Bursitis and Tendinitis: How to Tell Them Apart and Treat Them Right
 Jan, 24 2026
Jan, 24 2026
When your shoulder aches after lifting groceries, or your knee hurts when you kneel down, it’s easy to blame it all on "arthritis" or just "getting older." But more often than not, the real culprit is something more specific: bursitis or tendinitis. These aren’t the same thing - and mixing them up can make your pain last longer, sometimes for months. Bursitis is inflammation of the bursae. These are tiny, fluid-filled sacs that act like cushions between bones and tendons or muscles. There are about 160 of them in your body, and the most common ones to get inflamed are near your shoulder, elbow, hip, and knee. Think of them as shock absorbers. When they swell up, they press on nearby nerves and cause pain - especially when you lie on the sore spot at night. Tendinitis, on the other hand, is inflammation of the tendons - the thick ropes that connect your muscles to your bones. When you move, your muscles pull on these tendons. If you do the same motion over and over - typing, swinging a racket, climbing stairs - the tendon gets irritated. The pain doesn’t just sit still; it follows the path of the tendon. A classic example is tennis elbow: pain running from your elbow down your forearm when you grip something. The big difference? Bursitis pain is often dull and deep, worse with pressure or at rest. Tendinitis pain is sharper, triggered by movement. If you raise your arm and it hurts along the side of your shoulder, it’s likely tendinitis. If it hurts when you roll onto your side in bed, it’s probably bursitis. And here’s the catch: they often happen together. In fact, about 65% of people with shoulder pain have both rotator cuff tendinitis and subacromial bursitis at the same time. That’s why so many people get misdiagnosed. If your doctor assumes it’s just tendinitis and gives you stretching exercises, but you actually have bursitis, those moves can make things worse. Doctors don’t just guess. They look for three things: pain when pressing directly on the bursa or tendon, pain when moving the joint in a specific way, and swelling you can feel or see. Ultrasound is the gold standard for diagnosis - it’s 92% accurate at spotting inflamed bursae and torn tendons. MRI is overkill for most cases unless the pain doesn’t improve after a few weeks. Treatment starts the same for both: rest, ice, and avoiding what hurts. But after that, the paths split. For bursitis, a corticosteroid injection right into the bursa often brings quick relief - about 78% of patients feel better within four weeks. Ice massage with a frozen water bottle works wonders at home. One study found 73% of people using this method reported major improvement. Just roll it slowly over the sore spot for 5-10 minutes, twice a day. For tendinitis, injections are less reliable. Only about 52% of people get lasting relief, and there’s a real risk: injecting cortisone into a tendon can weaken it and increase the chance of a tear. That’s why the real fix for tendinitis is movement - but not just any movement. Eccentric strengthening is key. That means slowly lowering a weight after lifting it. For Achilles tendinitis, that’s heel drops: stand on a step, rise up on your toes, then slowly lower your heel below the step. Do 3 sets of 15 reps, twice a day, for 12 weeks. It’s boring, it’s hard, but it works - 68% of people see long-term improvement. The worst thing you can do? Push through the pain. If your pain hits 5 or higher on a 10-point scale during activity, you’re damaging tissue, not healing it. Physical therapists call it the "3-point rule": stay under 3/10 pain during rehab. That’s therapeutic discomfort - not injury. Many people try to self-diagnose. Reddit users in r/PhysicalTherapy say 68% of those who thought they had "rotator cuff tendinitis" were actually dealing with bursitis. They were doing shoulder strengthening exercises that made their pain worse. Once they switched to rest and ice, their pain dropped in under a month. Work and lifestyle matter a lot. Construction workers who kneel all day have an 18.4% chance of developing bursitis in their knees. Musicians? One in five develop tendinitis from repetitive finger motions. Office workers get it from typing or mouse use. The fix isn’t just medical - it’s ergonomic. Raise your monitor to eye level. Use a standing desk. Switch hands when you can. These small changes