Anticoagulants in Seniors: Fall Risk vs. Stroke Prevention
 Jan, 14 2026
Jan, 14 2026
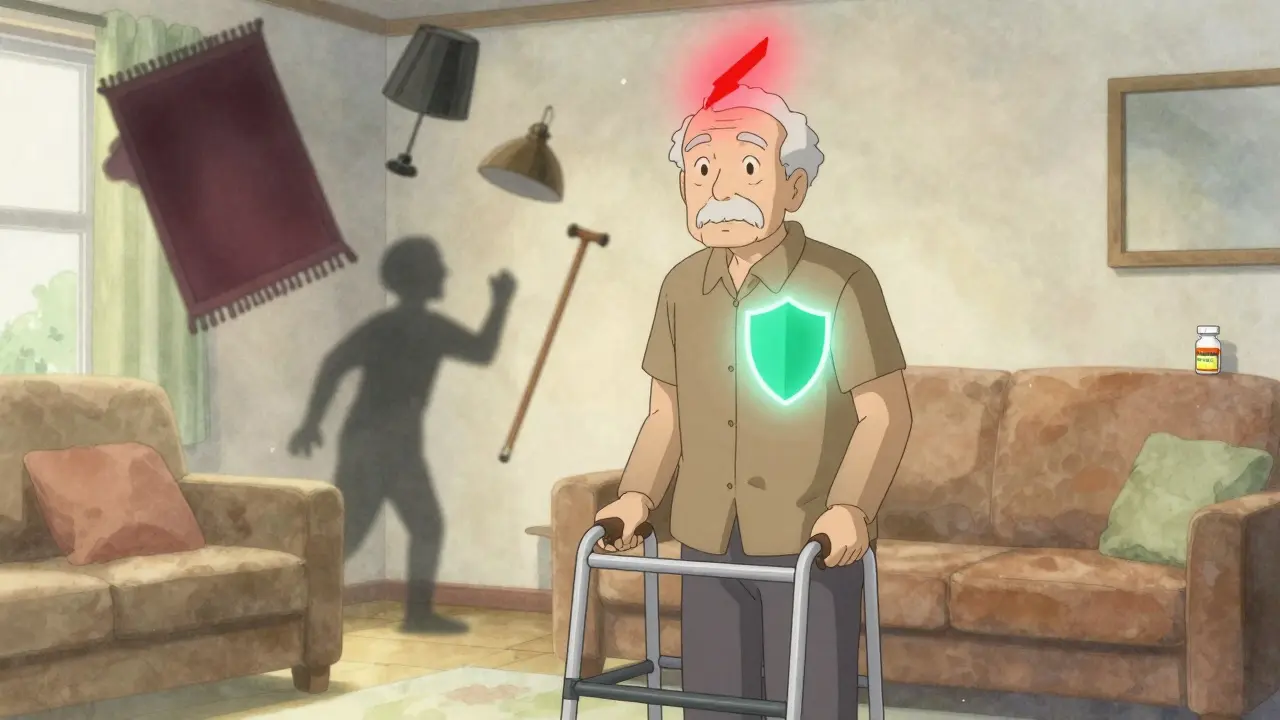
Every year, thousands of older adults in the U.S. and around the world face a quiet, life-altering decision: take a blood thinner to prevent a stroke, or avoid it because they’re afraid of falling. It’s not a hypothetical question. For many seniors with atrial fibrillation - an irregular heartbeat that affects nearly 1 in 10 people over 65 - this choice comes down to two very real dangers: a stroke that could end their independence, or a fall that could lead to a fatal bleed.
