How to Check Medication Strength and Quantity on Prescription Labels
 Dec, 27 2025
Dec, 27 2025
Every time you pick up a prescription, you’re holding your safety in your hands. A single mistake in reading the medication strength-like confusing 0.25 mg with 25 mg-can lead to a dangerous overdose. That’s why checking the label isn’t optional. It’s your last line of defense. And you don’t need to be a pharmacist to do it right.
Where to Find Medication Strength on the Label
The strength tells you how much active drug is in each dose. It’s always printed right next to the drug name. Look for numbers followed by units like mg (milligrams), mcg (micrograms), or IU (international units). For example:
- AMOXICILLIN 500 MG
- HYDROCORTISONE 1% CREAM
- INSULIN GLARGINE 100 UNITS/mL
For tablets or capsules, the number is the amount per pill. For liquids, you’ll see a ratio like 5 mg/5 mL. That means every 5 milliliters of liquid contains 5 milligrams of medicine. Don’t assume the total bottle volume is the dose-always check the ratio.
Pharmacies like CVS and Walgreens place strength information differently. CVS puts it directly under the drug name. Walgreens often puts it in parentheses after the name. But no matter the layout, the strength is always close by-usually within half an inch.
Understanding Quantity: What’s Actually in the Bottle
Quantity is how much the pharmacy gave you in total. It’s not the same as how much you take each time. Look for units like:
- 30 tablets
- 120 mL
- 30 grams
If you’re supposed to take one pill a day and you got 30 tablets, that’s a 30-day supply. If you got 120 mL of liquid and you take 5 mL twice a day, that’s 10 doses per day-so 12 days’ worth. Mismatched quantity and daily dose is a red flag. Always double-check your prescription instructions against what’s on the label.
Why Units Matter: mg vs. mcg Can Be Deadly
Milligrams (mg) and micrograms (mcg) look similar. But 1 mg equals 1,000 mcg. A mistake here isn’t just an error-it’s life-threatening. That’s why FDA rules require full words, not abbreviations. You’ll never see “U” for units or “mcg” written as “μg.” If you see “U,” stop. That’s outdated and dangerous.
One of the most common fatal errors is misreading a decimal point. 0.5 mg looks like 5 mg if the zero is small. That’s why many pharmacies now use bold fonts or larger text for strength. Still, you can’t rely on that alone. Use your phone’s magnifier app if the text is too small. Tap and hold on the label, then use the zoom feature. It’s free, fast, and saves lives.
Check for Liquid Medications: Concentration Is Key
Liquid meds are the most dangerous when it comes to strength errors. A 2022 study by the American Society of Health-System Pharmacists found that 32.4% of medication errors happen with liquids because caregivers mix up concentration ratios.
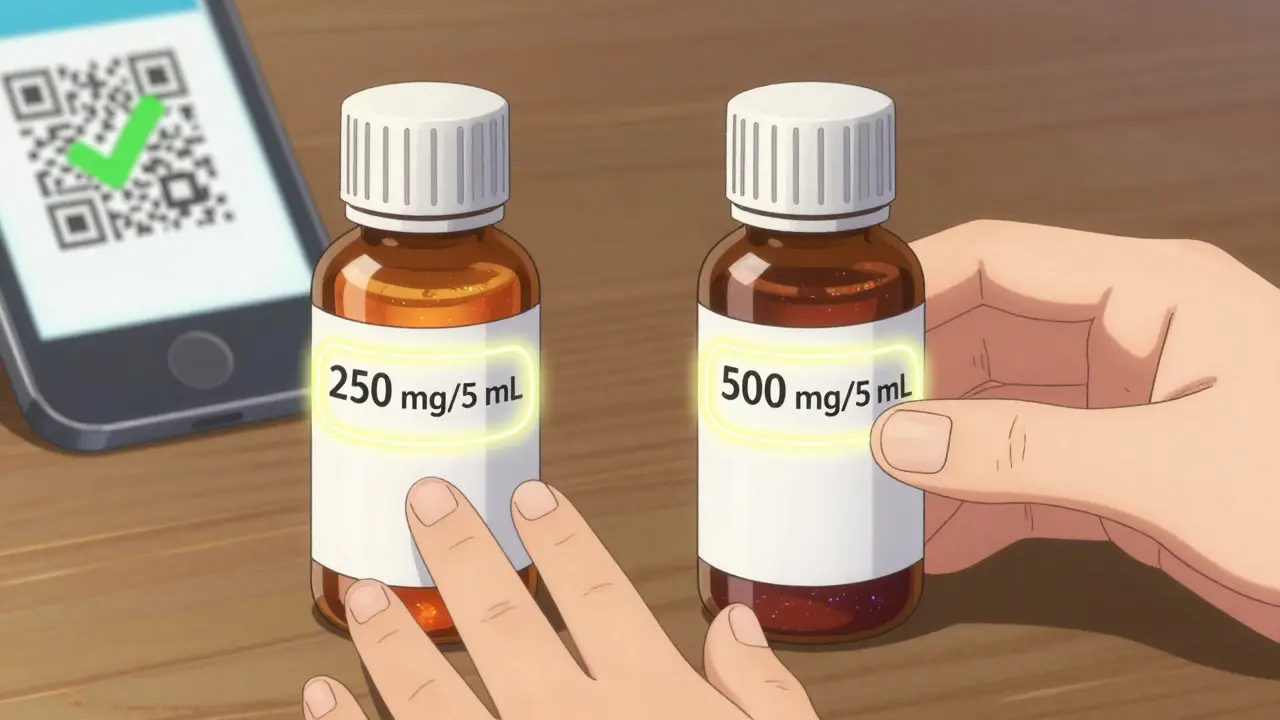
Example: Your child’s antibiotic says 250 mg/5 mL. You think, “I need to give 10 mL.” But if the label says 500 mg/5 mL instead, you’re giving double the dose. Always ask: “Is this the same concentration as last time?” If the pill looked different last month, or the liquid color changed, that’s a clue. Don’t assume the pharmacy didn’t make a mistake.
