Nexium (Esomeprazole) vs Alternatives: Which Acid‑Reducer Is Right for You?
 Sep, 30 2025
Sep, 30 2025
Acid Reducer Comparison Tool
Select your preferences to get a personalized recommendation on the best acid reducer for your needs.
When your stomach starts making that burning, uncomfortable feel, you reach for a medication that can bring relief fast. Nexium is the brand name for esomeprazole, a proton‑pump inhibitor (PPI) that blocks the final step of stomach acid production. It’s been a go‑to for many dealing with gastro‑esophageal reflux disease (GERD), ulcers, and Zollinger‑Ellison syndrome. But is it the only smart choice? Below you’ll find a side‑by‑side look at the most common alternatives, so you can decide which acid‑reducer fits your life and health goals.
Quick Takeaways
- Nexium comparison: Nexium is the strongest PPI on the market but comes with a higher price tag.
- Esomeprazole works best for daily, long‑term control of severe GERD.
- Other PPIs (omeprazole, lansoprazole, pantoprazole) offer similar efficacy at lower cost.
- H2 blockers (ranitidine, famotidine) act faster but may need multiple doses.
- Consider side‑effect profile, drug interactions, and how you plan to use the medication.
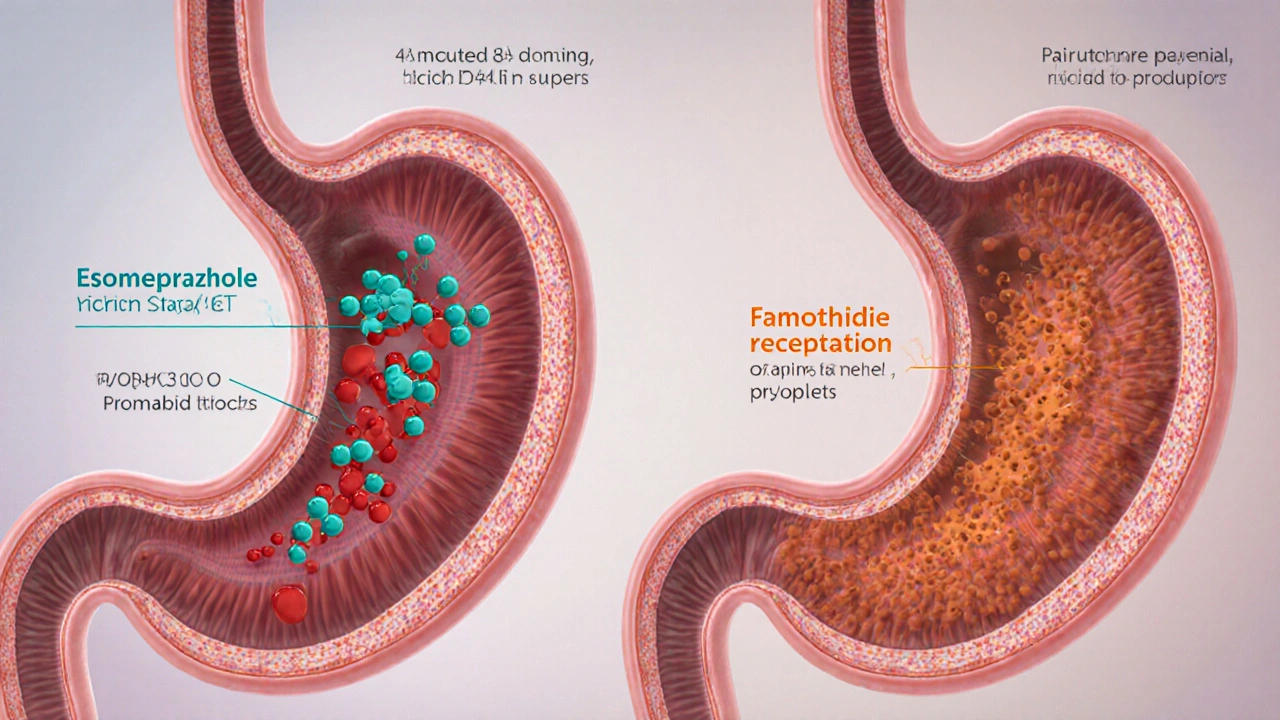
How Nexium (Esomeprazole) Works
Esomeprazole belongs to the proton‑pump inhibitor family. It targets the H+/K+ ATPase enzyme-often called the "proton pump"-found in the stomach lining. By binding to this pump, esomeprazole stops the final acid‑producing step, reducing gastric acidity by up to 95%.
