Antibiotic Stewardship at Home: Why Finishing Your Course and Proper Disposal Matters
 Feb, 10 2026
Feb, 10 2026
When you start an antibiotic, you might feel better after a few days. That’s great. But stopping there? That’s where the real danger begins. Antibiotics don’t work like painkillers. You can’t just take them until the ache goes away. If you quit early, even if you feel fine, you’re leaving behind the toughest bacteria-the ones that survive and come back stronger. And when they do, they can cause infections that no drug can touch. This isn’t science fiction. It’s happening right now, in homes across the country.
Why Finishing the Full Course Isn’t Optional
Doctors prescribe antibiotics for a reason: to kill every last harmful bacterium. But not all bacteria die at the same time. The ones that feel sick and weak? They go down fast. The strong ones? They hang on. If you stop taking the medicine before the full course is done, those survivors multiply. They pass on their resistance to future generations of bacteria. That’s how superbugs are born.
The CDC says stopping early can raise your risk of drug-resistant infection by 23% to 37%. That’s not a small number. That’s the difference between a simple infection you can treat and one that lands you back in the hospital. And it’s not just about you. Resistant bacteria don’t stay in one home. They spread through kitchens, bathrooms, and shared spaces. Your neighbor’s child could catch it. Your elderly parent could get it. It’s a chain reaction.
For seniors-34% of all home antibiotic users, according to AARP-the problem is worse. Many are on five, six, or seven medications. Remembering which pill to take at 2 a.m. isn’t easy. One caregiver on Reddit shared: “My mom takes 7 meds. I can’t keep track of which antibiotic goes when. I miss doses. I feel guilty.” That’s why simple tools matter. A pill organizer with alarms. A smartphone app like Medisafe, which 14,200 users rate 4.7 out of 5. These aren’t luxuries. They’re lifesavers.
What Happens When You Don’t Complete the Course
Dr. Lindsay M. Pettigrew from Yale School of Medicine says it plainly: “Non-completion rates of 38% among seniors lead to 22% higher readmission rates.” That means nearly 1 in 4 seniors who stop their antibiotics early end up back in the hospital. Why? Because the infection didn’t fully clear. It came back, harder. And now, the same antibiotic won’t work.
Studies show incomplete courses increase treatment failure by 18.7%. That’s not a guess. That’s from 14 randomized trials. And it’s not just about relapse. It’s about creating bacteria that laugh at penicillin, ignore amoxicillin, and shrug off azithromycin. These bugs don’t care if you’re 72 or 17. They only care if they can survive.
