Antibiotics in Children: When They’re Needed, Side Effects, and How to Avoid Allergies
 Jan, 28 2026
Jan, 28 2026
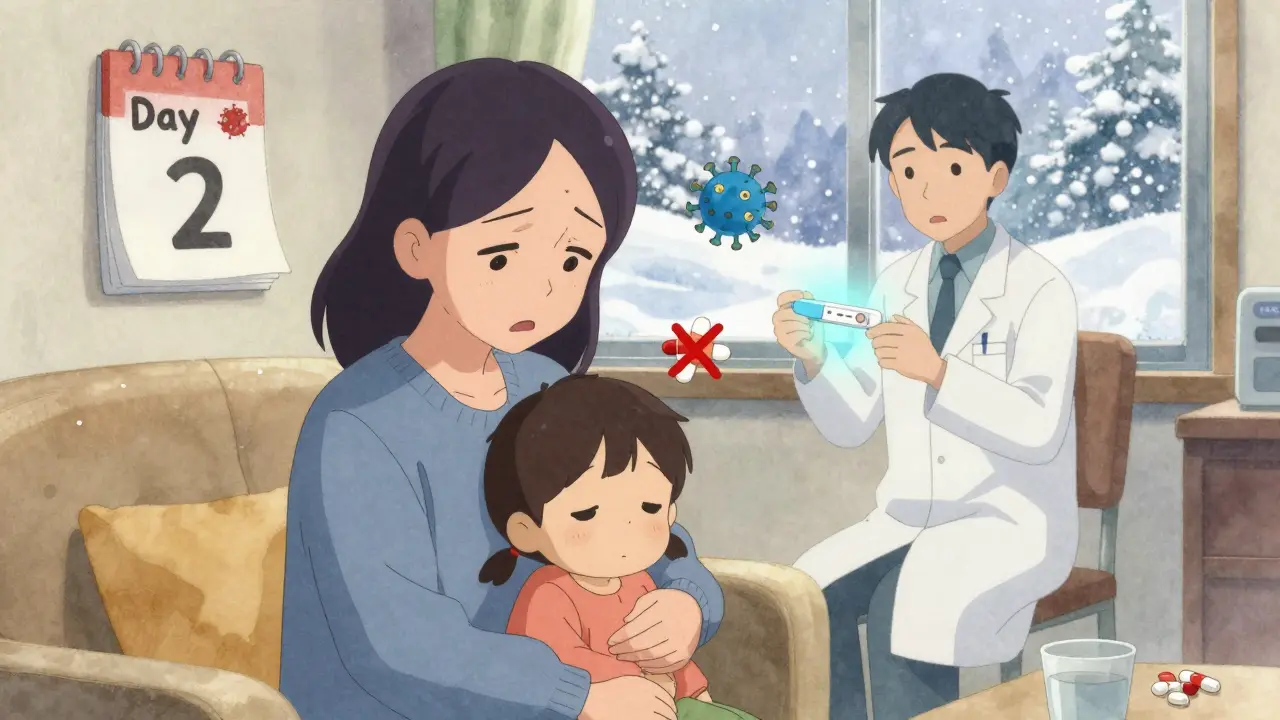
Every parent has been there: your child has a fever, a runny nose, a sore throat, and you’re wondering-should we give them antibiotics? It’s a question that comes up again and again, especially when your child is miserable and you just want to make them feel better. But here’s the hard truth: antibiotics won’t help most childhood illnesses. And giving them when they’re not needed can do more harm than good.
Antibiotics Only Work on Bacteria-Not Viruses
Antibiotics are powerful drugs designed to kill or stop the growth of bacteria. They don’t work on viruses. That’s why they won’t help with the common cold, flu, most coughs, or stomach bugs. In fact, 99% of cases with vomiting and diarrhea in kids are caused by viruses. So are 90% of pneumonia cases and nearly all cases of bronchiolitis. Even if your child has thick, yellow, or green mucus, that doesn’t mean they need antibiotics. Color changes in nasal discharge are normal during viral colds and can last for days.
Only about 20% of sore throats in children are bacterial-specifically strep throat. And only 10% of pneumonia cases are bacterial. That means in 8 out of 10 cases where parents think their child needs antibiotics, they don’t. Yet, doctors still prescribe them unnecessarily in about 30% of pediatric outpatient visits. That’s not just wasteful-it’s dangerous.
When Do Kids Actually Need Antibiotics?