Key attributes of Nexium:
- Onset: 1-4hours after the first dose.
- Duration: Up to 24hours of acid suppression.
- Dosing: Usually once daily before breakfast; can be increased to twice daily under doctor supervision.
- FDA‑approved uses: GERD, erosive esophagitis, duodenal ulcers, H.pylori eradication (as part of combo therapy), and Zollinger‑Ellison syndrome.
Because it’s a racemic *S*-enantiomer of omeprazole, Nexium claims slightly better bioavailability and a more consistent effect across patients. In practice, the benefit is modest-most people feel the same relief whether they take esomeprazole or its older sibling omeprazole.
Top Alternatives to Consider
Below are the most frequently prescribed acid‑reducer families. Each entry includes a brief definition with structured data markup.
Omeprazole (brand name Prilosec) is a first‑generation PPI that works the same way as esomeprazole but is usually $30‑$40 cheaper per month.
Lansoprazole (brand Prevacid) offers a slightly faster onset (about 30minutes sooner) and is popular for patients with night‑time heartburn.
Pantoprazole (brand Protonix) has a long half‑life, making it a good choice for people who need consistent coverage over 24hours.
Rabeprazole (brand AcipHex) is often touted for its rapid acid suppression and lower drug‑interaction potential.
Ranitidine (brand Zantac) is an H2 blocker that blocks histamine receptors, offering quicker relief (within 30minutes) but shorter duration (6‑8hours).
Famotidine (brand Pepcid) works like ranitidine but is less likely to cause liver toxicity and remains widely available after ranitidine’s recall.
Antacids (e.g., Tums, Maalox) neutralize existing acid instantly but provide only brief relief (1‑2hours).
Head‑to‑Head Comparison
| Attribute | Nexium (Esomeprazole) | Omeprazole (Prilosec) | Lansoprazole (Prevacid) | Ranitidine (Zantac) | Famotidine (Pepcid) |
|---|---|---|---|---|---|
| Drug class | Proton‑Pump Inhibitor | Proton‑Pump Inhibitor | Proton‑Pump Inhibitor | H2 Blocker | H2 Blocker |
| Typical dose | 40mg once daily | 20‑40mg once daily | 15‑30mg once daily | 150mg twice daily | 20‑40mg twice daily |
| Onset of relief | 1‑4hrs | 1‑4hrs | 30‑60min | 30min | 30‑60min |
| Duration of effect | ≈24hrs | ≈24hrs | ≈24hrs | 6‑8hrs | 6‑8hrs |
| Cost (US $/month) | ≈$70‑$95 (brand) | ≈$30‑$45 (generic) | ≈$35‑$50 | ≈$15‑$25 | ≈$20‑$30 |
| Common side effects | Headache, diarrhea, nausea, possible B12 deficiency | Headache, abdominal pain, risk of C.difficile | Diarrhea, abdominal pain, rare liver enzymes rise | Headache, dizziness, rare liver injury | Headache, constipation, rarely kidney issues |
| Drug‑interaction risk | High (clopidogrel, warfarin, HIV meds) | Moderate (clopidogrel, certain antifungals) | Low‑moderate | Low | Low |
| Best for | Severe/ chronic GERD, erosive esophagitis | Mild‑moderate GERD, cost‑sensitive patients | Night‑time heartburn, patients needing fast onset | On‑demand relief, occasional heartburn | Frequent mild symptoms, safer in pregnancy |
Choosing the Right Option - A Decision Guide
Not every acid‑reducer suits every person. Use the checklist below to narrow down your ideal match.
- How often do you experience symptoms?
- Daily or nightly → A PPI (Nexium, omeprazole, lansoprazole) gives sustained control.
- Occasional (once a week or less) → An H2 blocker or antacid may be enough.
- Do you need rapid relief?
- If you want relief within 30minutes, reach for famotidine or ranitidine.