And here’s the scary part: you don’t need to be sick to spread resistance. If you keep leftover pills, you’re storing a time bomb. Someone else might take them-your grandchild, a friend with a sore throat. Or worse, you might take them again next time you feel “a little off.” That’s not self-care. That’s playing Russian roulette with antibiotics.
Proper Disposal: It’s Not Trash or Sink
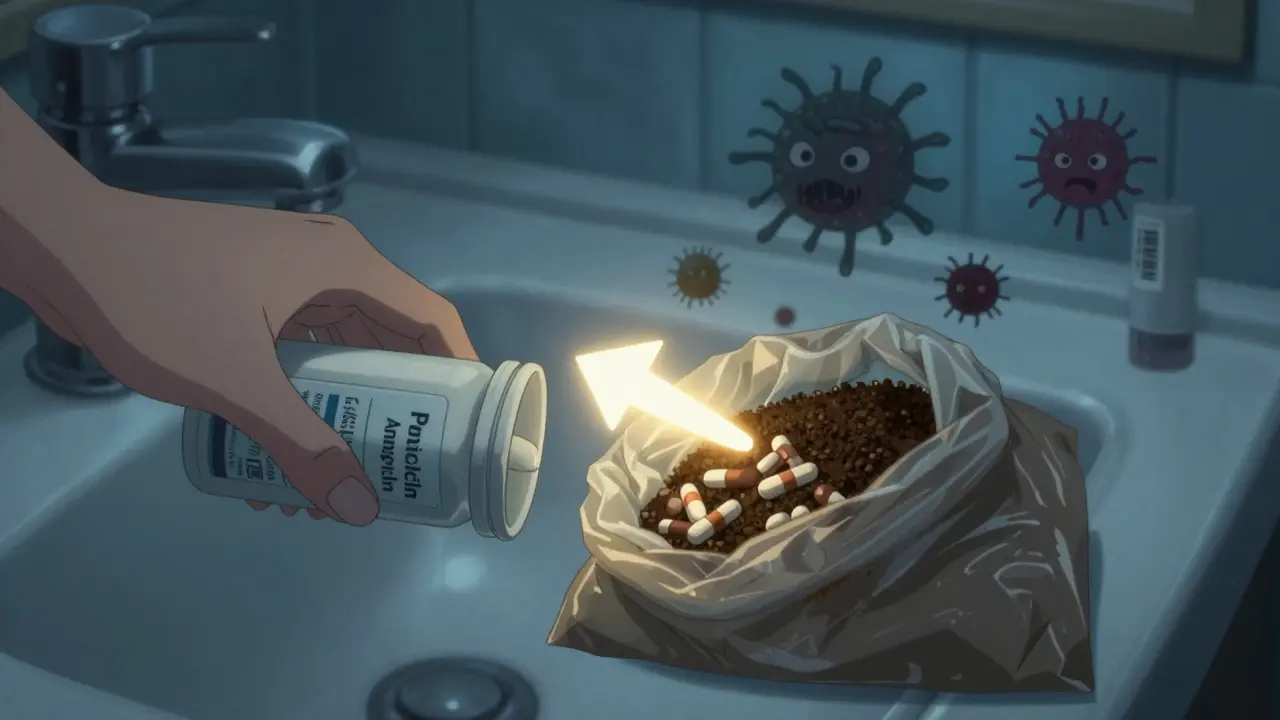
What do you do with the leftover pills? Throw them in the trash? Flush them down the toilet? Don’t. Both are dangerous.
Flushing antibiotics lets them enter water systems. A 2022 study found antibiotic residues in 63% of U.S. waterways near cities. Those chemicals don’t disappear. They mix with fish, frogs, algae-and even our drinking water. That’s how resistance spreads in nature, not just in hospitals.
Throwing them in the trash? That’s not safe either. Curbside pickup doesn’t mean safe disposal. Someone could dig through your bin. A child might find them. Pets might eat them. The FDA recommends a better way: mix unused pills with something unappealing-used coffee grounds, cat litter, dirt. Put the mixture in a sealed plastic bag. Then toss it in the trash. No labels. No pills visible. No temptation.
And here’s a hard truth: only 29% of home users know this method. Sixty-one percent keep leftovers for “next time.” That’s not smart. It’s risky. Antibiotics don’t expire like milk. But their effectiveness fades. And the dose might not match your new infection. What worked for a sinus infection might do nothing for a urinary tract infection. Worse, it could make the next one untreatable.
How to Make It Stick at Home
Stewardship at home isn’t about fancy tools. It’s about habits. Here’s how to build them:
- Use a pill organizer with alarms. Look for ones that beep at dosing times. Some even send alerts to your phone. Hero, a popular device, costs $299 with a $25/month fee-but many insurance plans cover it for seniors.
- Set calendar reminders. Even if you don’t use an app, set two alarms: one for morning, one for night. Label them clearly: “AM Antibiotic.”
- Track doses. Mark off each pill you take. A simple calendar on the fridge works. If you miss a dose, don’t double up. Call your doctor.
- Ask for a 48-hour check-in. After two days on antibiotics, ask your doctor: “Should we keep going?” This is called an “antibiotic timeout.” Hospitals do it. You should too. Studies show it cuts unnecessary use by nearly 20%.
- Dispose immediately after finishing. Don’t wait. Don’t store. Mix, bag, trash-right away.
And if you’re a caregiver? Educate yourself. The National Alliance for Caregiving says only 31% of family caregivers get proper training. That’s unacceptable. Ask your pharmacist for a 10-minute briefing. Watch the CDC’s free videos. Download their Home Care Stewardship Toolkit (coming Q1 2025). You’re not just helping someone. You’re protecting a community.
