Patient Information vs Healthcare Provider Information: How Label Differences Affect Care
 Oct, 30 2025
Oct, 30 2025
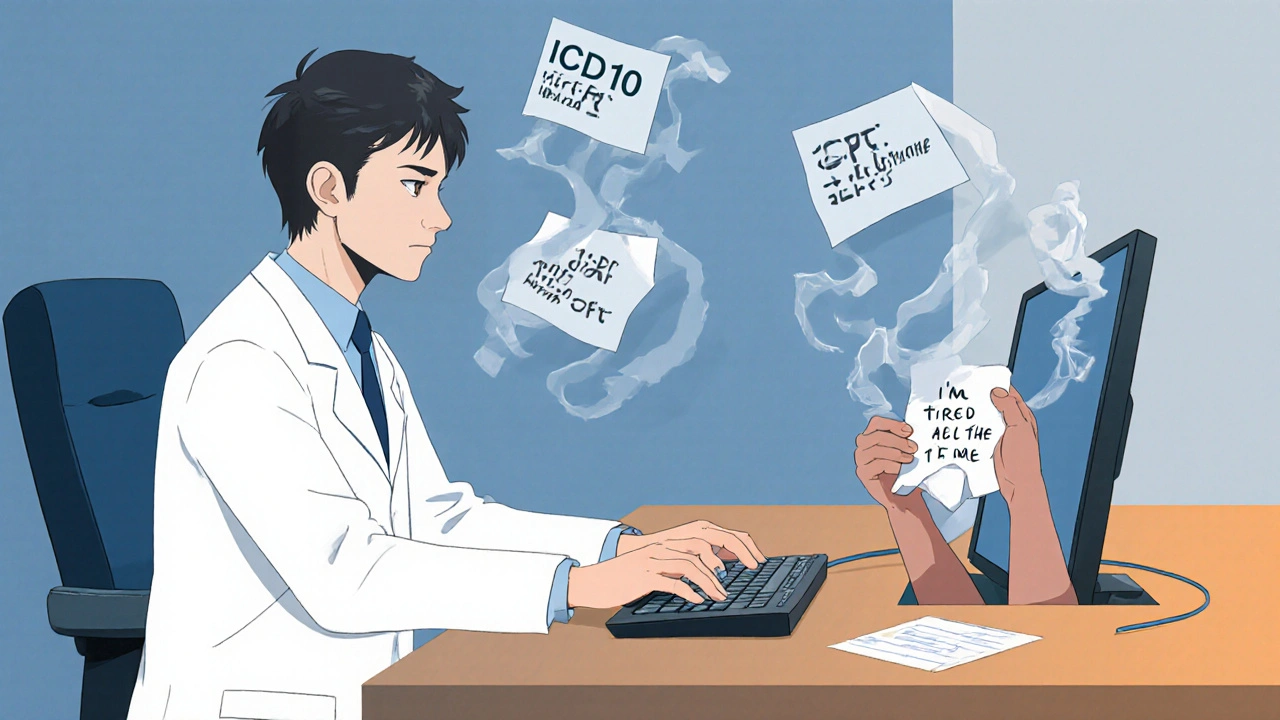
Why Your Doctor’s Notes Don’t Sound Like Your Symptoms
You go to the doctor feeling exhausted, dizzy, and like your body is running on empty. You tell them: "I’m always tired, I’m thirsty all the time, and I keep peeing at night." Later, you check your medical record online and see it says: "Type 2 Diabetes Mellitus, ICD-10 E11.9, poorly controlled." Suddenly, your experience feels erased. You didn’t hear "poorly controlled" - you heard "I’m failing." That’s not a mistake. It’s a gap.
Healthcare providers and patients don’t just see health differently - they speak different languages. The words doctors write down in their systems aren’t meant for you. They’re built for billing, coding, and research. But now, thanks to new laws and patient portals, you can read them. And that’s where the confusion starts.