- For a slower, long‑lasting effect, stick with a PPI.
- What’s your budget?
- Brand‑name Nexium is pricey; generic omeprazole or lansoprazole cut costs dramatically.
- H2 blockers and antacids are the most affordable “as‑needed” options.
- Any existing health conditions?
- Patients on clopidogrel or certain HIV meds should avoid or adjust dose of Nexium because of interaction.
- Kidney disease patients may need dose adjustments for famotidine.
- How long do you plan to treat?
- Short courses (<4weeks) are safe for most PPIs; long‑term use should be discussed with a doctor due to fracture and B12 concerns.
- For brief symptom spikes, H2 blockers are ideal.
Ask yourself these points, then talk to your healthcare provider. The right choice often balances efficacy, cost, and safety.
Common Pitfalls & Safety Tips
Even over‑the‑counter (OTC) meds can cause trouble if misused.
- Never double‑dose. Taking more than the recommended amount of a PPI doesn’t speed up relief; it only raises risk of infections and nutrient malabsorption.
- Watch for rebound acid hypersecretion. Stopping a PPI abruptly after weeks of use can trigger a flare‑up. Taper down under medical guidance.
- Check for drug interactions. If you’re on blood thinners, antiretrovirals, or antifungal meds, let the pharmacist know before picking up a PPI.
- Pregnancy and breastfeeding. Famotidine has the most safety data; most PPIs are classified as “Category C” and should be used only if benefits outweigh risks.
- Be wary of chronic use. Long‑term PPI therapy has been linked to higher rates of kidney disease, dementia, and bone fractures. Routine monitoring of magnesium and B12 levels is advised for anyone on PPIs beyond 6‑12months.
Frequently Asked Questions
Can I switch from Nexium to a cheaper generic PPI without losing effectiveness?
Yes. Omeprazole and lansoprazole have almost identical mechanisms, and most patients notice no drop in symptom control. A short trial period under doctor supervision helps confirm the switch works for you.
Are H2 blockers safe to use together with a PPI?
Combining an H2 blocker with a PPI can provide extra night‑time coverage, but it’s usually unnecessary for most patients. Talk to a clinician because overlapping acid suppression may increase infection risk.
What should I do if I miss a dose of Nexium?
Take the missed tablet as soon as you remember, unless it’s almost time for the next dose. Then skip the missed one-don’t double‑up.
Is it okay to take Nexium for more than a year?
Long‑term use is possible but requires monitoring. Doctors often check magnesium, calcium, and vitamin B12 levels every 6‑12months and may step down to the lowest effective dose.
Do antacids work at the same time as a PPI?
Yes, antacids can be taken on‑demand for breakthrough pain while a PPI works in the background to keep overall acid low.
Bottom line: Nexium offers powerful, long‑lasting relief, but it isn’t the only game in town. By weighing your symptom pattern, budget, and health backdrop, you can pick a medication that keeps your stomach calm without unnecessary expense or risk.

Chelsea Wilmer
September 30, 2025 AT 20:10When one contemplates the labyrinthine world of gastric pharmacology, it becomes evident that the choice of an acid reducer is not a mere exercise in brand loyalty but a profound philosophical inquiry into the nature of relief itself.
Consider, for a moment, the ontological weight of a proton‑pump inhibitor that dares to alter the very chemistry of the stomach's inner milieu, promising a suppression of acid that borders on the alchemical.
The esoteric dance between esomeprazole and its cousins-omeprazole, lansoprazole, pantoprazole-mirrors the subtle interplay of forces that govern our bodies, each with a unique kinetic profile, half‑life, and price tag, each whispering a different promise to the afflicted soul.
Yet, the economic dimension cannot be dismissed, for the lofty cost of Nexium forces the patient to weigh the intangible benefits of potential marginal efficacy against the tangible reality of monthly expenditures.
One must also ponder the ethical implications of long‑term PPI use, as the specter of vitamin B12 deficiency, magnesium depletion, and altered gut microbiota looms like a quiet existential dread.
Moreover, the interaction matrix, especially with antiplatelet agents such as clopidogrel, forces clinicians to navigate a treacherous moral landscape where the desire for symptom control may inadvertently compromise cardiovascular protection.
