GLP-1 Agonists for Weight Loss: Real Benefits and Common Side Effects
 Jan, 26 2026
Jan, 26 2026
When you hear about GLP-1 agonists, you might think of celebrities dropping weight on social media. But for millions of people struggling with obesity, these medications are changing lives-not because they’re magic, but because they work differently than anything before. GLP-1 agonists like Wegovy, Ozempic, and Zepbound don’t just suppress appetite. They rewire how your body talks to your brain about food, slow digestion, and help you feel full with less. The results? Real, measurable weight loss-often 10% to over 20% of body weight. But it’s not without trade-offs. Nausea, vomiting, and cost are real barriers. And if you stop taking them, the weight often comes back. This isn’t a quick fix. It’s a long-term tool, and understanding how it works-and what it costs-is critical.
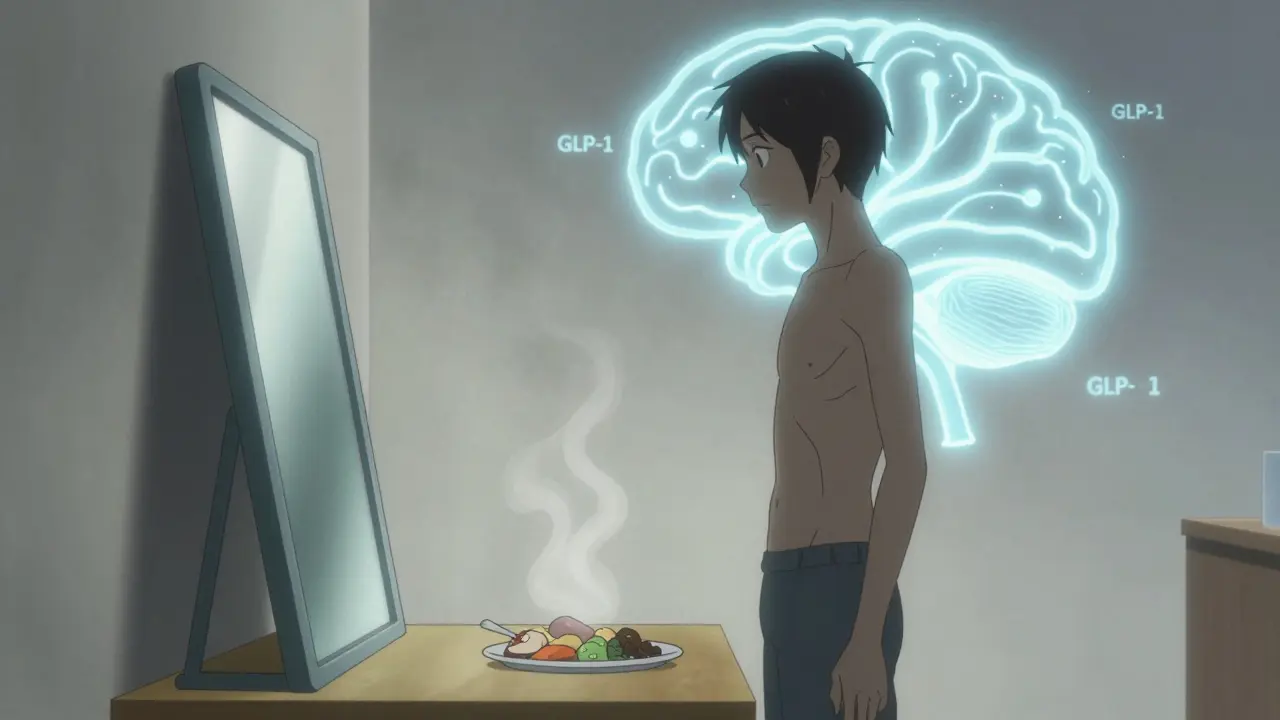
How GLP-1 Agonists Actually Work
GLP-1 agonists mimic a hormone your body already makes after eating. That hormone, glucagon-like peptide-1, tells your brain you’re full and tells your pancreas to release insulin. But in people with obesity or type 2 diabetes, this system doesn’t work well. These drugs boost that signal.
