Spotting Ulcer Symptoms and Early Warning Signs: A Complete Guide
 Oct, 15 2025
Oct, 15 2025
Ulcer Symptom Checker
Check Your Symptoms
This tool helps you assess common ulcer symptoms. It's not a diagnosis but can help determine if you need to see a doctor.
Answer the questions above to see your assessment results.
Many people think a stomach ache is just indigestion, but it could be the first clue that an ulcer is forming. Knowing the ulcer symptoms and the subtle warning signs can mean the difference between a quick fix and a serious health issue.
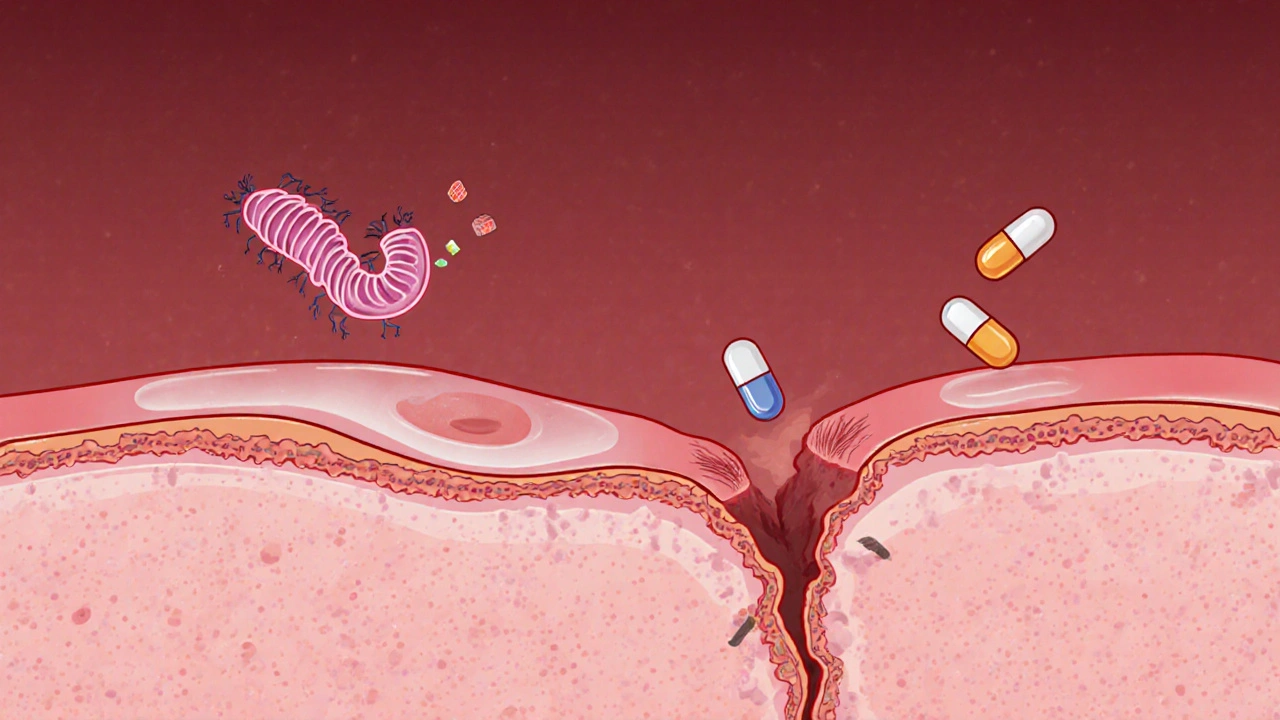
What exactly is an ulcer?
Ulcer is a break in the lining of the digestive tract that exposes tissue to stomach acid and digestive enzymes. Most ulcers develop in the stomach (stomach ulcer) or the first part of the small intestine (duodenal ulcer) and together they’re called peptic ulcer disease.
Ulcers aren’t rare. According to the World Health Organization, over 10% of the world’s population will experience a peptic ulcer at some point.
How does an ulcer form?
The stomach normally protects itself with a thick mucus layer and a steady flow of bicarbonate that neutralizes acid. When this protective barrier is weakened, acid starts chewing away at the tissue.