Why Anticoagulants Are Often Necessary
Atrial fibrillation, or AFib, is more than just an irregular heartbeat. It’s a silent threat. When the heart’s upper chambers quiver instead of pumping properly, blood can pool and form clots. If one of those clots breaks loose, it can travel to the brain and cause a stroke. The risk doesn’t creep up slowly - it spikes with age. At 70, your chance of a stroke from AFib is about 10% per year. By 85, it jumps to nearly 24% per year. That’s more than 1 in 5 people. Anticoagulants - blood thinners - cut that risk in half or more. Warfarin, used since the 1950s, reduces stroke risk by about 64%. Newer drugs like apixaban (Eliquis), rivaroxaban (Xarelto), and dabigatran (Pradaxa) do just as well, sometimes better. In fact, the ARISTOTLE trial showed apixaban reduced stroke and systemic embolism by 21% compared to warfarin. And here’s the kicker: they’re safer. Apixaban cuts major bleeding risk by 31% in people over 75. Rivaroxaban lowers the chance of bleeding in the brain by 34%.The Fall Fear Is Real - But Often Misplaced
It’s understandable to worry. Seniors fall. Sometimes often. About 1 in 4 Americans over 65 fall each year. And when someone on a blood thinner falls, the consequences can be severe. A head injury can turn into a brain bleed. A hip fracture can lead to surgery, hospitalization, and a downward spiral. But here’s what the data says: the fear of falling shouldn’t stop treatment. The BAFTA trial studied 413 people over 75 with AFib. Half got warfarin. Half got aspirin. The warfarin group had 52% fewer strokes. And the rate of major bleeding? No significant difference. Another study of 819 patients aged 85-89 found they got the most benefit from anticoagulants - even though they had the highest bleeding risk. The American College of Cardiology, the American Heart Association, and the Heart Rhythm Society all agree: age and fall history alone are not reasons to avoid anticoagulants. In fact, the 2023 American College of Chest Physicians guidelines say: "The net clinical benefit remains positive even in patients with multiple falls."What Doctors Get Wrong - And Why
Despite the evidence, underuse is common. Only about 48% of people over 85 with AFib get anticoagulants, compared to 72% of those in their 60s. Why? A 2021 survey found 68% of primary care doctors would withhold blood thinners from an 85-year-old who’d fallen twice - even if their stroke risk score (CHA2DS2-VASc) was high. Clinicians aren’t being careless. They’re overwhelmed. They see the headlines: "Elderly Man Dies After Fall on Blood Thinner." They hear family members say, "We can’t risk it." They worry about lawsuits. They don’t have time to explain the numbers. But the real danger isn’t the fall. It’s the untreated AFib. Studies show elderly patients are far more likely to suffer a stroke than to die from a fall-related bleed. One analysis found that for every 100 octogenarians treated with apixaban for a year, 24 strokes are prevented - and only 3 major bleeds occur. That’s a net gain of 21 lives saved or disability avoided.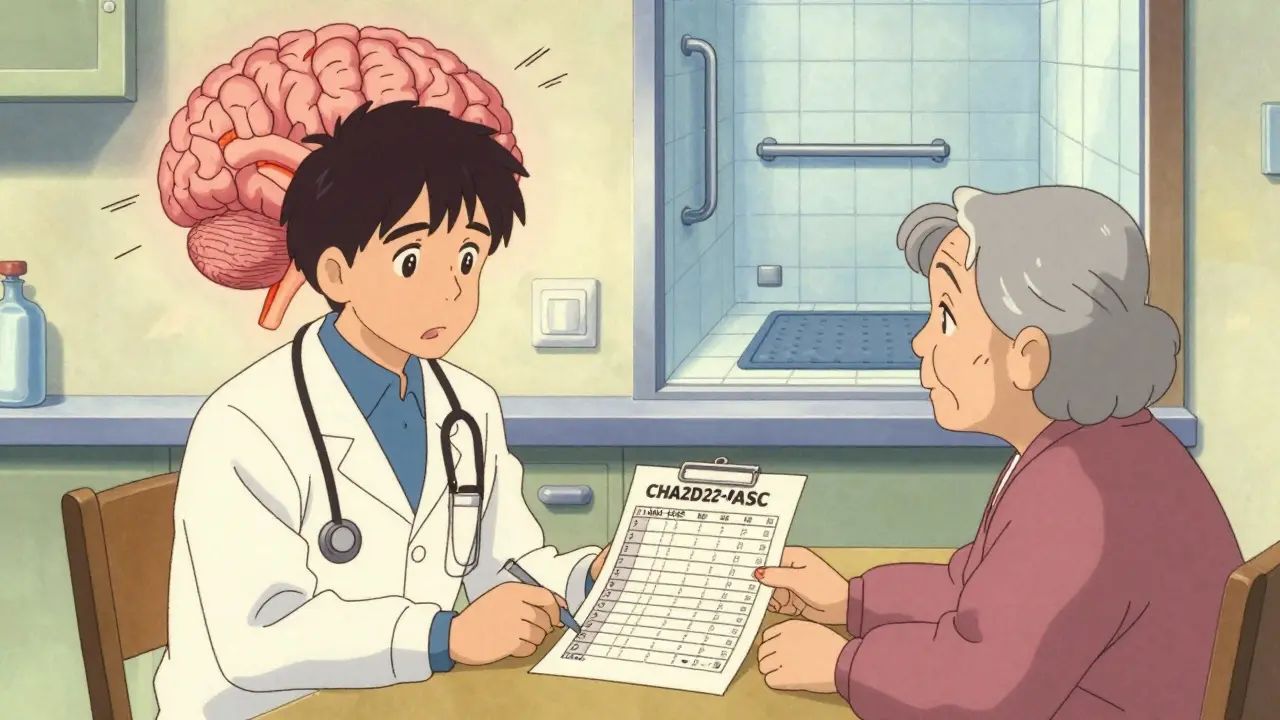
How to Make Anticoagulants Safer - Not Avoid Them