Antibiotics should only be used when there’s clear evidence of a bacterial infection. Here’s what doctors look for:
- Strep throat: A positive rapid test or throat culture is required. You can’t tell by sight alone-symptoms like fever and sore throat alone are wrong more than half the time.
- Ear infections (acute otitis media): Antibiotics are recommended only if the child has moderate to severe ear pain, a bulging eardrum, or fluid draining from the ear. For children over 6 months with mild symptoms, doctors often recommend watching for 48-72 hours first.
- Sinus infections: Only if symptoms last more than 10 days without improvement, or if they get worse after initially improving. Most sinus issues are viral.
- Pneumonia: If the child is very ill, has high fever, rapid breathing, and a doctor hears crackles in the lungs, antibiotics may be needed. But most cases are viral and will clear on their own.
- Whooping cough (pertussis): Yes, antibiotics are used here-but only to stop the spread to others. They don’t always shorten the cough, which can last weeks.
For many mild ear infections in kids over 2 years old, the American Academy of Pediatrics now recommends watchful waiting. If the child isn’t in severe pain and doesn’t have a high fever, waiting 48 hours often means no antibiotics are needed-and the body clears the infection on its own.
Common Side Effects of Antibiotics in Kids
Even when antibiotics are used correctly, side effects are common. About 1 in 10 children will have a reaction. Most are mild, but they can be unsettling.
- Diarrhea: This is the most frequent side effect, affecting 5-25% of kids. It happens because antibiotics kill good bacteria in the gut along with bad ones. In some cases, this leads to Clostridium difficile infection, which causes severe diarrhea and can be dangerous.
- Nausea and vomiting: These happen in 3-18% of children, especially with stronger antibiotics.
- Rashes: About 2-10% of kids get a rash. But here’s the big mistake most parents make: 80-90% of these rashes are not allergies. They’re just side effects-often flat, pink spots that don’t itch much and go away on their own.
- Yeast infections: Especially in girls, antibiotics can cause diaper rash or vaginal yeast infections. These are treatable with antifungal creams.
These side effects usually go away after the course ends. But if diarrhea is watery, bloody, or lasts more than a few days, call your doctor. Same goes for vomiting that won’t stop or signs of dehydration.

True Allergies vs. Misdiagnosed Reactions
Many parents think their child is allergic to penicillin because they got a rash once. But here’s what you need to know: fewer than 1 in 10 children labeled “allergic” to penicillin actually are.
True allergic reactions are serious. They include:
- Hives (raised, itchy red welts)
- Swelling of the lips, tongue, or face
- Wheezing or trouble breathing
- Anaphylaxis (a life-threatening reaction with low blood pressure, vomiting, and loss of consciousness)
If your child has any of these during or right after taking an antibiotic, get emergency help immediately. But if it’s just a mild, non-itchy rash that appears a few days later? That’s likely not an allergy. Many doctors now recommend allergy testing for kids with a history of “penicillin allergy,” because 95% of them can safely take penicillin-based antibiotics later.
And don’t assume your child is allergic just because you or a sibling are. Family history doesn’t predict it. Each child’s immune system reacts on its own.
Why Antibiotic Resistance Is a Silent Crisis
Every time you give an antibiotic when it’s not needed, you’re helping bacteria become stronger. This is called antibiotic resistance. And it’s getting worse.
Today, 47% of the bacteria that cause ear infections and pneumonia in kids no longer respond to penicillin. That’s up from 35% just 10 years ago. MRSA, a dangerous type of staph infection once found mostly in hospitals, is now common in schools and playgrounds. Since 2010, community-based MRSA infections in children have jumped by 150%.
These resistant infections are harder to treat. They require stronger, more expensive drugs. They lead to longer hospital stays. And in the worst cases, they can be deadly. In the U.S. alone, antibiotic-resistant infections cause over 35,000 deaths every year.
And it’s not just the child who’s at risk. When one child gets resistant bacteria, it can spread to siblings, grandparents, and classmates. Antibiotic resistance doesn’t care about age or health-it just spreads.
How to Give Antibiotics the Right Way
If your doctor says your child needs antibiotics, here’s how to do it right:
- Finish the full course. Even if your child feels better after two days, keep giving the medicine. Stopping early lets the toughest bacteria survive and multiply.
- Give it on schedule. For amoxicillin, doses should be spaced 12 hours apart. For azithromycin, take it daily for 3-5 days, no matter what.
- Don’t share or save leftovers. Never give your child someone else’s antibiotics. And never keep unused ones for next time. They won’t work for a different infection and can be dangerous.