- Helicobacter pylori is a spiral‑shaped bacteria that lives in the stomach lining and is the leading cause of ulcer formation.
- Nonsteroidal anti‑inflammatory drugs (NSAIDs) such as ibuprofen, aspirin, and naproxen inhibit prostaglandins, which helps keep the stomach lining intact.
- Excessive gastric acid production, often triggered by stress, smoking, or heavy alcohol use, can overwhelm the mucus barrier.
When the lining is breached, the exposed tissue inflames, bleeds, and eventually creates a painful sore.
Early warning signs you shouldn’t ignore
Before a full‑blown ulcer pain appears, the body may toss up subtle signals:
- Sudden, gnawing hunger after meals - the ulcer may be trying to signal that it’s not digesting food properly.
- Unexplained weight loss - a sore can reduce appetite and cause you to eat less.
- Night‑time discomfort that wakes you up - acid that sits while you lie down can irritate the ulcer.
- Black or tar‑like stools (melena) - a sign of slow bleeding inside the digestive tract.
- Vomiting blood or material that looks like coffee grounds - an urgent red flag indicating active bleeding.
If any of these appear, it’s time to see a health professional, even if the pain feels mild.

Typical ulcer symptoms
| Symptom | How Often It Shows Up | Why It Happens |
|---|---|---|
| Burning or gnawing pain in the upper abdomen | After meals or when the stomach is empty | Acid contacts the exposed ulcer surface |
| Bloating and belching | Throughout the day | Delayed gastric emptying caused by inflammation |
| Nausea or occasional vomiting | Occasional | Stomach irritation and spasms |
| Loss of appetite | Variable | Discomfort discourages eating |
| Red‑flag: Black stools | Rare but serious | Slow bleeding that mixes with digestive enzymes |
| Red‑flag: Vomiting blood | Rare but emergent | Active bleeding from the ulcer |
The first four rows are what most patients call “ulcer symptoms.” The last two rows are warning signals that demand immediate medical attention.
When to seek professional help
If you notice any red‑flag signs-black stools, vomiting blood, sudden sharp pain that doesn’t ease with antacids, or unexplained weight loss-call your doctor right away. Even persistent dull pain that lingers for weeks should be evaluated, because untreated ulcers can lead to perforation or serious bleeding.
How doctors diagnose an ulcer
Diagnosis typically involves a combination of history, physical exam, and tests:
- endoscopy is the gold‑standard procedure; a thin camera looks directly at the stomach lining and can also take a biopsy.
- Breath or stool tests for H. pylori detect the bacteria’s presence without invasive methods.
- Blood tests can reveal anemia caused by chronic bleeding.
- Imaging (CT scan) may be used if a perforation is suspected.
Once the diagnosis is confirmed, the doctor will decide on treatment based on the ulcer’s cause and severity.
Managing and preventing ulcer flare‑ups
Most ulcers heal within 4-8 weeks with the right therapy. Here’s a practical plan:
- Eradicate H. pylori if present. A typical regimen includes two antibiotics (clarithromycin and amoxicillin) plus a proton‑pump inhibitor (PPI) for two weeks.
- Reduce acid load. PPIs (omeprazole, lansoprazole) or H2‑blockers (ranitidine, famotidine) lower stomach acid, giving the ulcer a chance to mend.
- Stop or limit NSAIDs. Switch to acetaminophen for pain, or ask your doctor about a protective agent like misoprostol.
- Adopt ulcer‑friendly habits.
- Eat smaller, balanced meals; avoid spicy, fatty, or highly acidic foods.
- Quit smoking-nicotine impairs healing.
- Limit alcohol; it irritates the stomach lining.
- Manage stress through gentle exercise, meditation, or counseling.
Regular follow‑up appointments ensure the ulcer is closing properly and help catch complications early.
Quick self‑check checklist
- Do you feel a burning pain that improves after eating? - Possible ulcer symptom.
- Do you notice bloating, early satiety, or nausea? - Common but not exclusive to ulcers.
- Have you seen black stools or vomited blood? - Seek emergency care.
- Are you taking NSAIDs daily or have you been diagnosed with H. pylori? - Talk to your doctor about testing and treatment.