You don’t have to choose between stroke prevention and safety. You can have both - if you take smart steps. First, pick the right drug. DOACs like apixaban and edoxaban are easier to manage than warfarin. No weekly blood tests. Fewer food interactions. Lower risk of brain bleeds. But they’re cleared by the kidneys - so if someone has poor kidney function, dosing matters. Check creatinine clearance every 6-12 months. Second, reduce fall risk. It’s not about stopping the blood thinner - it’s about stopping the fall. A proven plan includes:- Removing tripping hazards: loose rugs, cluttered floors, poor lighting
- Installing grab bars in bathrooms and handrails on stairs
- Using non-slip mats in showers
- Reviewing all medications - especially sleep aids, painkillers, and antidepressants that cause dizziness
- Starting the Otago Exercise Program - shown to reduce falls by 35% in seniors
What Happens When You Stop
Too often, families and even doctors stop anticoagulants after a fall - thinking they’re protecting the patient. But stopping is dangerous. Within weeks, the risk of stroke returns to baseline. A 2022 study found that elderly patients who stopped anticoagulants after a fall had a 4x higher risk of stroke in the next year than those who stayed on therapy. One Reddit thread from caregivers described a grandmother with AFib and two falls. Her doctor said, "We’ll hold off on the blood thinner." She had a stroke six months later. Paralyzed on one side. Couldn’t speak. She didn’t die from the fall. She died from the stroke they tried to prevent by stopping the medicine.Reversal Agents - A Game Changer
In the past, if someone on warfarin had a major bleed, doctors could give vitamin K or fresh frozen plasma. But it took hours. For DOACs, there was no antidote - until recently. Now, we have specific reversal agents:- Idarucizumab (Praxbind) reverses dabigatran within minutes
- Andexanet alfa (Andexxa) reverses apixaban, rivaroxaban, and edoxaban
What You Can Do Right Now
If you or a loved one has AFib and is being told to avoid anticoagulants because of fall risk:- Ask for the CHA2DS2-VASc score. If it’s 2 or higher, anticoagulation is recommended.
- Ask if apixaban or edoxaban is an option - they’re safer in older adults.
- Request a fall risk assessment - not to stop meds, but to prevent falls.
- Ask about kidney function tests - DOACs need dose adjustments if kidneys are weak.
- Find out if the hospital has reversal agents on hand.
Anticoagulants aren’t the problem. The lack of action to prevent falls is.
Should seniors stop anticoagulants after a fall?
No. Stopping anticoagulants after a fall increases stroke risk by up to four times. The risk of stroke in someone with atrial fibrillation is far greater than the risk of a fatal bleed from a fall - especially when fall prevention measures are in place. Guidelines from the American Heart Association and others strongly advise against discontinuing therapy solely due to fall history.
Are newer blood thinners safer for seniors than warfarin?
Yes. Direct oral anticoagulants (DOACs) like apixaban, rivaroxaban, and edoxaban are generally safer for seniors than warfarin. They don’t require frequent blood tests, have fewer food and drug interactions, and cause fewer brain bleeds. Apixaban, in particular, reduces major bleeding by 31% in patients over 75 compared to warfarin. They’re now the first-line choice for most elderly patients with atrial fibrillation.
