Statins and Sleep Disturbances: Can Cholesterol Medication Cause Insomnia and Vivid Dreams?
 Nov, 6 2025
Nov, 6 2025
When you're taking a statin to protect your heart, the last thing you expect is to lie awake at night with bizarre, lifelike dreams. Yet thousands of people report exactly this: trouble falling asleep, waking up multiple times, or being jolted awake by dreams so vivid they feel real. Is it the statin? Or is it something else?
Statins Are Everywhere - But So Are Sleep Complaints
Statins like simvastatin, atorvastatin, and rosuvastatin are among the most prescribed drugs in the world. Over 300 million people take them annually to lower LDL cholesterol and reduce heart attack risk. For most, they work without a hitch. But for a noticeable chunk - maybe 5% to 10% - something odd happens: sleep falls apart. You might not think much of a bad night’s sleep. But when it’s happening every night for weeks? When you’re dreaming about falling off cliffs or reliving your high school graduation in full color? That’s not just stress. That’s a pattern. And here’s the twist: not all statins are the same when it comes to sleep. Some seem to trigger these issues. Others don’t. Why? It comes down to chemistry.Lipophilic vs. Hydrophilic: The Real Difference
Statins fall into two camps: lipophilic (fat-soluble) and hydrophilic (water-soluble). Lipophilic statins - like simvastatin, lovastatin, and atorvastatin - can cross the blood-brain barrier more easily. That means they can reach brain tissue, where they might interfere with chemicals involved in sleep regulation. Hydrophilic statins - like pravastatin and rosuvastatin - mostly stay in the bloodstream. They don’t enter the brain as readily. And guess what? Studies show people on these tend to report fewer sleep problems. Take the 2007 study by Dr. Beatrice Golomb. She gave 1,016 people either simvastatin, pravastatin, or a placebo. Those on simvastatin reported significantly worse sleep quality. Those on pravastatin? No difference from placebo. It wasn’t the statin class. It was the specific type. Later, researchers analyzed millions of adverse event reports from the FDA and Japan. Simvastatin showed up in sleep disturbance reports at more than double the rate of other statins. Rosuvastatin? Moderate risk. Atorvastatin? Nearly no link. So if you’re on simvastatin and having vivid dreams or insomnia, it’s not in your head. It’s in the molecule.But Some Studies Say Statins Don’t Affect Sleep