- Watch for vomiting. If your child throws up within 30 minutes of taking the dose, give the full dose again. If it’s between 30 and 60 minutes, give half the dose. After an hour, don’t repeat it.
And yes-many antibiotics taste awful. Liquid amoxicillin? Bitter. Azithromycin? Like chalk. Here’s what works: mix it with a small spoonful of chocolate syrup, apple sauce, or yogurt. Don’t mix it into a whole bottle of juice-it might dilute the dose. Some pharmacies offer flavoring services to make it more palatable.

What to Do If Your Child Doesn’t Improve
Antibiotics should start working in 48-72 hours. If your child’s fever is still high, they’re still in pain, or they’re getting worse after two days, call the doctor. Don’t just keep giving the same medicine. It might not be the right one, or the infection might be viral after all.
Also, don’t pressure your doctor for antibiotics. Many parents feel guilty if they don’t get a prescription, but that’s the wrong mindset. The best doctors are the ones who say, “Let’s wait and see,” or “This is viral, and we’ll help you manage it.”
What’s New in Pediatric Antibiotic Care
There’s good news on the horizon. In January 2023, the FDA approved a new rapid test that can tell if an infection is bacterial or viral in just 6 hours-not 2-3 days. This means doctors can avoid broad-spectrum antibiotics and use targeted ones only when needed.
Another tool gaining traction is CRP testing-a simple blood test that measures inflammation. In clinics using it, antibiotic use dropped by 85% without increasing complications. And a 2022 study showed that using procalcitonin (another blood marker) to guide treatment cut unnecessary prescriptions by 62%.
The goal? By 2025, the CDC wants to reduce inappropriate antibiotic use in children by half. That’s not just a number-it’s a lifeline for future generations.
What Parents Can Do Today
You don’t need to be a doctor to help fight antibiotic resistance. Here’s how:
- Ask: “Is this definitely bacterial?”
- Ask: “What happens if we wait a couple of days?”
- Ask: “Is there a test to confirm this?”
- Don’t pressure your doctor for a prescription.
- Don’t use leftover antibiotics from a previous illness.
- Teach your child to wash hands often-prevention beats treatment every time.
Most childhood illnesses get better with rest, fluids, and time. Antibiotics are powerful tools-but they’re not magic. The most important thing you can give your sick child right now isn’t a pill. It’s patience, comfort, and trust in the body’s ability to heal.
Can antibiotics treat a cold or flu in children?
No. Colds and flu are caused by viruses, and antibiotics only work on bacteria. Giving antibiotics for a viral illness won’t help your child feel better faster and can cause harmful side effects or lead to antibiotic resistance.
My child had a rash after taking amoxicillin-does that mean they’re allergic?
Not necessarily. Most rashes that appear after taking antibiotics are side effects, not true allergies. True allergic reactions include hives, swelling of the face or lips, wheezing, or trouble breathing. If your child only had a flat, pink rash without other symptoms, it’s likely not an allergy. Talk to your doctor about allergy testing before assuming they’re allergic for life.
What should I do if my child vomits after taking an antibiotic?
If vomiting happens within 30 minutes of taking the dose, give the full dose again. If it’s between 30 and 60 minutes after, give half the dose. If it’s more than an hour later, don’t repeat it-wait until the next scheduled dose. Always check with your doctor or pharmacist if you’re unsure.
How long should I keep giving antibiotics if my child feels better?
Always finish the full course, even if your child seems fine after a day or two. Stopping early lets the strongest bacteria survive and multiply, which can lead to a worse infection later and contributes to antibiotic resistance. For example, amoxicillin for ear infections is usually given for 10 days-even if symptoms improve by day 3.
Are there alternatives to antibiotics for ear infections in kids?
Yes. For children over 6 months with mild ear infections, doctors often recommend watchful waiting for 48-72 hours. Pain relief with ibuprofen or acetaminophen, warm compresses, and rest can help while the body fights off the infection. Antibiotics are only started if symptoms worsen or don’t improve after a couple of days.
Why do some doctors still prescribe antibiotics unnecessarily?
Some doctors prescribe antibiotics because parents expect them, or because it’s faster than explaining why they’re not needed. Others may be unsure about the diagnosis. But guidelines are clear: antibiotics should only be used when there’s strong evidence of a bacterial infection. More doctors are now using rapid tests and waiting strategies to avoid unnecessary prescriptions.