They act on the hypothalamus, the part of your brain that controls hunger. They quiet down the neurons that make you crave food and turn up the ones that say, “I’m done.” At the same time, they slow down your stomach emptying. So food stays in your stomach longer, which means you feel full after smaller meals. It’s not that you’re starving-you just don’t feel the urge to eat as much. In clinical trials, people on semaglutide (Wegovy) reported eating 30% to 50% less without feeling deprived.
These drugs also improve blood sugar control. They help your pancreas release insulin only when blood sugar rises, which reduces spikes and crashes. That’s why they were first approved for diabetes. But the weight loss effect is so strong that the FDA approved Wegovy specifically for obesity in 2021. Tirzepatide (Zepbound) goes even further-it activates two receptors, GLP-1 and GIP, leading to even greater weight loss in trials.
How Much Weight Can You Really Lose?
The numbers are hard to ignore. In the STEP 4 trial, people using Wegovy lost an average of 15.8% of their body weight over 68 weeks. That’s over 35 pounds for someone who weighs 220 pounds. Tirzepatide, in the SURMOUNT-2 trial, hit 20.9%-nearly 46 pounds on the same weight. Compare that to older weight loss drugs: orlistat (Xenical) gives you 5-10%, phentermine-topiramate (Qsymia) around 7-10%. GLP-1 agonists aren’t just better-they’re in a different league.
What’s even more surprising? About half of people on semaglutide lost 15% or more of their body weight. That’s the kind of loss usually seen after bariatric surgery. And it’s not just about the scale. People report better energy, lower blood pressure, improved cholesterol, and fewer diabetes symptoms. The SUSTAIN-6 trial showed a 26% reduction in major heart events for people with diabetes taking semaglutide. For many, this isn’t just weight loss-it’s disease prevention.
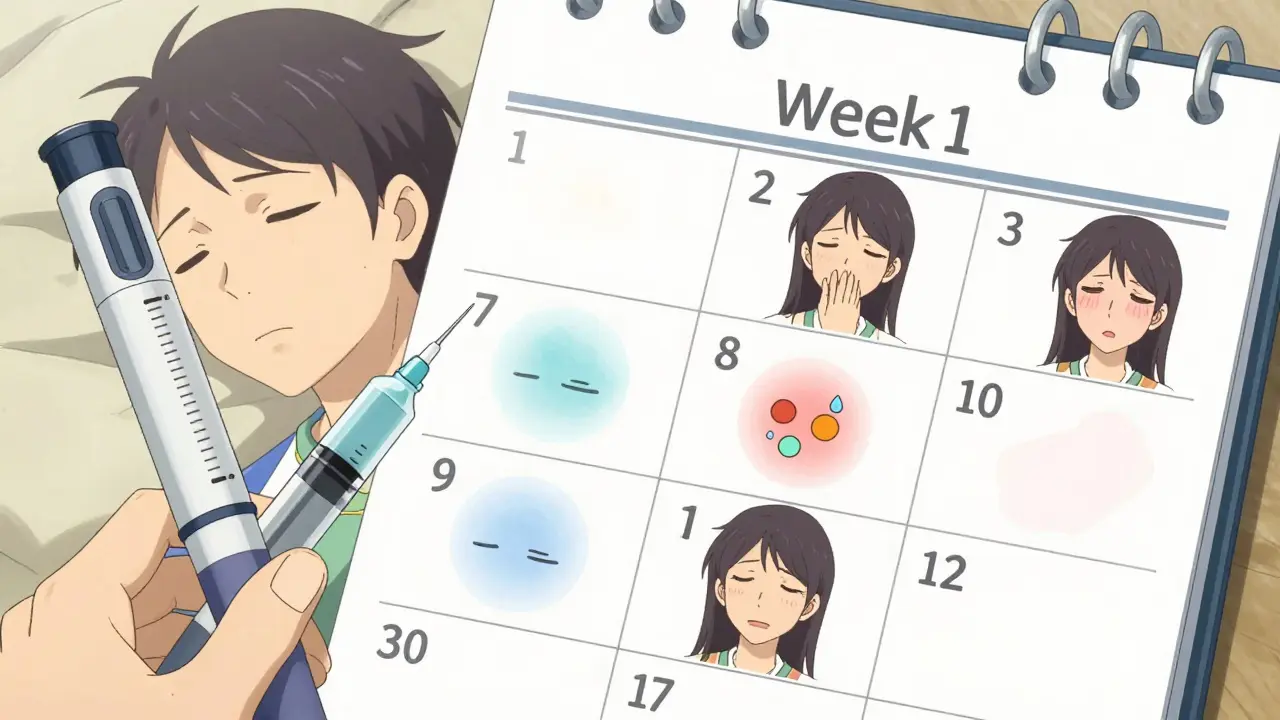
The Side Effects: Nausea, Vomiting, and What to Do About Them
Here’s the catch: most people experience gastrointestinal side effects. Up to 80% of users report nausea, especially in the first few weeks. Around 60% get diarrhea, 50% vomit, and 40% have abdominal pain. These aren’t rare side effects-they’re the norm.