How Providers Label Health: Codes, Not Stories
Doctors don’t write notes for patients. They write them for systems. Every symptom, test, and diagnosis gets turned into a code. ICD-10 has over 70,000 diagnosis codes. CPT codes track every procedure - from a simple blood draw to a heart surgery. These aren’t descriptions. They’re shorthand for computers and insurance companies.
When a provider writes "E11.9," they’re not saying "you’re sick." They’re telling the system: "This patient has type 2 diabetes without complications." That code triggers billing, determines treatment protocols, and feeds into national health data. It’s efficient - but cold. It doesn’t capture the sleepless nights, the fear of needles, or the shame of eating a cookie and feeling guilty.
Electronic Health Records (EHRs) like Epic and Cerner are designed around these codes. They’re optimized for speed, not understanding. A provider might type "DM2" or "HTN" in seconds. But those abbreviations? They’re meaningless to most patients. A 2019 study found 68% of patients didn’t understand common terms like "hypertension" or "colitis."
How Patients Describe Health: Feelings, Not Formulas
Patients don’t think in codes. They think in sensations. "My legs feel heavy." "I can’t get out of bed before noon." "The pain shoots down my arm when I bend over." These aren’t symptoms to be filed - they’re lived experiences. The American Health Information Management Association (AHIMA) calls this "the patient’s story." And it’s not just emotional - it’s essential.
When a patient says, "I take that white pill with breakfast," they’re describing metformin. But the chart says: "Metformin 500 mg BID." The patient doesn’t know what "BID" means. They don’t know it’s Latin for "twice a day." They just know they’re supposed to swallow something every morning - and sometimes they forget. That’s why medication errors happen.
On patient forums like PatientsLikeMe, people share stories like: "My doctor wrote 'poorly controlled DM' - I thought it meant I was a bad diabetic." That’s not just confusion. That’s trauma. And it’s common. A 2022 survey found 57% of patients felt confused by terms in their records. One in three avoided follow-up care because of it.
The Real Cost of the Labeling Gap
This isn’t just about feeling misunderstood. It’s about safety. Dr. Thomas Bodenheimer, a former UCSF professor, says language mismatches cause 30-40% of medication errors. That’s not a guess. It’s backed by data from the Institute of Medicine, which found communication failures contributed to 80% of serious medical mistakes.
When patients don’t understand their diagnosis, they don’t take their meds correctly. They skip appointments. They Google symptoms and panic. One patient thought "colitis" meant cancer. Another thought "hypertension" meant she had high blood pressure - and that she needed to stop eating salt forever. Neither was true. But the fear was real.
Providers feel the pressure too. A 2023 Medscape survey showed 64% of doctors spend 15 to 30 minutes per visit explaining terms they assumed were common knowledge. That’s time taken from other patients. It’s exhausting. And it’s avoidable.
How the System Is Starting to Change
Change is happening - slowly, but it’s happening. The 21st Century Cures Act of 2016 forced providers to give patients access to their clinical notes. By April 2021, no one could block that access. That meant millions of people could suddenly read their doctor’s notes - and many didn’t like what they saw.
So hospitals started adapting. Kaiser Permanente launched "Open Notes" in 2010. By 2021, they saw a 27% drop in patient confusion and a 19% increase in medication adherence. Why? Because they started rewriting notes in plain language. "Myocardial infarction" became "heart attack." "Hyperlipidemia" became "high cholesterol."
Mayo Clinic did the same. Their pilot program used smart EHR templates that auto-translated clinical terms for patient-facing documents. Results? A 38% reduction in patient confusion. That’s not magic. It’s just respect.
Now, the World Health Organization’s ICD-11 - rolled out globally in 2022 - includes patient-friendly descriptions alongside medical codes for the first time. That’s huge. And the HL7 FHIR standard, used by 78% of U.S. health systems, now lets systems show both the clinical term and the plain-language version side by side.

What You Can Do Right Now
You don’t have to wait for systems to fix this. Here’s what works:
- Ask: "Can you say that in plain English?" Don’t be shy. You’re paying for this care.
