapses.
Marcia Bailey
September 27, 2025 AT 10:24Thanks for the info! 😊 It’s really helpful to see the clear connection between smoking and pancreatic blockage. If anyone’s looking for resources, the South African Tobacco Control Programme offers free counseling and nicotine patches. Stay strong, friends!
Hannah Tran
September 27, 2025 AT 13:10From a clinical perspective, the pathophysiological cascade initiated by nicotine involves endothelial dysfunction, oxidative stress, and activation of pancreatic stellate cells, culminating in periductal fibrosis. This fibrogenic milieu not only narrows the lumen but also predisposes to protein plug formation, synergistically amplifying obstructive risk when coupled with ethanol‑induced acinar injury. Early detection via MRCP, coupled with targeted cessation strategies, represents a pragmatic approach to mitigating this multifactorial disease process.
Crystle Imrie
September 27, 2025 AT 15:57Smoking turns your pancreas into a battlefield-choose peace.
Dhananjay Sampath
September 27, 2025 AT 18:44Indeed, the data presented in the article, while extensive, underscores a critical point,; smoking is not merely a respiratory hazard,; it is a systemic toxin,; and the pancreatic duct is particularly vulnerable; the mechanisms-fibrosis, enzymatic activation, calcification-are intertwined,; each amplifying the other; therefore, a comprehensive cessation program, complemented by dietary modifications, and regular imaging surveillance, becomes indispensable; clinicians must adopt a multi‑disciplinary approach, and patients should be empowered with education, support, and access to resources; only then can we hope to reverse the trend.
kunal ember
September 27, 2025 AT 21:30When we examine the relationship between tobacco use and pancreatic health, it becomes clear that nicotine acts as more than a simple stimulant; it is a potent vasoconstrictor that diminishes microvascular perfusion within the gland. This reduction in oxygen delivery creates a hypoxic environment that encourages the activation of pancreatic stellate cells, the very architects of fibrotic tissue. Over time, the accumulation of collagen around the ductal walls progressively narrows the lumen, impeding the flow of essential digestive enzymes. Simultaneously, nitrosamines present in cigarette smoke can alter the pH balance of pancreatic secretions, prompting premature activation of trypsin and other proteases. These enzymes, now inappropriately active, begin to digest the ductal epithelium from within, forming strictures that further exacerbate obstruction. Heavy metals such as cadmium, also inhaled with each puff, have a propensity to precipitate calcium salts, leading to calcific plugs that stubbornly block the conduit. Moreover, nicotine interferes with bicarbonate‑producing cells, decreasing the alkaline buffer needed to flush debris and increasing the likelihood of residue buildup. The cumulative effect of these processes is a threefold increase in the odds of ductal blockage among chronic smokers, as documented in recent cohort studies. Importantly, cessation of smoking initiates a cascade of reparative mechanisms; microvascular flow improves, stellate cell activation wanes, and the progression of fibrosis can be halted. Clinical observations suggest that within two years of quitting, many patients exhibit stabilization of ductal diameter and reduced incidence of new strictures. However, for those with established fibrosis, endoscopic interventions such as stenting or lithotripsy remain essential to restore patency. Lifestyle modifications, including a low‑fat diet and weight management, complement these medical approaches by decreasing the metabolic load on the pancreas. Regular imaging surveillance, particularly MRCP or EUS, enables early detection of subclinical narrowing before symptomatic pancreatitis ensues. Ultimately, the prevention of pancreatic duct blockage hinges on a multifactorial strategy that prioritizes smoking cessation, dietary mindfulness, and vigilant medical follow‑up.
Kelly Aparecida Bhering da Silva
September 28, 2025 AT 00:17Our nation’s strength lies in protecting our bodies from foreign toxins, and smoking is a clear enemy of our health sovereignty. The infiltration of nicotine into our bloodstream is a covert assault that compromises not only lungs but also vital organs like the pancreas. By rejecting cigarettes, we assert our independence from corporate manipulation and safeguard our genetic legacy for future generations. Let’s unite in a decisive, patriotic push to end this harmful habit once and for all.
Michelle Dela Merced
September 28, 2025 AT 03:04Can you even imagine the drama of a pancreas suffocating because of a tiny cigarette? It’s like watching a tragedy unfold in slow motion-so avoidable, so cruel! 😱🔥 Quit now or watch the drama continue!