Antacids and Antibiotics: How to Time Your Doses to Avoid Treatment Failure
 Dec, 29 2025
Dec, 29 2025
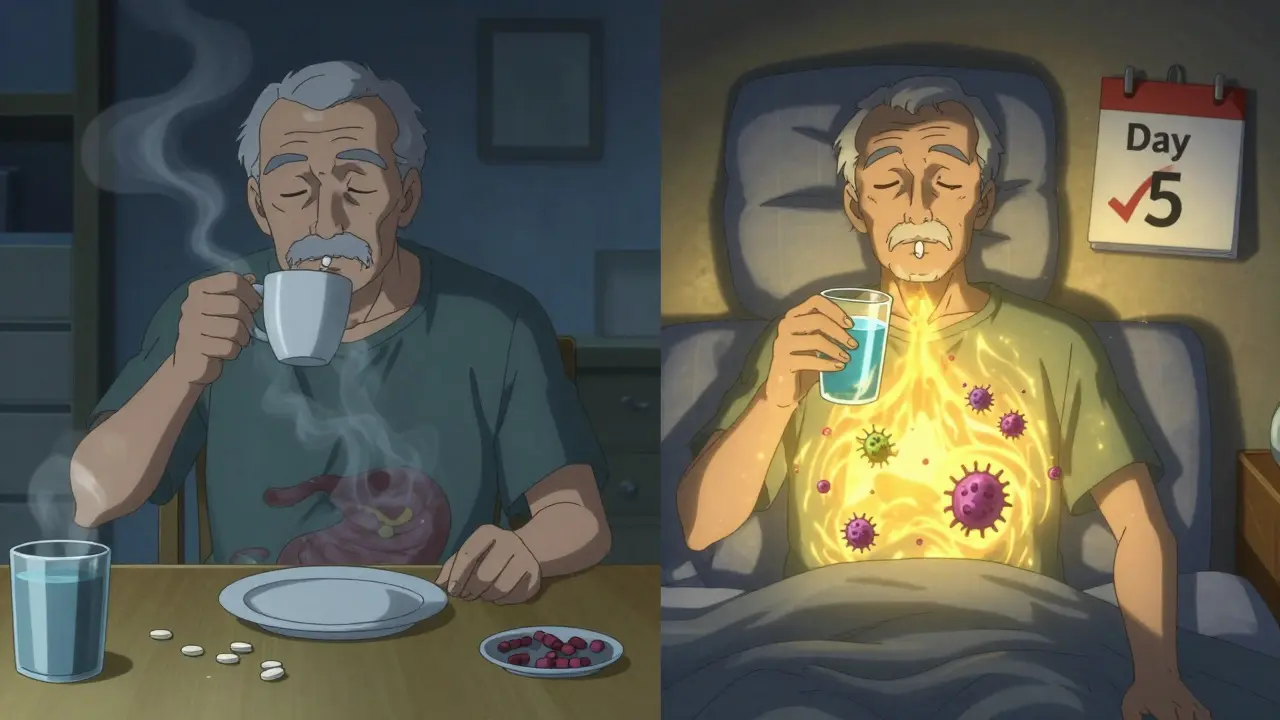
Every year, millions of people take antibiotics for infections - and nearly one in three also reach for an antacid for heartburn or upset stomach. But if you take them at the same time, your antibiotic might not work. Not because it’s broken. Not because you’re sick in a way the drug can’t fix. But because the antacid is blocking it from getting into your bloodstream.
Why Antacids Can Ruin Your Antibiotic
Antacids like Tums, Rolaids, Maalox, and Mylanta contain aluminum, magnesium, or calcium. These minerals don’t just neutralize stomach acid - they also bind tightly to certain antibiotics, forming a kind of chemical cage. Once that happens, your body can’t absorb the antibiotic. It just passes through you, useless.This isn’t a myth. It’s been proven in labs and clinics for decades. In the 1970s, researchers at UC San Francisco found that tetracycline, a common antibiotic back then, lost nearly half its power when taken with antacids. Today, we know the same thing happens with ciprofloxacin, levofloxacin, doxycycline, and others.
Take ciprofloxacin, for example. If you swallow it right after a Tums, your body absorbs up to 90% less of the drug. That means instead of killing the bacteria in your urinary tract or lungs, you’re giving them a free pass to multiply. And that’s how treatment fails - not because the antibiotic is weak, but because you took it at the wrong time.