The good news? They usually fade. In most cases, symptoms drop significantly after 8 to 12 weeks. That’s why dose titration is so important. Wegovy doesn’t start at 2.4 mg. It begins at 0.25 mg weekly and increases every four weeks until you hit the full dose. Rushing this process makes side effects worse. Many people quit because they think it’s not working-but they’re just not giving their body time to adjust.
What helps? Eat smaller meals. Avoid greasy, fried, or sugary foods. Stay hydrated. Some doctors prescribe low-dose ondansetron (Zofran) for the first few weeks to manage nausea. One Reddit user wrote, “Weeks 3 to 8 were brutal. I almost quit. Then I slowed the dose increase and switched to bland meals-everything got better.”
There are also rare but serious risks. Animal studies showed thyroid tumors with high doses. The FDA added a black box warning, but no clear link has been proven in humans. Still, if you or a family member has a history of medullary thyroid cancer or multiple endocrine neoplasia, you shouldn’t take these drugs. Pregnant women are also advised to avoid them because safety data is limited.
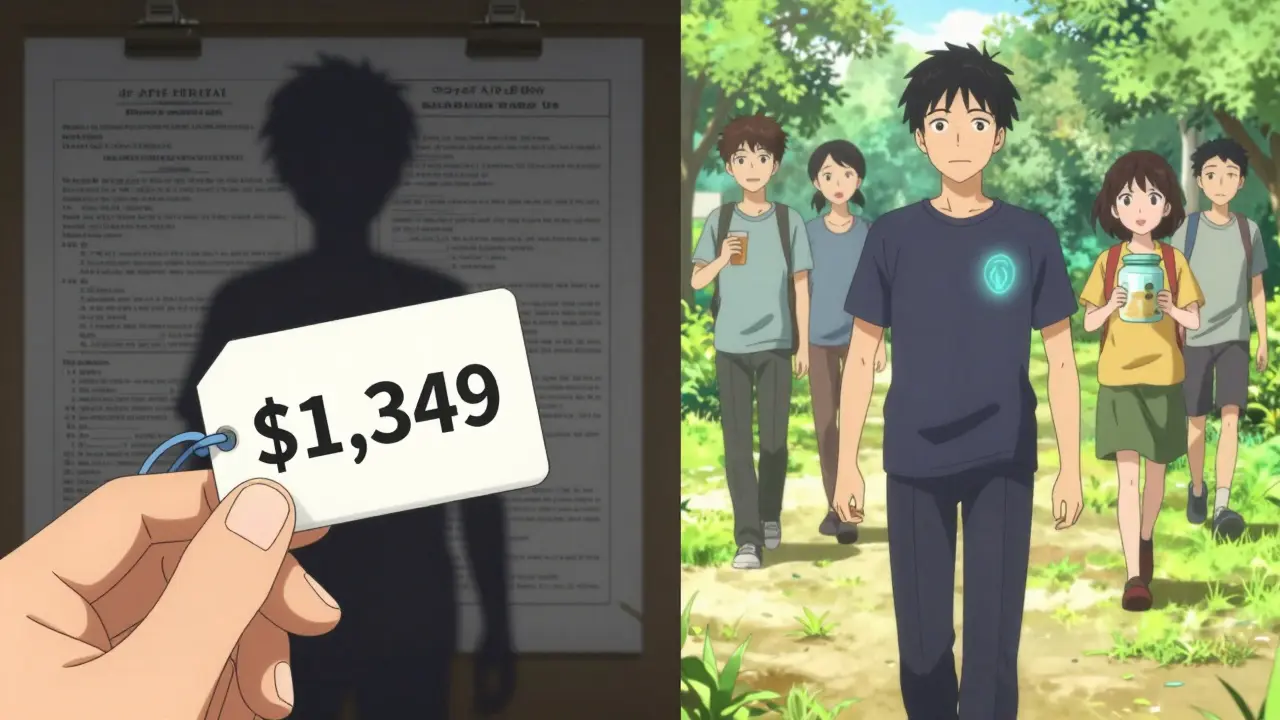
Cost and Insurance: The Biggest Hurdle
Wegovy costs about $1,349 a month without insurance. Ozempic, the same drug but approved for diabetes, is cheaper at $936. But insurance rarely covers Wegovy for weight loss. As of 2023, only 37% of private insurance plans in the U.S. cover it for obesity, even if your BMI is over 30. That’s a problem-because 78% of users are women, and many are middle-income earners who can’t afford $16,000 a year.
Compare that to older weight loss pills like phentermine, which can cost under $20 a month. Orlistat runs about $100. But those drugs don’t deliver the same results. The cost difference is stark-and it’s creating a two-tier system. People who can pay get life-changing results. Others are left behind.
Some manufacturers offer savings cards. Novo Nordisk has a program that can bring Wegovy down to $25 a month for eligible patients. But these programs have limits. And even with discounts, many still can’t access them because their doctors won’t prescribe them without insurance approval.