Wait - didn’t a huge 2018 study say statins actually improve sleep? Yes. And that’s where things get messy. That study, led by Professor Colin Baigent, followed 10,000 people on atorvastatin versus placebo. The statin group reported fewer sleep problems than the placebo group. How? Researchers think it’s the nocebo effect. The nocebo effect is the opposite of placebo. If you hear that a drug causes insomnia, you start noticing every night you toss and turn - and blame the pill. You might even stop sleeping well because you’re anxious about it. But here’s the catch: that study used atorvastatin - a statin with low brain penetration. It’s not the same as simvastatin. So the results don’t cancel out the other data. They just show context matters. And then there’s the muscle connection.It Might Not Be the Brain - It’s the Muscles
A 2024 study by Dr. L. Graves found something surprising: people with statin-associated muscle symptoms (SAMS) - aches, weakness, cramps - also had terrible sleep. When they stopped the statin, their sleep improved. Not because the drug left their brain. But because their muscles stopped hurting. Nighttime muscle pain? That keeps you awake. Restless legs? That disrupts deep sleep. Poor sleep from pain looks just like sleep disruption from brain chemistry. And many doctors miss the link. So if you’re on simvastatin and your legs ache at night, your dreams are wild, and you’re exhausted - it might not be the statin messing with your REM cycle. It might be your muscles screaming for relief.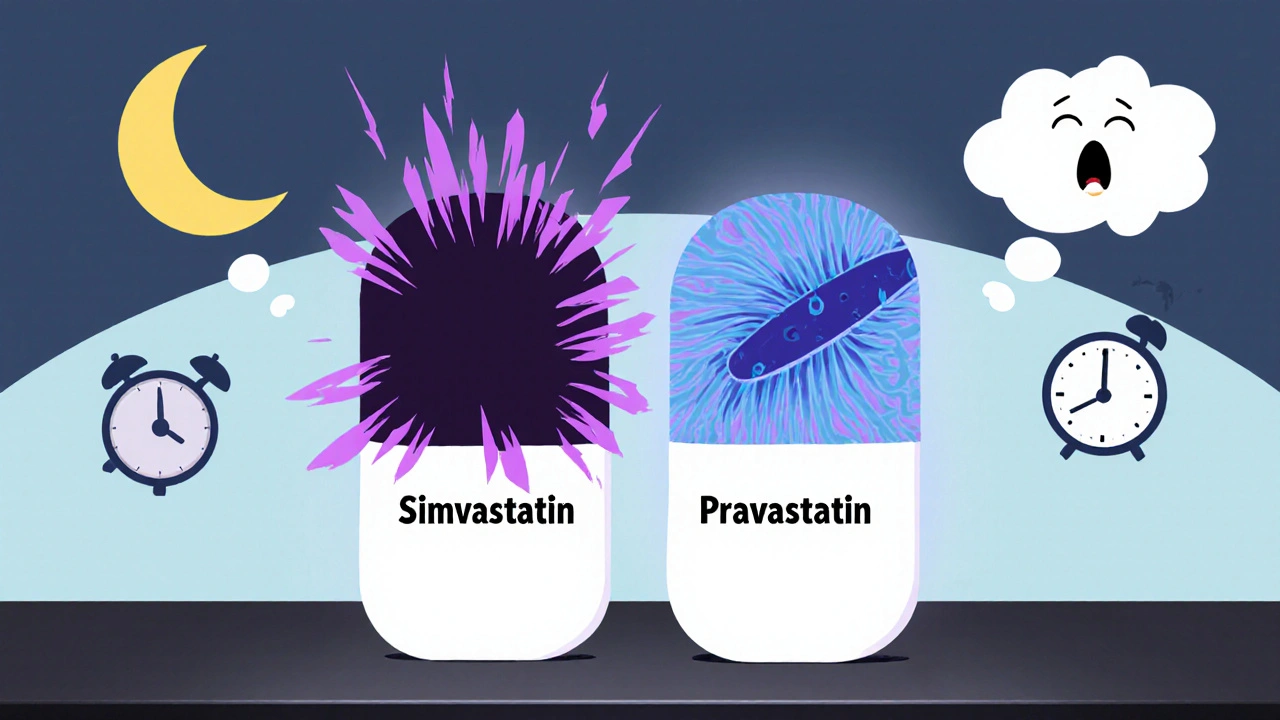
What Should You Do If Sleep Gets Worse?
Don’t stop your statin on your own. Heart risk doesn’t wait. Instead, try this:- Track your sleep. For two weeks, write down when you go to bed, when you wake up, how many times you wake, and whether your dreams were vivid. Use a simple app or notebook.
- Check your statin. Are you on simvastatin or lovastatin? Those are the usual suspects. Atorvastatin and pravastatin? Much less likely.
- Talk to your doctor about switching. If you’re on simvastatin, ask about switching to pravastatin or rosuvastatin. Many people report sleep improvements within 10-14 days.
- Consider timing. Some people find taking their statin in the morning instead of at night helps - even if it’s lipophilic. Why? Less drug in your system when you’re trying to sleep.
- Rule out other causes. Stress, caffeine after 2 p.m., screen time before bed, or sleep apnea can all mimic statin-related sleep issues.