Can kidney problems make anticoagulants unsafe for older adults?
Some DOACs are cleared by the kidneys, so reduced kidney function can raise drug levels and increase bleeding risk. Dabigatran is mostly cleared by the kidneys (80%), while apixaban is less so (27%). Doctors check kidney function (creatinine clearance) every 6-12 months and adjust doses accordingly. For severe kidney disease, warfarin may be preferred, or a lower DOAC dose may be used. Never stop or change a dose without medical advice.
Is aspirin a good alternative to blood thinners for stroke prevention in seniors?
No. Aspirin reduces stroke risk by only about 22% in atrial fibrillation - compared to 64% with anticoagulants. The BAFTA trial showed that elderly patients on warfarin had 52% fewer strokes than those on aspirin. Aspirin is not recommended for stroke prevention in AFib by any major guideline. It’s a common mistake, but it’s dangerous.
What’s the best way to prevent falls in seniors on blood thinners?
Start with a home safety check: remove rugs, add grab bars, improve lighting. Review all medications - especially sedatives and painkillers. Start a balance program like the Otago Exercise Program, which reduces falls by 35%. Use a cane or walker if needed. Get vision checked yearly. Don’t rely on one fix - combine multiple strategies. The goal isn’t to avoid anticoagulants - it’s to keep the person safe so they can stay on them.

Andrew Freeman
January 14, 2026 AT 13:47anticoagulants my ass they just wanna sell pills and make banks richer
Sarah -Jane Vincent
January 16, 2026 AT 07:04Oh please. You think Big Pharma gives a damn about your grandma's balance? They're laughing all the way to the bank while you're reading this. DOACs cost $500/month. Warfarin is $4. The reversal agents? $10k a dose. They don't care if you live or die-they care if your insurance pays. And don't get me started on how they pushed these drugs through the FDA with barely any long-term data. Your 'net clinical benefit' is a marketing slide deck.
And the Otago Program? Cute. But who's gonna pay for the home visits? The physical therapist? The fall sensors? The 24/7 caregiver? Your 'smart steps' are just privilege in a lab coat. I've seen 80-year-olds on Medicaid fall in their own bathrooms because the VA didn't install grab bars for six years. Now tell me again why we're blaming the fall and not the system.
And yes, aspirin is trash for AFib-but so is pretending these drugs are safe. I know a woman who bled out after a tiny slip because the ER didn't have Andexxa. They gave her plasma. Took three hours. She died before they even got her to the OR. That's not 'safer.' That's roulette with a loaded gun and a smile.
Stop romanticizing anticoagulants like they're a moral victory. They're a high-stakes gamble. And the house always wins when the patient can't afford the backup plan.
Dylan Livingston
January 16, 2026 AT 11:58How delightful. Another sanctimonious pamphlet dressed up as medical wisdom. You know, I once read a peer-reviewed study that found people who take blood thinners are statistically more likely to be buried in expensive caskets because their families couldn’t afford to clean up the bloodstains from the living room floor. But no, let’s not talk about that. Let’s talk about how ‘the numbers are clear’-as if numbers don’t come from studies funded by the same companies that make the drugs.
And let’s not forget the charming detail that many of these ‘safer’ DOACs have no antidote in 70% of rural hospitals. So if your 87-year-old mother falls while taking apixaban, and the nearest hospital with Andexxa is 90 miles away? Well, congrats! You’ve just made her a tragic statistic in a TED Talk. Meanwhile, the doctor who prescribed it? Probably got a bonus.
Oh, and the Otago Exercise Program? Yes, because nothing says ‘I care about your dignity’ like a 90-year-old woman doing balance drills in a fluorescent-lit community center while her Medicare Advantage plan denies her home safety modifications. The real tragedy isn’t the stroke-it’s the system that makes you choose between dignity and death, then calls it ‘informed consent.’
And don’t even get me started on the fact that the CHA2DS2-VASc score was designed for clinical trials, not for the 84-year-old widow who lives alone with two cats, a walker, and a fear of stairs. But sure, let’s keep pretending this is medicine and not a spreadsheet with a stethoscope.