What Happens When You Stop?
This is the part no one talks about enough. If you stop taking the drug, you’ll likely regain most of the weight. In the STEP 4 trial, people who stopped Wegovy after a year regained 60% of their lost weight within a year. That’s not failure-it’s biology. These drugs don’t cure obesity. They manage it, like blood pressure or cholesterol meds.
That’s why experts say they should be used long-term. Dr. Louis Aronne from Weill Cornell says, “We’re treating a chronic disease. You don’t stop taking insulin after your blood sugar normalizes. You don’t stop taking statins after your cholesterol drops. Why stop GLP-1 agonists?”
But that means lifelong commitment-and cost. For many, that’s not sustainable. Some try to wean off slowly, but there’s no proven protocol. The best strategy? Combine the drug with lifestyle changes: regular movement, protein-rich meals, mindful eating. That way, even if you regain some weight, you won’t go back to square one.
How It Compares to Other Weight Loss Drugs
| Medication | Weight Loss (Average) | Dosing | Cost (Monthly, US) | Key Side Effects |
|---|---|---|---|---|
| Wegovy (semaglutide) | 15.8% | Weekly injection | $1,349 | Nausea, vomiting, diarrhea |
| Zepbound (tirzepatide) | 20.9% | Weekly injection | $1,350+ (est.) | Nausea, diarrhea, fatigue |
| Saxenda (liraglutide) | 6.4% | Daily injection | $1,300 | Nausea, constipation |
| Qsymia (phentermine-topiramate) | 7-10% | Daily pill | $150-200 | Cognitive fog, dry mouth, birth defects |
| Xenical (orlistat) | 5-10% | Daily pill | $100 | Oily stools, frequent bowel movements |
GLP-1 agonists are the most effective-but they’re also the most expensive and require injections. If cost or needles are deal-breakers, oral options like phentermine-topiramate might be considered. But they come with their own risks: brain fog, mood changes, and serious harm to unborn babies. For now, GLP-1 agonists remain the gold standard for people who need major weight loss and can manage the side effects.