Real Stories: What People Are Saying
One Reddit user wrote: “Switched from atorvastatin to pravastatin. My crazy dreams stopped the next week. I didn’t even know they were that bad until they were gone.” Another: “Took simvastatin for five years. Never had a sleep problem. So much for the horror stories.” And another: “I thought I was going crazy. Woke up screaming from dreams about my dead dog. Stopped the statin. Slept like a baby. My doctor said it was probably the drug.” These aren’t rare. They’re common enough that the British Heart Foundation now tells doctors to ask about sleep when starting statins.The Bottom Line: It’s Personal
There’s no blanket answer. For some, statins are sleep killers. For others, they’re harmless. For a few, they might even help. What matters is this: if you’re sleeping poorly after starting a statin - especially simvastatin or lovastatin - it’s worth investigating. Don’t assume it’s just stress. Don’t assume it’s all in your head. And don’t assume switching statins will fix everything. But here’s what you can do right now: talk to your doctor. Ask if your statin is lipophilic. Ask if a switch might help. Ask about muscle pain. Ask about sleep tracking. Your heart needs protection. But so does your sleep. And you don’t have to choose one over the other.
What If Switching Doesn’t Help?
If you switch from simvastatin to pravastatin and your sleep doesn’t improve, it’s likely not the statin at all. Consider these:- Are you drinking alcohol before bed? It fragments sleep.
- Do you use your phone in bed? Blue light suppresses melatonin.
- Have you been under stress? Anxiety is a silent sleep thief.
- Do you snore or wake up gasping? Sleep apnea is common and often undiagnosed.
What About Vivid Dreams? Are They Dangerous?
Vivid dreams aren’t harmful. But they can be unsettling - especially if they’re frightening or feel real. The good news? They usually fade once you stop the statin or switch to a different one. In most cases, they’re not a sign of mental illness. Just a side effect of brain chemistry shifting. If the dreams are causing anxiety or you’re afraid to sleep, tell your doctor. There are short-term strategies - like relaxation techniques or cognitive behavioral therapy - that can help you feel safe again.Final Thought: Don’t Let Fear Stop Your Heart Protection
Statins reduce heart attacks by 22% for every 1 mmol/L drop in LDL. That’s huge. For someone with high cholesterol or a history of heart disease, the benefits far outweigh the risks - even if sleep gets worse. But that doesn’t mean you have to suffer. Millions take statins and sleep just fine. And if yours isn’t one of them? There’s a solution. It’s not about avoiding statins. It’s about finding the right one for you.Can statins cause insomnia and vivid dreams?
Yes, some statins - especially lipophilic ones like simvastatin and lovastatin - have been linked to insomnia and vivid dreams in certain people. Research shows these effects are more common with statins that can cross the blood-brain barrier. Not everyone experiences this, and hydrophilic statins like pravastatin are far less likely to cause sleep issues.
Which statin is least likely to cause sleep problems?
Pravastatin and pitavastatin are the least likely to cause sleep disturbances because they are hydrophilic and don’t cross into the brain easily. Rosuvastatin has a moderate risk, while simvastatin and lovastatin carry the highest risk based on clinical and adverse event data.
Should I stop taking my statin if I have bad dreams?
No. Stopping statins without medical advice can increase your risk of heart attack or stroke. Instead, talk to your doctor. They can help you switch to a different statin or investigate other causes like muscle pain, stress, or sleep apnea.
How long does it take for sleep to improve after switching statins?
Most people notice improvement within 10 to 14 days after switching to a different statin. In some cases, especially if muscle pain was contributing to poor sleep, it may take up to 4 weeks for full recovery.
Is there a test to prove statins are causing my sleep issues?
There’s no blood test or scan to confirm it. Diagnosis is based on timing - did sleep problems start after beginning the statin? Did they improve after switching? Doctors rely on this pattern, along with ruling out other causes like anxiety or sleep apnea.
Can taking statins in the morning help with sleep?
Yes, some people find that taking their statin in the morning instead of at night helps reduce sleep disturbances. This is especially true for lipophilic statins, as it reduces drug concentration in the body during nighttime hours when sleep is most vulnerable.
Are vivid dreams from statins dangerous?