cut recurrence by 82%, according to Arthritis Today’s 2023 survey. If nothing helps after 6-8 weeks, it’s time to see a specialist. Most cases resolve with conservative care. Surgery is needed in fewer than 5% of patients. But if you’ve had pain for more than six months, you might have tendinopathy - a degenerative change, not active inflammation. That means anti-inflammatories won’t help as much. Platelet-rich plasma (PRP) injections are showing promise here, with one 2023 study showing 67% improvement at six months, compared to 42% with cortisone. Wearable tech is starting to help too. Apple Watch’s motion tracking can now detect abnormal movement patterns linked to tendinitis risk with 89% accuracy. It won’t diagnose you, but it can warn you before you’re in pain - like a fitness tracker that says, "You’ve been typing with your wrist bent too long. Adjust your posture." The bottom line? Don’t ignore joint pain just because it’s "common." Bursitis and tendinitis are treatable - but only if you treat them right. Rest the bursa. Strengthen the tendon. Avoid the movements that hurt. And if you’re not sure which one you have, get an ultrasound. It’s faster, cheaper, and more accurate than guessing. And skip the opioids. The CDC found 12.7% of tendinitis patients get prescribed them - even though guidelines say they shouldn’t. Painkillers mask the problem. They don’t fix it. And they carry serious risks. Healing takes time. Bursitis often clears in 4-6 weeks. Tendinitis? 12-16 weeks. Patience isn’t optional. It’s the treatment.
What causes bursitis and tendinitis?
Repetitive motion is the #1 cause. It doesn’t have to be sports. It could be painting ceilings, carrying heavy bags, typing all day, or even gardening. Aging plays a role too - after 40, your tendons and bursae lose elasticity and become more prone to irritation. Obesity adds pressure to joints, especially hips and knees. Poor posture or muscle imbalance can also throw off how your joints move, putting extra stress on tendons and bursae.Can bursitis or tendinitis go away on its own?
Yes, but only if you stop doing what caused it. If you keep lifting weights, typing, or kneeling, the inflammation won’t settle. Rest is non-negotiable. Most people see improvement within a few weeks if they modify their activity. But if you ignore it, it can turn chronic - meaning the pain sticks around for months or years.Is heat or ice better for bursitis and tendinitis?
Ice is better in the first 48-72 hours. It reduces swelling and numbs the pain. After that, heat can help loosen stiff muscles around the joint - but never apply heat if the area is still swollen or red. For bursitis, ice massage with a frozen water bottle is more effective than just holding an ice pack. For tendinitis, ice before and after activity helps control flare-ups.Can I still exercise with tendinitis or bursitis?
Yes - but not the same way. Avoid the exact motion that hurts. If your shoulder hurts when you reach overhead, don’t do overhead presses. But you can still do lower-body workouts, swimming (if it doesn’t strain your shoulder), or cycling. Movement keeps blood flowing and prevents stiffness. Just avoid aggravating the area. Physical therapists recommend low-impact, pain-free motion.When should I see a doctor?
See a doctor if: - Pain lasts more than two weeks despite rest and ice - You can’t move the joint normally - The area is red, hot, or swollen - that could mean infection - You have a fever along with joint pain - You feel a pop or snap during movement - could be a tendon tear Don’t wait until it’s unbearable. Early treatment cuts recovery time in half.
Are cortisone shots safe?
They’re safe when used correctly - but only for bursitis. For tendons, they’re risky. One injection can help for months. Two or three a year is usually okay. More than that weakens tissue. Studies show injecting cortisone into a tendon increases the risk of rupture by up to 30%. That’s why many doctors now avoid it for tendinitis unless all else fails.What’s the difference between tendinitis and tendinopathy?
Tendinitis means active inflammation - swelling, redness, heat. Tendinopathy means degeneration - the tendon has broken down over time from overuse, with little to no inflammation. Most chronic cases (over 3 months) are tendinopathy, not tendinitis. That’s why anti-inflammatories often don’t work. The fix is strengthening, not steroids.Can I prevent these conditions?