If you tick any red‑flag boxes, book an appointment now. Early detection makes treatment easier and prevents complications.
Frequently Asked Questions
Can stress alone cause an ulcer?
Stress increases stomach acid and can slow healing, but on its own it rarely creates a full ulcer. Most ulcers involve H. pylori infection or NSAID use, with stress acting as a worsener.
Are coffee and tea bad for ulcer patients?
Caffeinated drinks stimulate acid production, so they can aggravate symptoms. Decaf or herbal teas are safer choices while the ulcer heals.
How long does it take for an ulcer to heal?
With proper medication and lifestyle changes, most ulcers close in 4 to 8 weeks. Follow‑up endoscopy may be done to confirm healing in complicated cases.
Is it safe to take antacids while on PPIs?
Generally yes; antacids provide quick relief, while PPIs work longer‑term. However, avoid taking them simultaneously-space them at least 30 minutes apart.
Can ulcers come back after treatment?
Recurrence is possible, especially if the underlying cause (like H. pylori or chronic NSAID use) isn’t addressed. Maintaining ulcer‑friendly habits reduces the risk dramatically.

Alyssa Griffiths
October 15, 2025 AT 13:11Look, the medical industry has been pushing proton‑pump inhibitors like candy, and they don’t want us to notice the subtle side‑effects, because profit, profit, profit! The ulcer guide is helpful, but you must also question why your doctor prescribes a drug that can mask symptoms while the real cause-H. pylori or NSAIDs-remains untreated. Remember, the mucus barrier is a natural defense, not a product you can buy at a pharmacy. If you’re constantly on antacids, you might be fueling a covert agenda to keep you hooked on medication. Stay vigilant, read the fine print, and consider natural healing methods.
dany prayogo
October 23, 2025 AT 15:14Ah, the classic peptic ulcer-nature's way of reminding us that we can't just binge on coffee and ignore the warning signs, right? First, let’s acknowledge that the guide does a decent job of outlining symptoms, but it completely sidesteps the fact that most of us are already nursing a diet of processed junk that practically mines our stomach lining for profit. Secondly, while helicobacter pylori is mentioned as the leading cause, the real kicker is that the pharmaceutical companies conveniently downplay lifestyle factors to keep the market for antibiotics and PPIs alive. Thirdly, those “black stools” aren’t just a scary headline; they’re a literal bleed‑off that could land you in an emergency room that’s already overrun with patients who ignore basic health advice. Fourth, the recommendation to “stop NSAIDs” is adorable-who would ever think about that when you’ve been told that ibuprofen is the miracle cure for everything from headaches to heartbreak? Fifth, the guide’s advice to “limit alcohol” sounds reasonable, until you consider that social norms and advertising make a glass of wine feel like a prerequisite for adulthood. Sixth, stress is brushed off as a minor aggravator, yet modern life is a pressure cooker designed to keep us perpetually anxious, and that anxiety translates directly into acid overproduction. Seventh, the checklist at the end is nice, but it’s basically a self‑diagnosis tool that encourages laypeople to play doctor-a dangerous game when the real experts are conveniently out of reach due to insurance nightmares. Eighth, the emphasis on “quick relief” with antacids subtly nudges us toward over‑the‑counter solutions that only mask pain while the ulcer silently worsens. Ninth, let’s not forget the socioeconomic angle: poorer communities get less access to endoscopy, meaning many ulcers go undiagnosed until catastrophe strikes. Tenth, the suggested “follow‑up appointments” sound like a polite reminder that you’ll need to spend more money on healthcare, because the ulcer won’t just disappear on its own. Eleventh, the notion that “most ulcers heal in 4‑8 weeks” smacks of optimism brewed in a lab full of profit‑driven research. Twelfth, the guide’s tone feels like it’s written by someone who’s never actually experienced that gnawing, midnight pain that throws you out of bed. Thirteenth, the avoidance of discussing diet specifics beyond “avoid spicy” is a missed opportunity to empower readers with real culinary alternatives. Fourteenth, the brief mention of “meditation” as a stress‑relief tool feels tokenistic when there’s no guidance on actual practices. Finally, while the guide is comprehensive on the surface, it leaves out the uncomfortable truth: the healthcare system benefits from our chronic reliance on medication, and it’s up to us to break free from that cycle.
