Complex Regional Pain Syndrome: Burning Pain After Injury
 Jan, 3 2026
Jan, 3 2026
After a broken wrist, a sprained ankle, or even a minor cut, most people expect pain to fade over weeks. But what if the pain doesn’t just stick around-it grows worse? What if your skin feels like it’s on fire from the lightest touch, your limb swells for no reason, and the temperature of your hand or foot changes without explanation? This isn’t normal healing. This could be Complex Regional Pain Syndrome-a misunderstood, often misdiagnosed condition that turns a simple injury into a lifelong battle.
What Exactly Is CRPS?
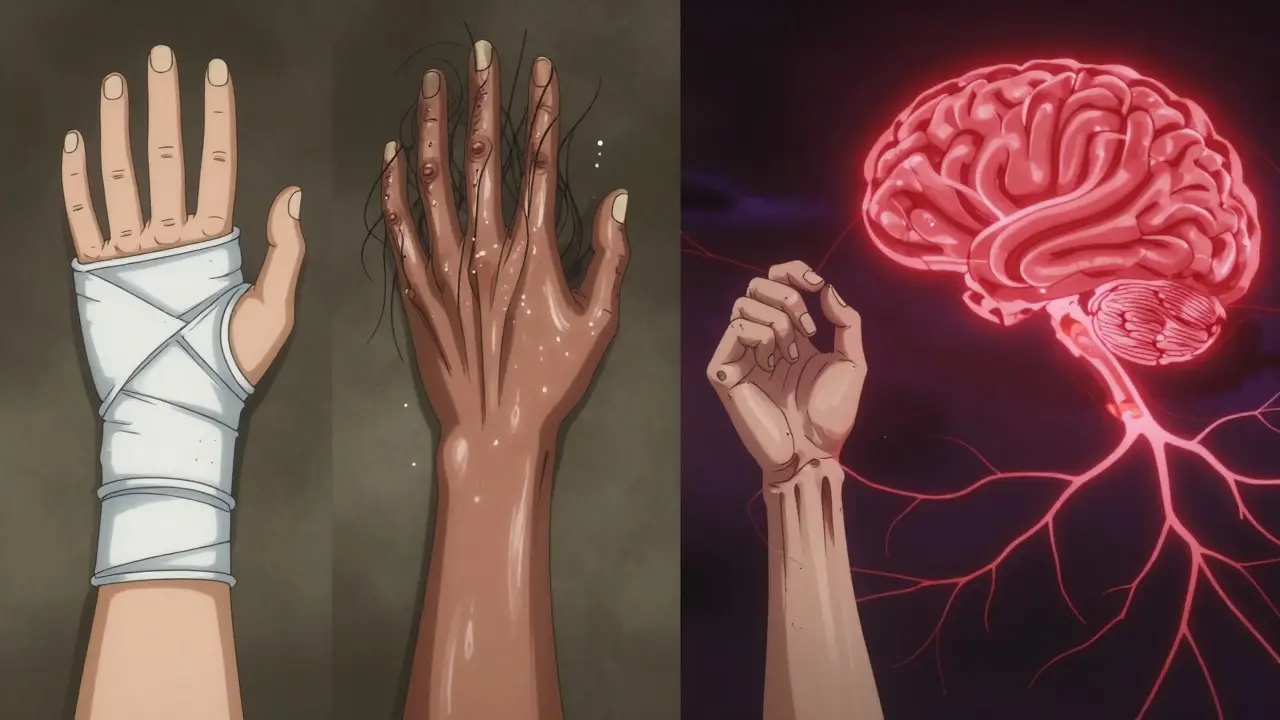
Complex Regional Pain Syndrome, or CRPS, is a neurological disorder where the nervous system goes haywire after an injury. It’s not just pain-it’s pain that’s out of proportion, persistent, and often spreads beyond the original site. The burning, stabbing, or electric shock-like sensation doesn’t match the severity of the initial trauma. A stubbed toe doesn’t cause months of agony. A broken wrist shouldn’t make your fingers feel like they’re being held in a flame. Yet for people with CRPS, that’s exactly what happens.
There are two types. Type I, which makes up about 90% of cases, happens without a clear nerve injury-often after a fracture, sprain, or surgery. Type II occurs after a confirmed nerve injury, like a cut nerve during an operation. Both trigger the same brutal symptoms. It’s not a muscle strain. It’s not inflammation alone. It’s your nerves misfiring, sending constant danger signals to your brain even when there’s no real threat.
Why Does the Pain Feel So Extreme?