In contrast, the H2 blockers, with their swift onset, offer an immediacy that appeals to the impatient heart, yet their episodic coverage may be insufficient for chronic erosive disease.
Antacids, those humble alkaline saviors, provide fleeting solace, a reminder that not all solutions demand permanence; sometimes a momentary neutralization suffices.
The decision matrix, therefore, resembles a multidimensional chessboard, where factors such as symptom frequency, urgency of relief, budgetary constraints, comorbid conditions, and treatment duration intersect in complex patterns.
Thus, the patient must become an active participant, an architect of his own therapeutic destiny, rather than a passive recipient of pharmaceutical fiat.
From a systems‑level perspective, the healthcare ecosystem benefits when patients are educated, for informed choices reduce unnecessary switches, lower the burden of adverse events, and promote cost‑effective prescribing.
Clinicians, too, are called upon to embody the role of sage guides, translating dense pharmacokinetic data into relatable narratives that empower the individual.
Christopher Xompero
September 30, 2025 AT 20:35i cant even with this whole acid reducer drama bro i mean, who needs another pill when the stomach already be like a volcano? Nexium's pricey af but if ur like on the daily grind of heartburn you might as well splurge, right? i tried omeprazole once and it was okay but not as strong as the "king" Nexium. also, the side effects? headache, diarrhea… i heard ppl get bc deficiency after months, but lol who has time for that. plus, the interaction with clopidogrel? yeah, that’s a whole other level of drama. overall i think just stick to famotidine for fast fix unless you want to be on a budget and rodeo with cheap meds.
Jason Lancer
September 30, 2025 AT 21:00Exactly, the drug interaction risk is real.
lindsey tran
September 30, 2025 AT 21:53Hey folks! 🌟 If you're juggling a hectic schedule and the dreaded nightly heartburn, remember that relief doesn't have to be a nightmare. A PPI like Nexium can be a superhero for severe GERD, but don't forget the trusty sidekick-famotidine-for those moments when you need quick action. Keep an eye on your budget, because the generic versions of omeprazole or lansoprazole are often just as effective without breaking the bank. And hey, if you're on clopidogrel, talk to your doc about the best option-there are safer routes! Stay empowered, stay comfortable, and keep that stomach happy! 💪
Krishna Sirdar
September 30, 2025 AT 22:53When we think about acid reducers, it's useful to start from a simple place: how often does the pain happen? If it's daily, a proton‑pump inhibitor gives steady control; if it's just once a week, an H2 blocker or antacid works fine. Also, the speed of relief matters-famotidine and ranitidine act within half an hour, while PPIs need a few hours to kick in. In many cases, the cheaper generic omeprazole provides the same benefit as the brand‑name Nexium, so consider cost first. Finally, always check for interactions, especially if you're on blood thinners or HIV meds. These basics help you make a balanced choice.
becca skyy
September 30, 2025 AT 23:53People often overlook the cultural aspects of medication choices-like how certain communities may prefer over‑the‑counter antacids because they’re readily available and familiar. It’s also worth noting that generic versions of PPIs have become more common globally, which can help reduce costs without sacrificing efficacy. When you read the label, pay attention to the active ingredient and not just the brand name; that can ease the transition if you need to switch due to insurance or availability. In short, stay informed and don’t let marketing jargon drive your health decisions.
Ryan Walsh
October 1, 2025 AT 00:53Generic omeprazole works well for most people.
Kiersten Denton
October 1, 2025 AT 01:53Sounds solid.
Karl Norton
October 1, 2025 AT 02:53Let’s cut to the chase: if you’re a high‑risk patient on clopidogrel, ditch the brand‑name Nexium and go for a safer PPI like pantoprazole or even a low‑dose H2 blocker. The reason? High drug‑interaction potential is a real thing, and I’m not here to sugarcoat it. Also, the price difference between brand and generic is ridiculous-why pay double? If you’re after fast relief, famotidine beats everything, quick as a flash. Bottom line: match the drug to your specific clinical scenario, not the marketing hype.