- Use the "teach-back" method: After your provider explains something, say, "So if I understand right, you’re saying ______. Is that correct?" Studies show this cuts miscommunication by 45%.
- Check your patient portal. If the note says "E11.9," Google it. Then ask: "Is that the same as type 2 diabetes?"
- Keep a personal health journal. Write down how you feel in your own words. Bring it to appointments. It helps your provider connect your story to their codes.
Some clinics now offer "health literacy navigators" - staff trained to translate medical jargon. Ask if yours does. If not, suggest it.
The Future: AI That Speaks Both Languages
Google’s Med-PaLM 2, released in May 2023, can convert clinical notes into patient-friendly language with 72.3% accuracy. That’s impressive - but not good enough yet. Clinical systems need 95% accuracy to be trusted.
Still, the direction is clear. By 2027, the American Medical Informatics Association predicts 60% of EHRs will have real-time translation built in. Imagine: You click "View Notes," and your doctor’s "hypertension" instantly becomes "high blood pressure." The code stays for billing. The plain language stays for you.
This isn’t about dumbing down medicine. It’s about making sure the people who live with illness - not just treat it - can understand what’s happening. Health isn’t just data. It’s dignity.
Frequently Asked Questions
Why do doctors use medical terms instead of plain language?
Doctors use medical terms because those terms are standardized across the entire healthcare system. Codes like ICD-10 and CPT are required for billing, insurance claims, and legal records. They ensure everyone - from hospitals to insurers to researchers - is talking about the same thing. But that doesn’t mean those terms should be the only version patients see. The shift now is toward showing both: the official code for systems, and plain language for people.
Can I ask my doctor to rewrite my medical notes in simpler terms?
Yes - and you should. You have the right to understand your health information. You can say, "I want to make sure I understand this correctly. Could you explain what this term means in everyday language?" Many providers now use plain-language templates, especially if they’re part of an Open Notes program. If they don’t, ask if they can add a patient-friendly summary to your record.
What’s the difference between ICD-10 and CPT codes?
ICD-10 codes describe diagnoses - like "Type 2 Diabetes" or "Depression." CPT codes describe procedures - like "blood test," "MRI," or "office visit." ICD-10 tells the system what’s wrong. CPT tells the system what was done about it. Both are used for billing, but only ICD-10 is used to track disease trends in public health.
Why does my portal say "poorly controlled diabetes" when I’ve been trying my best?
"Poorly controlled" is a clinical label based on your lab results - usually HbA1c levels above 8%. It doesn’t mean you’re lazy or failing. It means your blood sugar has been higher than the target range over the last few months. The label is about data, not judgment. Ask your provider: "What specific changes could help bring this number down?" That turns a judgment into a plan.
Are there tools that help translate medical terms for patients?
Yes. Many patient portals now include a "plain language" toggle. Some hospitals offer free apps or websites that translate medical terms - like MedlinePlus or Healthwise. Google’s Med-PaLM 2 is being tested in clinics to auto-translate notes. You can also ask your provider for a printed glossary. Most clinics have one - they just don’t always offer it unless you ask.

Shana Labed
October 30, 2025 AT 16:44OMG YES. I saw 'poorly controlled DM' in my portal and cried. Like I’m some lazy failure? No. I’m working 60-hour weeks, sleeping 4 hours, and still taking my meds. That label feels like a punch. But now I know it’s just code - not a verdict. Thank you for saying this out loud.
California Daughter
October 31, 2025 AT 07:28Wait… so… you’re saying… doctors… are… lazy…? And… we… should… just… ignore… the… codes…? Because… I… think… they… exist… for… a… reason…? Like… maybe… not… everyone… should… get… to… decide… what… their… diagnosis… is… called…? Just… saying…
Vishwajeet Gade
November 1, 2025 AT 00:37USA always whining. In India, we don't care about labels. We just take medicine. Doctor says 'diabetes' we say 'haan sahab' and move on. Why you need plain English? You think you are smart? I work in hospital, I see your kind. Always typing on phone, never listening.