Wilda Prima Putri
October 31, 2025 AT 16:18Okay, you’ve got the basics down, so just keep an eye on what you eat and try not to stress too much. Small meals are easier on the gut, and if you’re feeling off, give your body a break. Remember, you don’t have to go full‑on guru mode to stay healthy.
Sharif Ahmed
November 8, 2025 AT 18:22One must concede that the prose of the guide aspires to the lofty heights of a medical textbook, yet it flirts with melodrama in equal measure. The ulcer, a mere erosion, is painted as an epic villain, an adversary worthy of Shakespearean tragedy. Such dramatization, while captivating, may obscure the pragmatic steps a layperson ought to adopt. Nonetheless, the emphasis on eradication of H. pylori and the judicious use of PPIs is commendable, aligning with contemporary gastroenterological consensus. In sum, the guide straddles the line between scholarly exposition and theatrical flourish, a balancing act that, if refined, could serve both the educated and the curious alike.
Chelsea Kerr
November 16, 2025 AT 20:25Ulcers remind us that the body is a delicate ecosystem 🌱. Treating the root cause, whether it’s H. pylori or chronic NSAID use, respects that balance. Remember to hydrate, nourish with gentle foods, and give yourself moments of calm 😊. Healing is a journey, not a sprint.
Tom Becker
November 24, 2025 AT 22:29Yo, don't trust those big pharma pills they push, they're just keepin' you sicker longer. The ulcer's real enemy is the hidden chemicals in the meds, not the stress you think. I read some forum say the cure is honey and ginger, defintely better than a bottle of pills. Stop the lie, start the heal!
Laura Sanders
December 3, 2025 AT 00:32The guide is accurate, but let’s be clear: ulcers are caused by more than just bacteria. Lifestyle changes are essential – cut back on NSAIDs, avoid late‑night coffee, and monitor stress levels. Remember, knowledge is power; don’t rely solely on medication.
Jai Patel
December 11, 2025 AT 02:36Namaste! In India we’ve long used turmeric and cumin to soothe the stomach, and they work wonders when paired with mindful eating. Try incorporating a warm ginger‑lemon tea after meals; it eases digestion and reduces inflammation. And don’t forget a short walk – it aids gastric motility while lifting your spirit.
Zara @WSLab
December 19, 2025 AT 04:40Great guide! If you’re unsure about the symptoms, keep a daily log of meals and any discomfort – it helps your doctor pinpoint the issue faster. Also, stay hydrated; water is a simple yet powerful ally. 🌟
Randy Pierson
December 27, 2025 AT 06:43Keeping a symptom diary is a solid move for troubleshooting ulcers.
Bruce T
January 4, 2026 AT 08:47Look, ignoring ulcer warning signs because you think “it’s just a stomachache” is reckless. We have a responsibility to ourselves to take health seriously, not brush it off with jokes. If you’re popping NSAIDs for every ache, you’re practically inviting trouble. Let’s be honest-taking care of our bodies is the first step toward being decent human beings.
Darla Sudheer
January 12, 2026 AT 10:50That’s solid advice; staying on top of symptoms can prevent bigger issues. I’d add that regular check‑ups are key, even if you feel fine. Keep it simple and stay safe.
Elizabeth González
January 20, 2026 AT 12:54The systematic approach outlined in the guide reflects a commendable dedication to patient education. Its thoroughness in distinguishing routine symptoms from red‑flag warnings is particularly noteworthy. However, a more nuanced discussion of socioeconomic barriers to endoscopic access would enhance its applicability. Overall, the composition balances clinical precision with accessible language, a laudable achievement.
Sebastian Samuel
January 28, 2026 AT 12:11Listen, the ulcer guide is decent, but you need to own your health-no more sitting on the sidelines. 🙅♂️ If you’re on NSAIDs, ditch them ASAP, and if you’re stressed, find a hobby that actually distracts you. 😈 Remember, the body will betray you if you treat it like an after‑thought. 🚀