Which Antibiotics Are Most Affected?
Not all antibiotics are equally vulnerable. The risk depends on the drug’s chemical structure. Here’s what you need to know:- Fluoroquinolones (ciprofloxacin, levofloxacin, moxifloxacin): These are the most sensitive. Antacids can slash absorption by 75-90%. Even a small delay can make a big difference.
- Tetracyclines (doxycycline, tetracycline): Also highly affected. Absorption drops by 50-70%. This includes doxycycline, often prescribed for acne or Lyme disease.
- Macrolides (azithromycin, clarithromycin): Less affected, but still worth spacing out. A 2-hour gap is recommended just to be safe.
- Beta-lactams (amoxicillin, cephalexin): These are the exceptions. They lose only 15-20% absorption with antacids. Still, it’s better to avoid taking them together.
- Metronidazole: No meaningful interaction. You can take it with antacids without worry.
If you’re on ciprofloxacin or doxycycline, treat your antacid like a poison - not to be mixed. For amoxicillin, it’s more of a nuisance than a danger. But if you’re immunocompromised, even a 15% drop matters.
How Far Apart Should You Take Them?
Timing isn’t about minutes - it’s about hours. And the gap depends on the antibiotic.The safest rule across the board: Take antibiotics at least 2 hours before or 4 hours after an antacid. This is the recommendation from the FDA, NHS, and Cleveland Clinic. Why the difference?
For fluoroquinolones like ciprofloxacin, you need the full 4-hour buffer. The minerals in antacids cling to the drug so strongly that even 2 hours isn’t enough. For doxycycline, 2-3 hours works. But if you’re unsure, go with 4 hours. It’s safer.
Here’s a simple schedule if you take antibiotics twice a day:
- 7 AM: Take antibiotic
- 11 AM: Take antacid (if needed)
- 3 PM: Take antibiotic
- 7 PM: Take antacid (if needed)
If you take your antibiotic at night, reverse it:
- 7 PM: Take antibiotic
- 11 PM: Take antacid
- 7 AM: Take antibiotic
- 11 AM: Take antacid
Don’t wait until you feel heartburn to take the antacid. Plan ahead. If you know you get acid reflux after meals, take your antibiotic at least 2 hours before eating - then take your antacid after.
What About Other Acid Reducers?
Antacids aren’t the only thing that changes your stomach’s pH. H2 blockers (famotidine, ranitidine) and proton pump inhibitors (omeprazole, pantoprazole) also reduce acid - but they don’t contain aluminum or magnesium. That means they don’t chelate antibiotics.Studies show that switching from antacids to omeprazole cuts treatment failure rates by more than half in patients needing both antibiotics and acid control. If you’re on long-term acid-reducing therapy, ask your doctor if you can switch. It’s a simple fix that avoids the whole timing problem.
Real Stories: When Timing Made the Difference
A woman in Atlanta kept getting urinary tract infections. Her doctor prescribed ciprofloxacin three times. Each time, the infection came back. She didn’t think anything of taking her Tums with the pill - it helped her stomach feel better. Only when her pharmacist asked, “Do you take antacids with your antibiotics?” did the puzzle click. She started taking the antibiotic 4 hours before any antacid. The fourth round worked. She hasn’t had another UTI in 11 months.On Reddit, a medical student shared that her grandfather, on doxycycline for a skin infection, gave up after two weeks because “it wasn’t working.” He was taking his antacid at breakfast, and his antibiotic at lunch. The pharmacist told him to take the antibiotic at bedtime, 4 hours after his last antacid. His rash cleared up in 5 days.
These aren’t rare. A 2023 review of patient reviews on Drugs.com found that 68% of people who reported antibiotic failure saw results improve - once they fixed their timing.
Why Do People Keep Getting This Wrong?
It’s not laziness. It’s confusion.Most people don’t know the difference between antacids and other acid reducers. They think “anything that helps heartburn” is the same. They take their antibiotic with breakfast, and their Tums right after. Or they’re on a busy schedule and forget.
Doctors don’t always explain it clearly. A 2023 CMS audit found that only 63% of antibiotic prescriptions included timing instructions for antacids. That means nearly 4 out of 10 patients are left guessing.