CRPS doesn’t just hurt-it changes your body. The affected limb might turn red, purple, or pale. Skin can become thin, shiny, or sweaty. Hair and nails may grow faster-or stop growing altogether. You might notice your injured hand is 1°C warmer or cooler than the other. That’s because CRPS messes with your autonomic nervous system, the part that controls blood flow, sweat, and temperature without you thinking about it.
One of the most terrifying symptoms is allodynia-pain from something that shouldn’t hurt at all. A light blanket, a breeze, or even the brush of clothing can feel like glass under your skin. Some people can’t tolerate a watch, a bracelet, or a sock. This isn’t weakness. It’s your nervous system stuck in overdrive, amplifying every signal like a broken alarm that can’t be turned off.
Studies show that in early stages, inflammation plays a big role. Immune cells flood the area, releasing chemicals that irritate nerves. Over time, the brain itself changes-neural pathways become wired to expect pain, even after the injury heals. This is called central sensitization. Your brain learns to feel pain constantly, making it harder to reverse later.
Who Gets CRPS-and Why?
CRPS doesn’t pick favorites, but it does have patterns. Women are three times more likely to develop it than men. It’s most common between ages 40 and 60, but teenagers and older adults get it too. You don’t need a major injury. A fracture accounts for about 40% of cases, especially wrist fractures. Surgery, especially on the hand or foot, is another common trigger. Even minor trauma-a bump, a burn, or a cast that’s too tight-can set it off.
And here’s the frustrating part: no one knows why some people get it and others don’t. Two people break the same bone. One heals fine. The other develops CRPS. There’s no blood test. No X-ray shows it. Some researchers suspect genetics or immune system quirks, but no clear link has been proven. That’s why so many patients are told it’s "all in their head"-because doctors still don’t fully understand it.

When Does It Start?
CRPS doesn’t show up overnight. Most people notice symptoms four to six weeks after the injury. That delay is why it’s often missed. A patient comes in with a healed fracture, but their wrist still burns. Their doctor thinks it’s scar tissue. Or they blame arthritis. By the time CRPS is suspected, the condition may have progressed.
There are three stages, but not everyone goes through them all-and they don’t always follow a clear order.
- Stage 1 (0-3 months): Burning pain, swelling, skin changes, temperature shifts, increased sweating, stiff joints, faster nail/hair growth.
- Stage 2 (3-6 months): Pain spreads, skin becomes cooler and more pale, nails become brittle, muscles weaken, stiffness worsens.
- Stage 3 (6+ months): Pain may become constant and spread further. Muscles atrophy, joints harden, movement becomes very limited. At this point, damage can be irreversible.
But here’s the key: not everyone progresses. Some stay in Stage 1. Others skip stages. Early recognition is everything.
How Is CRPS Diagnosed?
There’s no scan for CRPS. No blood test. No MRI that shows it clearly. Diagnosis relies on the Budapest Criteria, a set of clinical signs doctors use to spot it. You must have:
- Pain that’s ongoing and disproportionate to the injury
- At least one symptom in three of these four categories: sensory (like burning or allodynia), vasomotor (temperature/skin color changes), sudomotor/edema (swelling or sweating), motor/trophic (weakness, tremors, hair/nail changes)
- No other condition that explains the symptoms
Doctors also rule out other causes-like nerve compression, infection, or arthritis. If you’ve had an injury and your pain doesn’t improve with normal healing, and you have these signs, CRPS is likely. The earlier it’s caught, the better the outcome.
What Treatments Actually Work?
CRPS isn’t cured with painkillers. Regular NSAIDs or even opioids rarely help. The goal isn’t to mask pain-it’s to reset the nervous system.
Physical therapy is the cornerstone. Early movement is critical. Many patients avoid using the limb because it hurts-only to make it worse. A skilled therapist will guide you through gentle exercises, desensitization techniques, and mirror therapy (where you watch the unaffected limb move, tricking your brain into thinking the injured one is moving too). This helps rewire the brain’s pain map.
Medications are used strategically:
- NSAIDs and corticosteroids help in early stages if inflammation is active.
- Neuropathic pain drugs like gabapentin, pregabalin, or amitriptyline target nerve signals.
- Sympathetic nerve blocks can temporarily shut down overactive nerves, giving your system a reset.
- Spinal cord stimulation sends mild electrical pulses to block pain signals before they reach the brain.
- Ketamine infusions are being studied for severe cases, showing promise in resetting neural pathways.
For some, CRPS improves over time-sometimes within months. But for others, pain lasts years. The difference often comes down to timing. People who start treatment within the first three months have a much better chance of recovery.
