First-Episode Psychosis: Why Early Intervention and Family Support Save Lives
 Jan, 27 2026
Jan, 27 2026
When someone experiences their first episode of psychosis, everything changes. They might hear voices no one else can hear, believe things that aren’t true, or start speaking in ways that don’t make sense. It’s terrifying-for them, and for everyone around them. But here’s the truth most people don’t know: first-episode psychosis is not a life sentence. With the right help, quickly and with family support, most people recover and go on to live full, meaningful lives.
What Happens During a First Episode of Psychosis?
First-episode psychosis isn’t one single symptom. It’s a cluster of experiences that break a person’s connection to reality. Hallucinations-like hearing whispers, screams, or commands-are common. Delusions, such as believing they’re being watched, followed, or chosen for a special mission, happen too. Thoughts get jumbled. Speech becomes hard to follow. Emotions shift without warning. Some people withdraw completely. Others become agitated or aggressive.
This isn’t just "being odd" or "going through a phase." It’s a medical event. The brain is in crisis. Research shows that the longer psychosis goes untreated, the more damage it does. A delay of just 3 to 6 months can lead to lasting problems with memory, focus, motivation, and relationships. The brain’s ability to recover weakens over time. That’s why timing isn’t just important-it’s everything.
The 12-Week Window: Why Speed Matters
The World Health Organization says treatment should start within 12 weeks of the first signs. Why? Because this is the "window of opportunity." During this time, the brain is still trying to adapt. It’s plastic-capable of change. Early treatment doesn’t just reduce symptoms. It protects the person’s ability to return to school, work, and social life.
One major study, the RAISE project, followed over 400 people with first-episode psychosis. Those who got coordinated specialty care (CSC) within 12 weeks were 45% more likely to have their symptoms fully ease compared to those who waited longer. They stayed in treatment longer, returned to school or work at twice the rate, and reported much higher quality of life. Those who waited more than 6 months? Their recovery was slower, harder, and often incomplete.
Think of it like a broken bone. The sooner you set it, the better it heals. Delay treatment, and you risk permanent misalignment.
What Is Coordinated Specialty Care (CSC)?
CSC isn’t just one doctor, one pill, or one therapy. It’s a team. A group of trained professionals working together-psychiatrists, therapists, case managers, employment coaches, and peer support specialists-all focused on one person’s recovery.
There are five core parts:
- Case Management: Someone helps the person navigate appointments, insurance, housing, and transportation. They call weekly, sometimes more, especially in the early weeks.
- Medication Management: Antipsychotic meds are started at the lowest effective dose. High doses? They’re dangerous. The National Institute for Health and Care Excellence warns against doses over 400mg chlorpromazine equivalent-they don’t work better, but they cause more weight gain, diabetes, and heart problems.
- Psychotherapy: Cognitive behavioral therapy (CBT) tailored for psychosis helps people understand their experiences, reduce fear, and build coping skills. Sessions are weekly at first.