Casey Crowell
November 1, 2025 AT 23:27This is why I love healthcare tech so much. 🤖❤️ Imagine a world where your EHR doesn't just dump codes on you - it whispers, 'Hey, this is what's going on, and here's how we fix it.' No shame. No jargon. Just clarity. We're not dumb. We just need to be spoken to like humans. And honestly? This is the future. It's already here in places like Kaiser. We just gotta push harder.
Shanna Talley
November 3, 2025 AT 23:05It’s not about dumbing things down. It’s about meeting people where they are. If your doctor uses words that make you feel stupid, that’s not professionalism - that’s a communication breakdown. Your story matters. Your experience is data too. Write it down. Bring it in. You’re not just a code. You’re a person.
Samuel Wood
November 5, 2025 AT 20:12Frankly, I find this entire discussion a bit… quaint. The medical system operates on precision, not sentiment. If you can't parse ICD-10, perhaps you shouldn't be entrusted with your own health data. The fact that patients feel 'traumatized' by clinical terminology speaks more to societal infantilization than systemic failure. I mean, really - do we now need a glossary for 'hypertension'?
Jacqueline Anwar
November 6, 2025 AT 04:48While I appreciate the sentiment, the notion that patients require 'plain language' versions of their diagnoses implies a fundamental lack of intellectual capacity among the general population. Medical terminology is not an elitist construct - it is a standardized, scientifically rigorous language. To dilute it for comfort's sake is to undermine the integrity of clinical practice. One cannot expect to navigate quantum physics in emoji.
Ganesh Kamble
November 8, 2025 AT 03:26lol this whole post is just woke healthcare theater. Doctors are busy. They don't have time to write novels. If you can't read your own chart, that's your problem. Stop blaming the system. Also, why are we even talking about this? Nobody cares.
Jenni Waugh
November 8, 2025 AT 23:20Oh honey. Let me tell you about my last visit. My doctor wrote 'anxiety disorder' - I thought it meant I was a bad person. Then I Googled it. Turns out it's not a moral failing. It's a chemical imbalance. So I asked her to write 'your brain is tired' next time. She rolled her eyes. But she did it. And I cried. Not because I'm weak - because someone finally saw me.
Theresa Ordonda
November 9, 2025 AT 22:37Ugh. I’ve been saying this for years. People think 'poorly controlled' means they're failing. It doesn't. It means the system failed them. They didn't get the right support. The right education. The right follow-up. But instead of fixing that, we blame the patient. And now they feel guilty for being sick. That's not healthcare. That's punishment wrapped in a stethoscope. 💔
Judy Schumacher
November 10, 2025 AT 11:25Let’s be real - this isn’t about language. It’s about power. The medical establishment has spent decades hoarding knowledge like a dragon with gold. Now that patients can see the gold, they’re asking, 'Why didn’t you just show me this before?' And suddenly, the dragons are mad. The real revolution isn’t plain language - it’s transparency. And that terrifies them.
Megan Raines
November 10, 2025 AT 13:36Interesting. So if I read 'E11.9' and panic, is that my fault? Or is it the system’s job to make sure I don’t panic? I mean… if a sign says 'Exit' in 12 languages but I only speak English… who’s at fault? The sign? Or me?
Mamadou Seck
November 11, 2025 AT 01:35Doctors use codes because they’re faster. Plain language takes time. Time = money. Money = profit. You think this is about care? Nah. It’s about billing. But hey, at least we’re pretending now. Progress?
Anthony Griek
November 12, 2025 AT 11:42I’m a nurse. I see this every day. A woman came in crying because her note said 'noncompliant.' She hadn’t missed a dose. She just forgot to write it down. We changed it to 'needs support with medication tracking.' She hugged me. That’s not fluff. That’s care. Simple changes save lives.
Norman Rexford
November 12, 2025 AT 13:33Y’all are overthinking this. Just ask your doctor what the words mean. They’re not hiding anything. They’re just busy. Also, ICD-10 is not a conspiracy. It’s a code. Like a password. You don’t need to know how the internet works to use Google. Same here. Chill.