No, vivid dreams themselves are not dangerous. They’re a side effect, not a sign of mental illness. However, if they cause anxiety, fear of sleeping, or daytime fatigue, talk to your doctor. Strategies like relaxation techniques or a short course of cognitive behavioral therapy can help you feel safe again.

Abigail Chrisma
November 7, 2025 AT 20:00I switched from simvastatin to pravastatin last year after months of waking up screaming from dreams about my ex-husband driving a tractor into our living room. Like, full color, sound effects, the whole cinematic disaster. Didn’t even realize how bad it was until it vanished. Now I sleep like a log. Also, took my statin in the morning after reading this - total game changer. No more 3 a.m. existential dread.
Edward Weaver
November 9, 2025 AT 04:30LMAO you people are so weak. Statins save lives. If you can’t sleep because your brain is overactive from finally having decent cholesterol, that’s your problem. I’ve been on atorvastatin for 12 years and dream about winning the lottery and punching Trump. That’s not a side effect - that’s progress. Stop blaming medicine for your anxiety.
Lexi Brinkley
November 10, 2025 AT 02:24OMG SAMEEEE 😱 I was on simvastatin and started dreaming I was being chased by a giant avocado. Like, full-on horror movie vibes. I thought I was losing it. Switched to pravastatin and now I dream about cats wearing tiny hats 🐱🎩. Life is good again. Also, morning dose = magic. 💪
Kelsey Veg
November 11, 2025 AT 21:11idk why ppl are making such a big deal. i took simvastatin for 3 years and never had a problem. maybe its just people who are already anxious and then they read online and start thinking about it and then boom insomnia. its all in the head. also i spell weird because i type fast and dont care lol
Alex Harrison
November 12, 2025 AT 06:47My dad had the same thing. He was on simvastatin, started having nightmares about falling down stairs, couldn’t get back to sleep. We called his doc, switched to rosuvastatin, and within two weeks he was sleeping 8 hours straight. He didn’t even know how tired he’d been. Also, he started taking it in the morning and that helped too. Don’t ignore it - it’s not just stress. It’s real.
Jay Wallace
November 13, 2025 AT 08:33Let me be perfectly clear: the notion that a lipophilic statin could cross the blood-brain barrier and modulate GABAergic or serotonergic pathways - while theoretically plausible - is not robustly supported by double-blind, placebo-controlled, multi-center trials with adequate statistical power. The FDA’s FAERS database is riddled with confounders - age, comorbidities, polypharmacy - and yet, somehow, Reddit has become the de facto arbiter of pharmacovigilance? Absurd. Also, you’re all mispronouncing ‘hydrophilic.’ It’s hy-dro-FIL-ic, not hy-dro-FILL-ic. 🤦♂️
Alyssa Fisher
November 15, 2025 AT 08:16What’s fascinating isn’t just the pharmacology - it’s the way we assign meaning to bodily experiences. We’re told statins cause insomnia, so we start noticing every restless night. But what if the real issue is the fear of the side effect itself? The nocebo effect isn’t just psychological - it’s biological. Cortisol spikes, melatonin drops, sleep architecture fractures. The drug might not be the villain. Our belief in its villainy might be. And yet… the clinical data on simvastatin and vivid dreams? Too consistent to ignore. So we’re caught between biology and belief. Which one do we trust when both are screaming?
Alyssa Salazar
November 16, 2025 AT 01:37Okay, but let’s talk about the muscle connection - that’s the real kicker. Statin-associated myopathy isn’t just about soreness - it’s about micro-inflammation and mitochondrial dysfunction. Those nighttime cramps? They trigger sympathetic nervous system activation. That’s why sleep gets shredded. And here’s the kicker: many patients don’t even connect the dots because their doctor doesn’t ask about muscle symptoms. We need better screening protocols. We need to stop treating sleep complaints as ‘psychosomatic’ when they’re often somatopsychic. It’s not either/or - it’s both. And we’re missing the forest for the trees.