Anna Hunger
January 17, 2026 AT 21:02It is imperative to emphasize that the clinical guidelines referenced in this post are grounded in robust, evidence-based research, and their adherence significantly improves patient outcomes. The underutilization of direct oral anticoagulants (DOACs) in elderly populations with atrial fibrillation remains a critical quality-of-care gap. The risk-benefit ratio, as demonstrated by the ARISTOTLE and BAFTA trials, overwhelmingly supports anticoagulation even in the presence of recurrent falls.
It is also essential to recognize that fall prevention is not an alternative to anticoagulation-it is a necessary adjunct. A multidisciplinary approach, including occupational therapy, medication reconciliation, and environmental modification, must be systematically implemented. Failure to do so reflects a systemic failure in geriatric care, not a contraindication to therapy.
Furthermore, the availability of specific reversal agents, while not universally accessible, represents a significant advancement in patient safety. Clinicians should advocate for institutional protocols that ensure timely access to these agents, particularly in high-risk populations.
Patients and caregivers must be educated not to discontinue anticoagulants after a fall. The data are unequivocal: discontinuation increases stroke risk by up to fourfold. This is not a matter of opinion-it is a matter of clinical fact. The responsibility lies with healthcare providers to communicate this clearly, compassionately, and consistently.
Let us not confuse fear with wisdom. The goal is not to avoid risk entirely-impossible in geriatric medicine-but to mitigate it intelligently. Anticoagulation, paired with fall prevention, is not only safe-it is the standard of care.
Robert Way
January 18, 2026 AT 23:07my grandma took one of those blood thinners and she fell and died and now i dont trust doctors at all
they just wanna kill old people
Vicky Zhang
January 20, 2026 AT 20:14Oh honey. I’ve been there. My dad was 83, AFib, fell three times in six months. Doctor said, ‘We’ll hold off on the blood thinner.’ Six months later-he had a stroke. Couldn’t talk. Couldn’t move his right side. We had to feed him through a tube for the last two years. He never smiled again.
It broke my heart. Not because he died. Because he was still alive… and we could’ve prevented it.
They told us, ‘He’s too old. Too frail.’ But the truth? He was too loved. And we were too scared. We thought we were protecting him. We didn’t realize we were killing him slowly.
So if you’re reading this and your doctor says, ‘Let’s not risk it’-ask for the CHA2DS2-VASc score. Ask for apixaban. Ask for a home safety check. Ask for the Otago Program. Don’t let fear make the decision. Let love make the decision. And then fight for it.
I don’t care if you’re 75 or 95. You deserve to live. Not just exist. Live.
TooAfraid ToSay
January 20, 2026 AT 21:57you think this is about medicine? nah. this is about the government using old people as guinea pigs so they can say 'we reduced stroke rates' while ignoring the real problem: why are seniors falling so much in the first place? because they're lonely, underfed, and forced to live in apartments with no handrails because the housing market is a pyramid scheme. the blood thinners are just a bandaid on a bullet wound
says haze
January 21, 2026 AT 09:25It’s fascinating how we’ve transformed a physiological condition into a moral imperative. The entire discourse around anticoagulants in seniors has been weaponized-not by clinicians, but by a culture that conflates longevity with virtue. To take a blood thinner is to be ‘responsible.’ To refuse is to be ‘irrational.’ But what if the fear of falling isn’t irrational? What if it’s the only rational response to a society that abandons its elderly in the name of efficiency?
We celebrate the ‘net clinical benefit’ like it’s a mathematical proof, but we ignore the lived reality: a woman with a hip fracture, alone in a hospital bed, surrounded by machines, her family too afraid to visit because ‘she’s not the same anymore.’ Is that a life worth preserving? Or just a statistic with a pulse?
The reversal agents? A technological mirage. They don’t restore dignity. They don’t undo the trauma of the fall, the loss of autonomy, the shame of being ‘a burden.’ And yet, we reduce this entire existential dilemma to a dosage chart.
Perhaps the real question isn’t whether to prescribe anticoagulants-but whether we’ve lost the moral courage to say: ‘Some lives are not meant to be prolonged. And that’s okay.’