And it’s worse for older adults. Someone on five medications already? Adding a 4-hour gap between two of them feels impossible. That’s why tools like MyMedSchedule apps and visual pill timers are becoming essential. One Mayo Clinic study showed that giving patients a printed chart with colored time blocks cut timing errors by 37%.

What’s New in 2025?
The science is evolving. In 2023, the FDA approved a new version of ciprofloxacin called Cipro XR-24. It’s designed to release slowly so it’s less affected by antacids. In trials, it lost only 8% absorption - compared to 90% for the old version. It’s not widely available yet, but it’s a sign of where things are headed.Also, new guidelines from the American Society of Health-System Pharmacists now distinguish between types of antacids. Calcium-based ones (like Tums) need 4 hours separation. Magnesium-based ones (like Maalox) can be spaced at 2 hours. That’s more precise - and more useful.
Even more exciting? Researchers at the University of Pittsburgh found that your genes affect how fast your stomach empties. In the future, your doctor might use a simple genetic test to tell you whether you need 2 hours or 6 hours between doses. Personalized timing is coming.
What You Can Do Today
You don’t need to wait for new drugs or genetic tests. Here’s your action plan:- Check your antibiotics. If it’s ciprofloxacin, levofloxacin, or doxycycline - assume you need to space it out.
- Read the label. Every fluoroquinolone and tetracycline label now says when to avoid antacids. Don’t ignore it.
- Use a pill organizer. Separate your antibiotics and antacids into different slots. Label them clearly.
- Ask your pharmacist. They’re trained to catch these interactions. Most will offer a free 5-minute consultation.
- Switch if you can. If you take antacids daily, talk to your doctor about switching to omeprazole or famotidine.
And if you’re ever unsure - wait. Take your antibiotic on an empty stomach. Wait 2 hours. Then take your antacid. It’s that simple. And it could mean the difference between getting better - and having to start all over again.
What If You Accidentally Took Them Together?
Don’t panic. One mistake won’t ruin your whole course. But don’t just keep going the same way.If you took them together once, skip the next dose of antacid. Wait at least 4 hours before taking your next antibiotic. Resume your schedule properly. If you’re on a short course (like 5-7 days), just stick to the rules for the rest. If you’re on a longer course, or if your symptoms aren’t improving, call your doctor. You might need a different antibiotic or a longer treatment.
Remember: antibiotics aren’t like vitamins. They need to reach a certain level in your blood to work. If you keep mixing them with antacids, you’re not just reducing their effect - you’re helping bacteria survive and become stronger.
Can I take Tums with amoxicillin?
You can, but it’s not ideal. Amoxicillin loses about 15-20% of its absorption when taken with antacids. That’s usually not enough to cause treatment failure in healthy people. But if you’re elderly, diabetic, or have a weakened immune system, even a small drop matters. Best practice: wait 1-2 hours between doses.
Does omeprazole interact with antibiotics like antacids do?
No. Omeprazole and other proton pump inhibitors reduce stomach acid but don’t contain aluminum, magnesium, or calcium. They don’t bind to antibiotics the way antacids do. That’s why doctors often switch patients from Tums to omeprazole when both are needed. It’s a safer combo.
What if I forget and take my antibiotic with food and antacid?
If it’s just one time, don’t double up on your next dose. Just wait until your next scheduled time and take the antibiotic on an empty stomach, with water, and avoid antacids for the next 4 hours. Consistency matters more than perfection.
Can antacids affect all antibiotics?
No. Only antibiotics that bind to minerals - mainly fluoroquinolones and tetracyclines. Penicillins (like amoxicillin), macrolides (like azithromycin), and metronidazole aren’t strongly affected. Always check your specific drug, but don’t assume all antibiotics behave the same.
Why does the FDA require timing instructions on antibiotic labels now?
Because studies showed that improper timing was causing real harm. A 2021 FDA analysis of 15,000 patients found that those who took ciprofloxacin with antacids had a 22% higher chance of treatment failure - leading to repeat visits, stronger antibiotics, and even hospital stays. The FDA mandated clearer labels to prevent preventable failures.

Fabian Riewe
December 31, 2025 AT 09:48Wow, this is one of those posts that makes you feel like a genius for finally getting it. I used to take Tums with my doxycycline because I thought ‘heartburn relief’ and ‘antibiotic’ were just two parts of the same morning ritual. Now I’ve got a little chart taped to my fridge. Life changed.