What’s Changing-and What’s Coming
Change is happening, slowly. The CDC’s 2024 update to its Core Elements now includes home settings. AALLCare released new guidelines in October 2024, specifically for seniors. They say: “No doses missed. Full course completed. No leftovers kept.”
The FDA’s 2024 National Action Plan sets a goal: reduce inappropriate antibiotic use in homes by 15% by 2027. That’s not a suggestion. It’s a target. And it’s backed by real data. Johns Hopkins piloted telehealth check-ins for home patients. Result? 28% fewer unnecessary antibiotic days. That’s proof that support works.
But here’s the gap: 78% of nursing homes have structured antibiotic reviews. Only 12% of home care agencies do. That’s not a mistake. That’s a system failure. And until home care is treated like a frontline health setting, not an afterthought, this problem won’t fix itself.
It’s Not Just About Pills. It’s About Survival
Antibiotics saved millions of lives in the 20th century. But we’re throwing that away. Every time we stop early. Every time we flush a pill. Every time we share a leftover dose. We’re giving bacteria the tools to win.
There’s no magic pill for resistance. No new drug coming soon. The only defense we have right now is simple: use antibiotics exactly as prescribed. Finish them. Dispose of them safely. And teach others to do the same.
Because the next superbug won’t come from a hospital. It’ll come from your kitchen cabinet. And it might be the one that kills someone you love.
What happens if I stop my antibiotic early even if I feel better?
Stopping early leaves behind the strongest bacteria. These survivors multiply and pass on resistance, making future infections harder-or impossible-to treat. The CDC says this increases your risk of drug-resistant infection by 23% to 37%. You might feel fine, but the infection isn’t fully gone.
Can I give my leftover antibiotics to a friend or family member?
Never. Antibiotics are prescribed for a specific infection, at a specific dose, for a specific person. What works for you might not work for them-or could make their condition worse. Sharing antibiotics contributes to misuse and resistance. It’s not just unsafe. It’s dangerous.
Is it safe to flush antibiotics down the toilet?
No. Flushing antibiotics pollutes water systems. A 2022 study found antibiotic residues in 63% of U.S. waterways near populated areas. These chemicals harm aquatic life and can end up in drinking water. The FDA recommends mixing pills with coffee grounds or cat litter, sealing them in a bag, and throwing them in the trash.
How can I remember to take my antibiotics on time?
Use a pill organizer with alarms, smartphone apps like Medisafe (rated 4.7/5), or set calendar reminders. For seniors on multiple meds, devices like Hero (costing $299 with $25/month subscription) can automatically dispense pills and notify caregivers. These tools reduce missed doses by up to 70%.
Should I still take antibiotics if I have side effects?
Mild side effects like nausea or diarrhea are common. Don’t stop unless you have a severe reaction-like rash, swelling, trouble breathing, or persistent vomiting. Call your doctor. They may adjust the dose or switch antibiotics. Never stop without medical advice. Stopping early increases resistance risk more than mild side effects do.
Are there free resources to help with antibiotic stewardship at home?
Yes. The CDC offers free downloadable toolkits, posters, and guides for home caregivers. The ‘Be Antibiotics Aware’ campaign also provides videos and printable checklists. AALLCare’s 2024 guidelines for seniors are available online. Ask your pharmacist-they often have printed materials too.
Next Steps: What You Can Do Today
- Check your medicine cabinet. Are there old antibiotics? If yes, dispose of them now using the coffee grounds method.
- Set up reminders for your next antibiotic course-even if you haven’t been prescribed one yet. Practice the habit.
- Ask your doctor or pharmacist: “Can I get a copy of the CDC’s Home Care Stewardship Toolkit?”
- Teach one person-your parent, sibling, neighbor-how to complete a course and dispose of pills safely.
Antibiotic resistance doesn’t wait. It doesn’t care if you’re busy, tired, or confused. But you can fight back. One pill. One reminder. One properly disposed bottle. It starts at home.