The Hidden Toll: Mental Health and Isolation
CRPS doesn’t just hurt your body-it steals your life. Sleep is disrupted. Work becomes impossible. Social plans vanish. You can’t hold your child, carry groceries, or even wear a watch. Many patients report depression, anxiety, and PTSD from the relentless pain and lack of understanding.
Doctors often don’t know how to help. Friends and family may think you’re exaggerating. Some are told they’re just stressed. That kind of invalidation adds another layer of trauma. Support groups and psychological counseling aren’t optional-they’re part of treatment. Cognitive behavioral therapy helps you cope, manage flare-ups, and rebuild a sense of control.
What’s Next for CRPS Research?
Scientists are now looking at autoimmunity. A 2022 study found specific antibodies in 30% of CRPS patients-suggesting the body might be attacking its own nerves. Other research focuses on biomarkers to make diagnosis faster and more accurate. Clinical trials are testing new drugs that calm neuroinflammation and reset nerve function.
The big hope? Personalized treatment. If we can identify whether someone’s CRPS is driven more by inflammation, nerve damage, or brain changes, we can tailor therapy instead of guessing.
But for now, the message is simple: if you’ve had an injury and your pain is burning, spreading, or getting worse instead of better-don’t wait. Don’t accept it as normal. Ask about CRPS. See a pain specialist. Get moving. Early action saves limbs, careers, and lives.
Can CRPS go away on its own?
Yes, some cases resolve without treatment, especially if caught early. But waiting is risky. Studies show that up to 70% of people who get early, aggressive therapy see major improvement. Without treatment, pain can become permanent, and mobility may be lost. Don’t rely on spontaneous recovery-act fast.
Is CRPS the same as fibromyalgia?
No. Fibromyalgia causes widespread, diffuse pain across the body, often with fatigue and sleep issues. CRPS is localized to one limb and follows a specific injury. CRPS includes visible changes like skin color, temperature, and swelling-signs you don’t see in fibromyalgia. The mechanisms are different, and treatments don’t overlap much.
Can stress cause CRPS?
Stress doesn’t cause CRPS, but it can make it worse. Emotional stress triggers the nervous system, which can amplify pain signals in someone already with CRPS. That’s why therapy and stress management are part of treatment-not because it’s "all in your head," but because your nervous system responds to mental state.
Does a cast or bandage cause CRPS?
A cast or bandage doesn’t cause CRPS, but if it’s too tight or restricts movement, it can trigger it in someone who’s already at risk. Feeling like your cast is too tight after an injury is a red flag. Talk to your doctor immediately-loosening it or adjusting it might prevent CRPS from developing.
Is CRPS rare?
It’s not common, but it’s not ultra-rare either. Estimates suggest 20 to 26 cases per 100,000 people per year. Because it’s often misdiagnosed, the real number is likely higher. It’s more common after fractures and surgeries than most doctors realize.

Jay Tejada
January 4, 2026 AT 00:26Been there. Broke my wrist skiing, thought it was just bad healing. Then my hand started screaming at me for no reason. One day I brushed it with my other hand and nearly passed out. Took six months to get anyone to listen. Now I’m three years in and still fighting. But hey-at least I can type now. 🤷♂️
Allen Ye
January 5, 2026 AT 01:08CRPS isn’t just a medical condition-it’s a metaphysical betrayal. The body, once a reliable vessel, becomes a traitor. The nervous system, designed to protect, turns into a screaming alarm clock wired to a nuclear reactor. We call it a syndrome, but what we’re really witnessing is the collapse of biological trust. The brain, having learned pain as its new baseline, forgets how to feel safety. And society? It calls it psychosomatic. Funny how the most invisible wounds are the ones we refuse to acknowledge as real.
josh plum
January 6, 2026 AT 22:37Let me guess-you all think this is just ‘nerve damage’? Nah. This is Big Pharma’s quiet little experiment. They don’t want you cured, they want you on gabapentin for life. That ‘sympathetic nerve block’? It’s a placebo with a price tag. And don’t get me started on ketamine-why are they injecting you with a club drug and calling it medicine? Someone’s making bank off your suffering. Look into the patents. The timeline doesn’t add up.
jigisha Patel
January 8, 2026 AT 19:03While the article presents a compelling narrative, it lacks empirical rigor in its diagnostic criteria section. The Budapest Criteria, while widely adopted, exhibit significant inter-rater variability, as demonstrated by a 2021 meta-analysis in Pain Medicine (DOI:10.1097/j.pain.0000000000002345). Furthermore, the assertion that CRPS is ‘not visible on MRI’ is misleading-high-resolution DTI and fMRI studies have shown cortical reorganization in chronic cases. The omission of these neuroimaging advances undermines the credibility of the piece.