Who Should Consider These Drugs?
The Endocrine Society recommends GLP-1 agonists for adults with a BMI of 30 or higher, or 27 or higher with at least one weight-related condition like high blood pressure, sleep apnea, or prediabetes. They’re not for people who just want to lose a few pounds. They’re for those with obesity as a medical condition.
They’re also not for everyone. If you have a history of pancreatitis, gallbladder disease, or severe GI disorders, talk to your doctor. If you’re pregnant or planning to be, avoid them. And if you’re not ready for weekly injections or can’t afford the cost, there are other options.
But for those who qualify and are willing to stick with it? The benefits are profound. One user on Drugs.com wrote: “I used to eat dinner standing up because I was too tired to sit. After three months on Wegovy, I cooked meals again. I didn’t just lose weight-I got my life back.”
Can GLP-1 agonists help me lose weight without dieting?
No. These drugs reduce appetite, but they don’t replace healthy habits. People who combine them with modest calorie reduction (500 calories less per day) and regular movement lose more and keep it off longer. Eating high-protein, low-fat meals also helps reduce nausea and supports muscle retention during weight loss.
How long does it take to see results?
Most people notice reduced hunger within the first week. Weight loss typically starts after 4 to 8 weeks. The biggest losses happen between months 4 and 12. By 68 weeks, most users reach their maximum weight loss. Patience is key-this isn’t a 30-day challenge.
Is Wegovy the same as Ozempic?
Yes, they’re the same drug-semaglutide. Wegovy is approved for weight loss at 2.4 mg weekly. Ozempic is approved for type 2 diabetes at 0.5 mg or 1 mg weekly. Some people use Ozempic off-label for weight loss because it’s cheaper, but that’s not its intended use and can worsen shortages for people with diabetes.
Are there oral versions of GLP-1 agonists?
Rybelsus is an oral form of semaglutide approved for type 2 diabetes, but not yet for weight loss. Pfizer and other companies are testing oral GLP-1 drugs in phase 3 trials, with results expected in 2024-2025. If approved, these could be game-changers for people who can’t stand injections.
Can I take GLP-1 agonists if I have kidney or liver problems?
Yes, but with caution. GLP-1 agonists are generally safe for mild to moderate kidney or liver disease. But severe impairment may require dose adjustments or avoidance. Always tell your doctor about all your health conditions before starting.
What’s Next for GLP-1 Drugs?
The market is exploding. By 2030, sales could hit $100 billion a year. Novo Nordisk and Eli Lilly are racing to develop next-gen versions: longer-acting injections, combination therapies, and oral pills. More insurance plans are starting to cover them-but slowly. Supply shortages are still a problem; Novo Nordisk had 18-month backorders for Wegovy in late 2023.
More than 22 ongoing clinical trials are studying these drugs for heart failure, non-alcoholic fatty liver disease, and even Alzheimer’s. Early results are promising. This isn’t just a weight loss drug anymore. It’s becoming a cornerstone of metabolic health.
But access remains unequal. In places like South Africa, where healthcare is fragmented and costs are high, these drugs are out of reach for most. Even in the U.S., only those with good insurance or deep pockets can consistently use them.
For now, GLP-1 agonists are the most powerful tool we have for treating obesity. But they’re not a cure. They’re a bridge-between old ways of thinking about weight and a future where chronic disease is managed, not blamed. The goal isn’t just to lose weight. It’s to live better, longer, and healthier. And that’s worth understanding-no matter the cost or the side effects.

Katie Mccreary
January 28, 2026 AT 10:02Lance Long
January 30, 2026 AT 09:32My doctor said I’m a candidate. I’m not doing it for looks. I’m doing it so I can play with my niece without getting winded. So I can sleep through the night. So I don’t have to dread the scale anymore. I’m scared. But I’m doing it.
Timothy Davis
January 30, 2026 AT 17:33fiona vaz
January 31, 2026 AT 22:31Sue Latham
February 2, 2026 AT 02:09John Rose
February 3, 2026 AT 16:00