David Chase
January 2, 2026 AT 05:01OMG I CAN’T BELIEVE PEOPLE STILL DO THIS??!! 😱 Like, are we living in 2005?!! Antacids + cipro = bacterial rave party 🎉💀. Stop killing your meds with antacid snacks. I swear, if I had a dollar for every time someone told me they ‘took it with food’ and then got sicker… I’d buy a yacht. 🚢💸
Emma Duquemin
January 2, 2026 AT 17:36This is the kind of post that should be plastered on every pharmacy counter, mailed to every senior center, and read aloud at family dinners. I had a friend who kept getting recurrent UTIs for TWO YEARS because she took her cipro right after her Tums like it was a smoothie. When she finally figured out the 4-hour gap? She cried. Not from sadness-from relief. That’s the power of simple science, folks. 🙌
And yes, switching to omeprazole? Absolute game-changer. My mom’s been on it for six months now. No more ‘antibiotic roulette.’ She’s thriving. We need more of this clarity, not more jargon.
Also, the genetic testing bit? Mind. Blown. Imagine your body saying, ‘Hey, I empty my stomach slow, so you need 6 hours.’ That’s not sci-fi-that’s the future. And I’m here for it.
Kevin Lopez
January 3, 2026 AT 23:12Chelation kinetics of divalent cations with fluoroquinolones are well-documented in JAC 2018. The AUC reduction is statistically significant (p<0.001). Don’t conflate pharmacokinetics with anecdotal outcomes. Timing protocols are evidence-based, not folklore.
Duncan Careless
January 5, 2026 AT 21:16Good post. Really good. I’m from the UK and we don’t always get this explained well here either. I’ve seen elderly patients just give up because they ‘can’t remember’ when to take what. A printed timetable with colour coding? Brilliant idea. Wish my GP had suggested it. I’ll be sharing this with my mum.
Samar Khan
January 7, 2026 AT 04:58So basically, if you’re not rich enough to afford omeprazole, you’re just supposed to suffer through bad antibiotics? 😏
Russell Thomas
January 7, 2026 AT 21:57Ohhh so THAT’S why my last antibiotic didn’t work? I thought I was just ‘bad at healing.’ Guess I’m not sick-I’m just dumb. 🤦♂️
And now I gotta wait 4 HOURS after my lunch burrito to take my pill? Who has that kind of time? I’m a busy adult, not a lab rat.
Joe Kwon
January 8, 2026 AT 17:03This is such a critical piece of info that’s buried in fine print. I’m a pharmacist’s assistant and I see this daily. The real tragedy? People think ‘antacid’ means ‘harmless.’ It’s not. It’s a silent saboteur. The FDA’s new labeling push? Long overdue. And the Cipro XR-24? That’s hope in a capsule. 🙏
Also, props to the Mayo Clinic study on visual charts. Sometimes, the simplest solutions are the most powerful. No app needed. Just paper, pen, and a little discipline.
Nicole K.
January 10, 2026 AT 03:46People are so careless with their health. You wouldn’t mix bleach and ammonia, but you’ll mix antibiotics and Tums like it’s nothing? It’s disgusting.
Tamar Dunlop
January 11, 2026 AT 08:25As someone who grew up in a household where ‘if it helps your stomach, take it with everything,’ this post felt like a revelation wrapped in a love letter to science. I remember my grandmother, who took Tums with every meal and every pill, collapsing from a resistant infection at 78. We never knew why. Now I know. And I’ve started carrying a tiny card in my wallet with the timing chart. I’m not just healing myself-I’m honoring her memory by getting it right.
Thank you for writing this with such care. Not everyone gets to be the person who saves someone’s life with a simple fact. You did.
Greg Quinn
January 11, 2026 AT 22:39It’s fascinating how a chemical interaction-something invisible, silent, and utterly mechanical-can derail an entire treatment plan. We treat medicine like magic, but it’s physics. And physics doesn’t care if you’re busy, tired, or confused. It just… happens. The real question isn’t why people mix them-it’s why our system lets them. Why isn’t this on every prescription bottle? Why isn’t it a mandatory pharmacy script? Maybe we don’t need better drugs. We need better systems.
Fabian Riewe
January 12, 2026 AT 16:54Actually, I just checked my amoxicillin bottle-no warning about antacids. So I’m guessing it’s fine? Or should I still wait? 😅