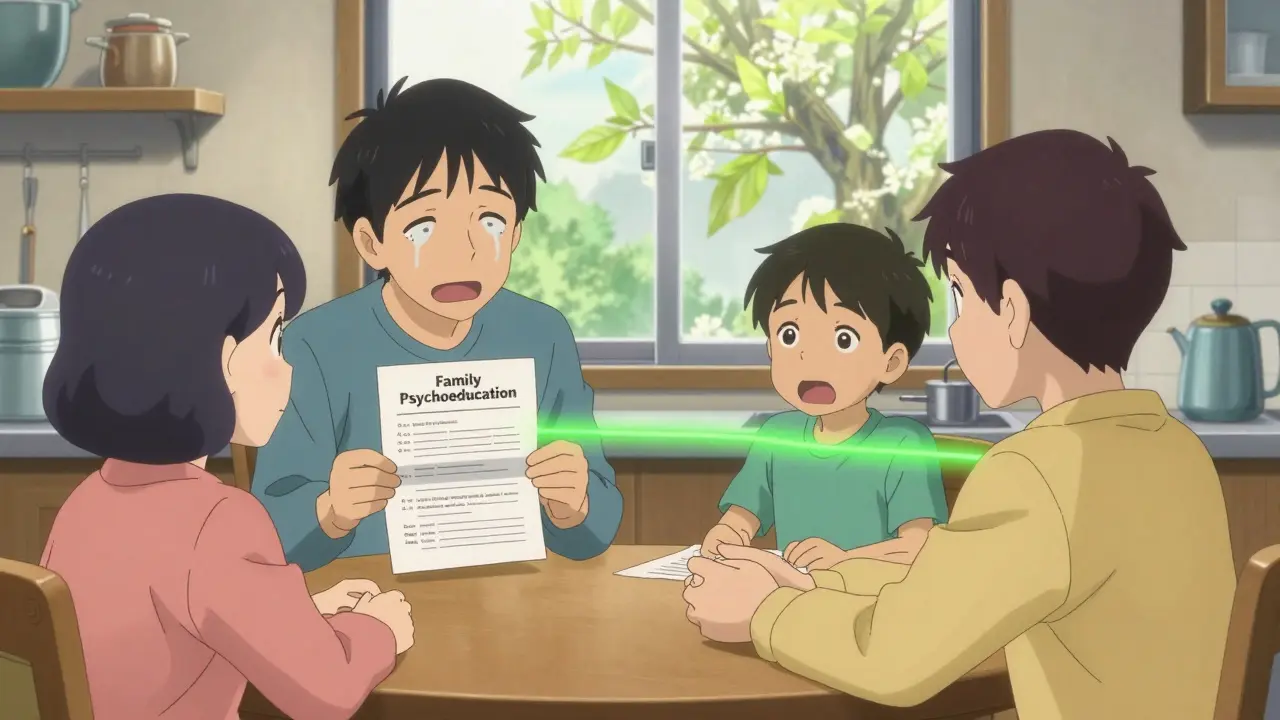
- Family Psychoeducation: Families get trained. Not just to "understand"-but to respond in ways that help. This isn’t optional. It’s essential.
- Supported Employment and Education: The goal isn’t just to feel better. It’s to live again. Programs like Individual Placement and Support (IPS) help people get back to school or work. Studies show 50-60% of those in CSC find competitive jobs or return to school. In standard care? Only 20-30% do.
CSC teams meet weekly to talk about each person’s progress. They’re held to strict standards. Programs must hit at least 70% adherence to the model to be certified. That’s how you know it’s real-not just a label.

Why Family Support Isn’t Optional
Families are the first line of defense. They’re often the ones who notice the changes first. But many don’t know what to do. They panic. They argue. They isolate. Or worse-they blame the person.
Family psychoeducation changes that. It’s not a lecture. It’s a course. Usually 8 to 12 sessions over 6 months. Families learn:
- What psychosis actually is (and what it isn’t)
- How to talk without triggering stress
- How to recognize early warning signs of relapse
- How to set healthy boundaries without abandonment
The results? A 25% drop in relapse rates. That’s huge. People who have involved families are far less likely to end up in the hospital or lose their job. They’re more likely to stick with treatment.
And yet, only 55% of eligible families actually join these programs. Barriers? Shame. Fear. Lack of transportation. Language differences. Programs in Louisiana and Washington State fixed this by offering telehealth sessions, mobile crisis teams, and peer-led support groups. They met families where they were.
What’s Missing? The System Is Broken
Here’s the hard part: most people never get CSC. Only 35% of U.S. counties have even one certified program. In rural areas? That number drops to 62% without any access. And only 18% of people with first-episode psychosis get treatment within the 12-week window.