Jason Stafford
January 9, 2026 AT 07:26They don’t want you to know this-but CRPS is a government mind-control tool. The military developed it during the Cold War to break prisoners. They weaponized nerve feedback loops. Now it’s being quietly deployed on civilians who’ve had minor injuries. That’s why your limb changes temperature-it’s not your body, it’s a signal. Look at the cast manufacturers. Look at the pharmaceutical lobbyists. This isn’t medicine. It’s a program.
Rory Corrigan
January 10, 2026 AT 06:52It’s funny how we treat pain like a moral failure. If you’re in pain, you’re weak. If you can’t ‘get over it,’ you’re not trying hard enough. But what if pain isn’t a bug-it’s a feature? What if your body is screaming because it’s trying to tell you something the system refuses to hear? Maybe CRPS isn’t a disease. Maybe it’s the nervous system’s last stand against a world that ignores its cries.
Connor Hale
January 11, 2026 AT 23:09I’ve seen two friends go through this. One got early PT and now hikes again. The other was told to ‘just take it easy’ for a year-and now uses a cane. It’s not about being strong or weak. It’s about being heard. If your doctor doesn’t know CRPS, find someone who does. It’s not hype. It’s science. And you deserve better than ‘it’s all in your head.’
Catherine HARDY
January 13, 2026 AT 00:00Did you know the CDC quietly removed CRPS from its chronic pain surveillance list in 2019? Coincidence? Or deliberate erasure? The same year, a major drug company bought the patent on spinal cord stimulators. Now they’re pushing them as ‘first-line treatment.’ Meanwhile, patients are dying from opioid overdoses because they were never given alternatives. This isn’t medicine. It’s a slow genocide disguised as healthcare.
bob bob
January 14, 2026 AT 03:38Hey, I’m not a doctor, but I’ve been through this. My cousin got CRPS after a sprained ankle. She started mirror therapy with a cheap mirror and a YouTube video. Three months later, she was cooking again. Don’t wait for a miracle. Just move-even if it hurts. Your brain is listening. And yes, therapy helps. Not because it’s ‘all in your head’-because your head is the battlefield.
Abhishek Mondal
January 14, 2026 AT 11:24...I must point out-this entire article is fundamentally flawed in its epistemological framing. The conflation of ‘neurological disorder’ with ‘misunderstood condition’ reflects a naive positivist bias. CRPS is not ‘misunderstood’-it is systematically suppressed by institutionalized biomedical hegemony. Furthermore, the reference to ‘Stage 3’ as irreversible is empirically dubious-neuroplasticity research since 2020 demonstrates remapping even after 12 years. Your article is not just incomplete-it is complicit in the medicalization of suffering.
Joseph Snow
January 14, 2026 AT 21:44Let’s be clear: this is not a syndrome. It’s a failure of the medical system. You break your wrist. You get a cast. You’re told to rest. You don’t move. You develop stiffness. You get pain. You’re labeled ‘CRPS’ because no one wants to admit they gave you bad advice. It’s not a neurological disorder-it’s iatrogenic. Stop pretending this is some mysterious disease. It’s negligence dressed up in jargon.
melissa cucic
January 16, 2026 AT 09:35Thank you for this comprehensive overview. I particularly appreciate the emphasis on early intervention. As a physiotherapist with over a decade of experience in pain management, I can confirm that the window for effective neuroplastic retraining is narrow-often less than 90 days. Delayed referral to multidisciplinary pain clinics correlates strongly with poorer long-term outcomes. The inclusion of psychological support is not ancillary-it is foundational.
Akshaya Gandra _ Student - EastCaryMS
January 17, 2026 AT 21:07wait so if u get a cut and then ur skin burns like its on fire its crps? i had that after i cut my finger and it was weird but it went away in a week?? so does that mean i almost had it??
Jacob Milano
January 19, 2026 AT 17:26CRPS is the silent scream of a body that’s been abandoned by the system. It’s the ghost in the machine-the pain that doesn’t fit the map. But here’s the beautiful, brutal truth: your nervous system didn’t break. It learned. And if it learned pain, it can unlearn it. Not with pills. Not with silence. But with movement, with touch, with someone who sees you-not your symptoms. You’re not broken. You’re just screaming louder than the world is willing to listen. Keep screaming. We’re here.