Ashley Leonard
October 1, 2025 AT 03:53I appreciate the thorough breakdown! For anyone dealing with occasional heartburn, an antacid may be all you need, but if the symptoms become frequent, it’s smart to upgrade to a PPI or H2 blocker. Also, keep an eye on any new side‑effects and discuss them with your physician-especially if you’re on other meds.
Ramanathan Valliyappa
October 1, 2025 AT 04:53Check drug interactions; be precise.
Nymia Jones
October 1, 2025 AT 05:53It is impossible to ignore the hidden agendas that pharmaceutical conglomerates embed within the seemingly innocuous packaging of acid‑reduction therapies. While the public is bombarded with glossy advertisements touting the superiority of Nexium, a closer examination reveals a concerted effort to marginalize cheaper alternatives, thereby inflating healthcare costs and perpetuating a cycle of dependency.
Consider the subtle yet pervasive influence of insurance formularies that routinely place generic PPIs on the lowest tier, yet simultaneously commission “clinical trials” that emphasize marginal benefits of the branded product, all while downplaying the long‑term safety concerns associated with chronic use.
The data on B12 deficiency, increased risk of fractures, and potential renal complications are often relegated to footnotes, hidden beneath dense statistical jargon that the average consumer cannot decipher without a medical degree.
Moreover, the interplay between drug‑drug interactions-particularly the attenuation of clopidogrel’s antiplatelet effect-has been documented extensively in peer‑reviewed literature, yet the same literature is rarely highlighted in mainstream medical marketing, thereby leaving patients unknowingly exposed to heightened cardiovascular risk.
In light of these considerations, it is prudent for individuals to demand transparency from their healthcare providers, to scrutinize the cost‑benefit ratio of brand versus generic, and to prioritize shared decision‑making over the one‑sided narratives propagated by corporate interests.
Only through vigilant, informed engagement can we hope to reclaim autonomy over our gastrointestinal health and defy the subtle coercion embedded within the pharmaceutical status quo.
swapnil gedam
October 1, 2025 AT 06:53Choosing the right medication is like picking the right tool for a job. If your heartburn shows up only once in a while, you probably don’t need a daily PPI; an antacid or H2 blocker will do the trick. If you’re dealing with nightly symptoms, a PPI such as omeprazole or lansoprazole might be more appropriate. Also, keep an eye on how fast you need relief-famotidine works within 30 minutes, while PPIs may take a few hours to reach full effect. And remember to factor in cost-generic options are usually just as effective and much easier on the wallet.
Michael Vincenzi
October 1, 2025 AT 07:53Hey everyone, just wanted to add that it can be helpful to keep a simple symptom diary for a couple of weeks. Jot down when you feel the burn, what you ate, and what medication you took. This info can guide your doctor in choosing the most appropriate acid reducer-whether it’s a PPI for chronic control or an H2 blocker for fast, on‑demand relief. And don’t forget to discuss any other meds you’re on, because interactions can be sneaky.
Courage Nguluvhe
October 1, 2025 AT 08:53From a pharmacoeconomic standpoint, the marginal benefit of Nexium over generic PPIs is negligible, yet the price differential is substantial. For health systems aiming to optimize resource allocation, prioritizing generic omeprazole or lansoprazole can yield significant cost savings without compromising clinical outcomes. Additionally, the risk profile of PPIs-including potential renal implications and dysbiosis-necessitates judicious prescribing, favoring the lowest effective dose and shortest appropriate duration.
Oliver Bishop
October 1, 2025 AT 09:53Our nation’s health depends on making smart choices, not getting swayed by foreign marketing.
Alissa DeRouchie
October 1, 2025 AT 10:53Honestly the whole hype around Nexium is overblown its just another PPI no magical cure but sure it sells better if you throw a fancy name on it ;)
Emma Howard
October 1, 2025 AT 11:53Great rundown! I love how you listed both cost and speed-so helpful!! Keep the info coming.
dee gillette
October 1, 2025 AT 12:53One must adopt a critical stance when evaluating the purported superiority of Nexium over its generics. The extant literature does not substantiate a clinically meaningful advantage in acid suppression, yet the marketing narrative persists, driven perhaps by profit motives rather than patient benefit. Consequently, clinicians should prioritize evidence‑based prescriptions, favoring cost‑effective generics unless specific patient factors dictate otherwise.