Why? Money. Workforce shortages. Insurance gaps. Medicaid covers CSC in only 31 states. The rest? Families pay out of pocket-or get nothing. CSC costs about $8,000 to $12,000 per person per year. Standard care? $5,000 to $7,000. But here’s the catch: untreated psychosis costs the U.S. $155 billion a year in lost jobs, emergency visits, homelessness, and incarceration. CSC cuts that cost by more than 80%.
Workforce turnover is another crisis. One in five CSC team members leaves every year. Training takes 40 hours of classroom time plus 120 hours of supervised practice. There aren’t enough trained people. And the ones who are? They’re burned out.
What’s Working? Real Examples
Washington State’s New Journeys program has served over 2,800 people since 2016. Their teams hit 95% fidelity scores-meaning they follow the model perfectly. The average time from first symptom to treatment dropped from 78 weeks to just 26 weeks.
Massachusetts trained 347 clinicians through a strict competency program. Louisiana created mobile crisis units that show up at homes within 14 days. Telehealth boosted family participation by 35% during the pandemic.
And now, new tools are emerging. Apps like "PRIME Care" let people log mood, sleep, and symptoms daily. Early results show 30% fewer hospitalizations. The National Institute of Mental Health is investing $50 million through 2026 to find biological markers that can detect psychosis before it fully hits.
What You Can Do
If you suspect someone is having their first episode:
- Don’t argue with their beliefs. Say, "I see this is really scary for you. I’m here."
- Don’t wait. Contact a mental health provider or crisis line immediately.
- Ask: "Is there a Coordinated Specialty Care program nearby?" Use the EPINET registry to find one.
- Reach out to NAMI or the National Council for Mental Wellbeing. They offer free training for families.
- Push for insurance coverage. If it’s denied, appeal. CSC is proven. It’s not experimental.
If you’re a family member: Take the training. Go to the sessions. Even if you’re angry, scared, or confused-you matter. Your presence changes outcomes.
If you’re a clinician: Don’t start with high-dose antipsychotics. Don’t skip family involvement. Don’t assume the person will "get better on their own." The data is clear. Early, coordinated care saves lives.
There’s Hope
First-episode psychosis is not the end. It’s a turning point. With fast, compassionate, team-based care, people don’t just survive-they thrive. They graduate. They get jobs. They start families. They contribute.
The science is settled. The models exist. What’s missing is access. And political will. But change starts with awareness. If you know someone in crisis, don’t wait. Don’t assume it’s "just stress." Act. Now. Because the clock is ticking-and every day without help costs them more than you can imagine.
What are the first signs of psychosis?
Early signs include social withdrawal, trouble sleeping, unusual beliefs or suspicions, decreased motivation, strange speech patterns, and a drop in school or work performance. Hallucinations and delusions often come later. Many people dismiss these as "teenage issues" or "stress," but they’re warning signs that need attention.
Is psychosis the same as schizophrenia?
No. Psychosis is a symptom, not a diagnosis. Schizophrenia is one possible outcome after repeated episodes. Many people who have one episode of psychosis never have another. With early treatment, up to 80% recover fully and don’t develop schizophrenia. The goal isn’t to prevent schizophrenia-it’s to prevent disability.
Can medication alone treat first-episode psychosis?
No. Medication helps reduce symptoms, but it doesn’t restore function. People need therapy to rebuild their sense of self, family support to reduce stress, and help returning to school or work. Without these, relapse is common-even if pills are taken regularly.
Why are family members so important in treatment?
Families are the main source of emotional stability. They help notice early warning signs, encourage treatment adherence, and reduce stress triggers like conflict or chaos. Studies show that when families are trained, relapse rates drop by 25%. Their involvement isn’t supportive-it’s therapeutic.
How do I find a Coordinated Specialty Care program near me?
Visit the Early Psychosis Intervention Network (EPINET) registry online. You can search by state or zip code. If none are listed nearby, contact your local NAMI chapter or university hospital psychiatry department. Many programs are affiliated with academic centers and can refer you to the closest one.
What if I can’t afford CSC?