Absolutely. Warm up before activity. Stretch after. Strengthen the muscles around your joints - strong muscles take pressure off tendons and bursae. Take breaks during repetitive tasks. Use padding when kneeling. Improve your posture. And listen to your body. That twinge? It’s your body saying, "Ease up."How long does recovery take?
Bursitis: 4-6 weeks with rest and ice. Tendinitis: 12-16 weeks with eccentric training. Chronic cases can take longer. The key is consistency. Skipping rehab days delays recovery. Stick to the plan - even when it feels boring.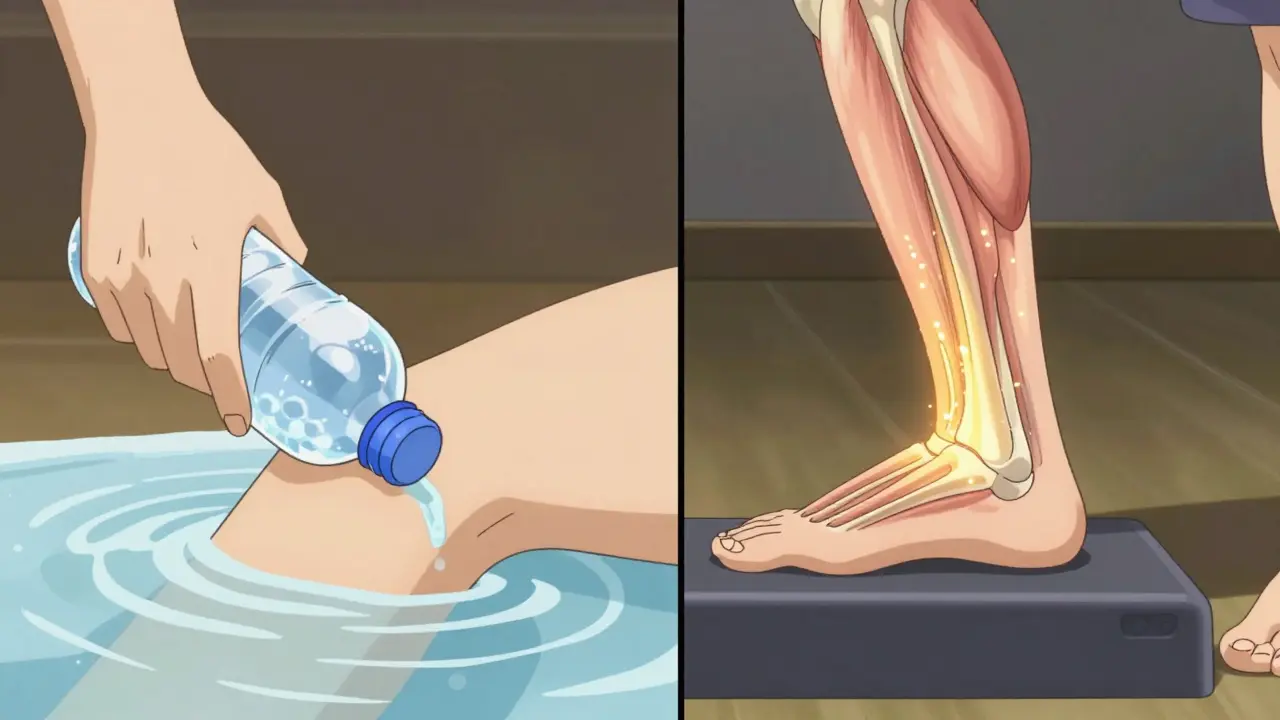
Do I need an MRI?
No, not usually. Ultrasound is just as good, cheaper, and faster. MRI is only needed if you’ve tried everything and still have pain, or if your doctor suspects a tear. Most people don’t need imaging at all - their diagnosis comes from symptoms and physical exam.What’s the most common mistake people make?
They assume it’s just "overuse" and push through the pain. Or they get a cortisone shot and think they’re cured, then go right back to the same activity. Pain relief isn’t healing. Healing takes time, patience, and the right kind of movement. Don’t rush it.What’s the best home remedy?