Medicaid covers CSC in 31 states. If you’re in one of them, ask your provider to bill under rehabilitative services. If you’re not, contact SAMHSA’s helpline (1-800-662-HELP) or your state’s mental health department. Some programs offer sliding scale fees or grant-funded slots. Don’t assume it’s too expensive-ask.
Are there risks with antipsychotic medication?
Yes. Second-generation antipsychotics can cause weight gain, high blood sugar, and high cholesterol. That’s why metabolic monitoring starts on day one: weight, waist size, and fasting glucose are checked at baseline and every 3 months. Low doses are safer. High doses are not more effective-they just increase side effects. Always ask: "Is this the lowest dose needed?"
Can someone with psychosis still go to college or hold a job?
Absolutely. In fact, helping people return to school or work is a core part of CSC. The Individual Placement and Support (IPS) model helps them find competitive jobs or enroll in classes with tailored support. Over half of those in CSC programs return to work or school. They don’t need to wait until they’re "100% better." Recovery happens through doing.

Colin Pierce
January 27, 2026 AT 18:01Just saw this and had to say-my cousin went through this last year. We didn’t know what was happening at first. Thought it was just stress from college. By the time we got her into CSC, it had been 5 months. She’s doing amazing now-back in school, working part-time, even started painting again. Early intervention isn’t just helpful-it’s everything. If you’re reading this and someone you love is showing signs, don’t wait. Call someone today.
Kevin Kennett
January 28, 2026 AT 03:58Stop pretending this is just about mental health. This is a systemic failure. The government spends billions on prisons but won’t fund a $10k/year program that keeps people out of them? We’re literally choosing to let people break so we can lock them up later. It’s not ignorance-it’s malice. And if you’re sitting there thinking ‘but what about the budget?’-you’re part of the problem.
Jess Bevis
January 29, 2026 AT 16:38First signs? Withdrawal. Sleep issues. Weird speech. Don’t ignore it.
Howard Esakov
January 30, 2026 AT 15:07Wow. Finally, someone who gets it. 🙌 I’ve been screaming this from the rooftops since my sister’s episode. Medication alone is like putting a bandaid on a broken femur. And families? They’re the unsung heroes. Most therapists don’t even train them properly. But hey, at least we’re talking about it now. Progress, baby! 💪🧠
Kathy Scaman
January 30, 2026 AT 23:16My mom went through this with my brother. She didn’t know where to start. Ended up finding a local NAMI group on Facebook. Best thing she ever did. Learned how to not freak out when he started talking about aliens controlling the microwave. Turns out, that’s a thing. And now he’s got a job at a coffee shop. Small wins, y’all.
Anna Lou Chen
January 31, 2026 AT 19:51Let’s deconstruct the epistemological framework of this ‘early intervention’ paradigm. It assumes a Cartesian duality between ‘normal’ and ‘psychotic’ subjectivities-a colonial, biomedical hegemony that pathologizes altered states of consciousness. What if psychosis isn’t a malfunction but a radical recalibration? The ‘window of opportunity’ rhetoric serves the pharmaceutical-industrial complex. We’re not treating illness-we’re enforcing conformity. 🌌
Lance Long
February 1, 2026 AT 16:37Hey, I’m a therapist who’s trained in CSC. I see the gaps every day. Clinicians are burned out. Families are scared. And insurance companies act like they’re negotiating a car deal. But here’s the truth: you don’t need to fix everything at once. Just show up. Listen. Say, ‘I’m here.’ That’s the first step. And then call EPINET. Seriously. It’s free. They’ll help you find the right program. You’re not alone in this.
fiona vaz
February 2, 2026 AT 09:04My brother had his first episode at 19. We got him into a program within 8 weeks. He’s 27 now, works in IT, and just bought his first car. The meds helped. The therapy helped. But what really made the difference? My mom showing up to every session-even when she was terrified. Family isn’t optional. It’s the foundation.