Ice massage with a frozen water bottle. It’s cheap, easy, and effective. Roll it over the sore spot for 5-10 minutes, twice daily. Combine it with posture correction and avoiding repetitive motions. Most people who do this see results in under two weeks.Can diet help?
Anti-inflammatory foods - like fatty fish, berries, nuts, leafy greens - may help reduce overall body inflammation. But they won’t fix bursitis or tendinitis alone. They’re a support tool, not a cure. The real fix is rest, movement, and avoiding triggers.Will I get this again?
If you don’t change what caused it, yes. Recurrence rates are high - up to 40% within a year if you return to the same activity without modifying your technique or workload. Prevention isn’t optional. It’s the next step after recovery.How do I know if I have bursitis or tendinitis?
Bursitis causes deep, dull pain that worsens with pressure - like lying on your hip or elbow. Tendinitis causes sharp, movement-related pain along the path of the tendon - like pain when lifting your arm or pointing your toes. If you’re unsure, see a doctor for an ultrasound - it’s the most accurate way to tell them apart.
Can I treat bursitis at home?
Yes. Rest the area, apply ice for 15-20 minutes 2-3 times a day, and avoid activities that press on the bursa. Use a cushion when kneeling. Most cases improve within 4-6 weeks. If pain persists, see a doctor for possible cortisone injection.
Is tendinitis permanent?
No. Even chronic tendinitis (tendinopathy) can improve with the right rehab. Eccentric strengthening exercises - like heel drops for Achilles pain - have a 68% success rate over 6 months. But it takes time and consistency. Rushing back to activity causes relapse.
Should I stretch if I have tendinitis?
Gentle stretching helps maintain mobility, but don’t force it. The real fix is eccentric strengthening - slowly lowering a weight after lifting it. Stretching alone won’t heal a degenerated tendon. Combine it with strengthening for best results.
Are cortisone injections dangerous for tendinitis?
Yes, if injected directly into the tendon. Cortisone can weaken tendon tissue and increase the risk of rupture. For tendinitis, injections are less effective and riskier than for bursitis. Physical therapy and eccentric exercises are safer and more effective long-term.
When should I consider surgery?
Surgery is rarely needed - fewer than 5% of cases. It’s only considered after 6-12 months of failed conservative treatment, especially if there’s a confirmed tendon tear. Most people recover without it.
Can I use a brace or wrap?
Yes, for short-term support. A compression sleeve or strap can reduce strain on a tendon during activity. But don’t rely on it long-term. It doesn’t heal the problem - it just masks it. Focus on correcting movement and strengthening instead.
Does age affect recovery?
Yes. After age 40, tendons and bursae heal slower due to reduced blood flow and tissue elasticity. That’s why recovery takes longer for older adults. But with proper rehab, full recovery is still possible - it just requires more patience.
Can I prevent bursitis and tendinitis from coming back?
Yes. Strengthen the muscles around your joints, improve your posture, take breaks during repetitive tasks, and avoid pushing through pain. Use padding when kneeling. Modify your workstation. Prevention isn’t optional - it’s the key to staying pain-free long-term.
What’s the most effective long-term treatment for tendinitis?
Eccentric strengthening. For Achilles tendinitis, that’s heel drops. For shoulder tendinitis, it’s controlled lowering of weights with a band or dumbbell. Do 3 sets of 15 reps, twice daily, for 12 weeks. Studies show 68% of patients achieve lasting relief with this method - far better than injections or rest alone.

asa MNG
January 26, 2026 AT 08:12Marie-Pier D.
January 27, 2026 AT 12:06Jenna Allison
January 28, 2026 AT 20:42Alexandra Enns
January 29, 2026 AT 13:45Vatsal Patel
January 30, 2026 AT 15:25John McGuirk
January 31, 2026 AT 22:03Kat Peterson
February 1, 2026 AT 22:59Viola Li
February 1, 2026 AT 23:21Dolores Rider
February 3, 2026 AT 23:03