Compare With Your Prescription
When your doctor writes a prescription, they specify the drug, strength, and quantity. That’s your baseline. When you get the bottle, compare:
- Drug name: Is it spelled right? Is it the brand or generic you expected?
- Strength: Does it match what the doctor wrote?
- Quantity: Did they give you the number of days you need?
Many people skip this step because they trust the pharmacy. But a 2023 study showed that 22.3% of medication errors reported to the Patient Safety Network were due to strength mismatches. One Reddit user caught their child’s amoxicillin was labeled 500 mg/5 mL instead of 250 mg/5 mL-almost doubling the dose. They caught it before giving it. That’s the power of checking.
Watch Out for Compounded Medications
If your medicine was made by a compounding pharmacy (custom-mixed for you), the label might be less clear. The FDA found that only 63.2% of compounded meds had clearly printed strength info. These labels often lack standardized formatting. If you’re unsure, call the pharmacy. Ask: “Can you confirm the strength per dose?” Don’t guess.
Use Tools That Help
Most big pharmacies now offer digital tools to verify your meds:
- QR codes on labels link to FDA-approved Medication Guides with dosage charts.
- Mobile apps let you scan the barcode to compare label info with your electronic prescription.
- Some stores offer high-contrast labels for low vision-just ask.
Over 67% of pharmacies now use digital verification systems. That means your phone can check the label against the pharmacy’s records in seconds. But even with tech, your eyes still matter. Use the app as a second check-not your only one.
Special Cases: Elderly, Low Literacy, and Polypharmacy
If you’re over 65, taking 4 or more meds, or have trouble reading small print, you’re at higher risk. A 2023 study found that 37.8% of strength errors happen in seniors. Only 43.6% of people with low health literacy understand label strength without help.
Here’s what works:
- Ask the pharmacist to write the daily dose on the bottle with a marker.
- Use a pill organizer with clear labels.
- Bring a family member or friend to pick up prescriptions.
- Request large-print labels-89% of chain pharmacies offer them.
Don’t feel embarrassed to ask for help. Pharmacists are trained to explain labels. That’s part of their job.
What to Do If Something Looks Wrong
If the strength, quantity, or drug name doesn’t match what your doctor prescribed:
- Don’t take it.
- Call the pharmacy immediately. Ask: “Can you verify this prescription with my doctor?”
- If they say it’s correct but you’re still unsure, call your doctor’s office.
- If you suspect a serious error, report it to the FDA’s MedWatch program.
One user on Mayo Clinic Connect shared: “My blood pressure med was filled as 10 mg instead of 2.5 mg. The pill looked different, but I didn’t know why until I checked the label. I could’ve had a stroke.”
You don’t need to be an expert. You just need to be careful.
Final Checklist Before Taking Any Medication
Before you swallow, take 30 seconds. Ask yourself:
- Is the drug name spelled correctly?
- Is the strength written clearly? (mg, mcg, IU, %)
- For liquids: Does the concentration match what I was told?
- Is the total quantity right for how long I’m supposed to take it?
- Does this match my last prescription? (Color, shape, size)
If even one answer feels off-stop. Call someone. Ask again.
Medication errors kill 7,000 to 9,000 people in the U.S. every year. Most of them are preventable. You’re not being paranoid. You’re being smart.
What does medication strength mean on a prescription label?
Medication strength tells you how much active drug is in each dose. For pills, it’s the amount per tablet or capsule (like 500 mg). For liquids, it’s a ratio like 5 mg/5 mL, meaning 5 milligrams of medicine in every 5 milliliters of liquid. Always check this number-it’s the most important safety detail on the label.
How do I know if the quantity on my prescription is correct?
The quantity is the total amount dispensed-like 30 tablets or 120 mL. To check if it’s right, multiply your daily dose by the number of days you’re supposed to take it. For example, if you take 2 pills a day for 14 days, you should get 28 pills. If you got 60, that’s too many. Call the pharmacy to confirm.
Can I trust the pharmacy to get the strength right?
Most pharmacies follow strict rules, but mistakes still happen. In 2022, over 1.3 million medication errors occurred in the U.S., and nearly 22% were due to incorrect strength. Pharmacies are human-run. Your job is to be the final check. Never assume it’s right-always verify yourself.
What should I do if the label looks different from last time?
If the pill looks different-color, shape, size-or the liquid seems thicker or thinner, don’t take it. Ask the pharmacist: “Is this the same medication I got before?” Sometimes, pharmacies switch to a generic version, which is safe-but you should still confirm the strength matches. Never ignore a visual change.
Are there tools to help me read small print on labels?
Yes. Use your smartphone’s magnifier app-tap and hold on the label to zoom in. Many pharmacies also offer large-print labels for free if you ask. Some even have QR codes you can scan to see a larger version of the label on your phone. Don’t strain your eyes. Use the tools available.
What’s the most dangerous mistake people make with prescription labels?
The most dangerous mistake is misreading decimal points-like reading 0.5 mg as 5 mg. That’s a 10-fold overdose. Another big risk is confusing total quantity with daily dose. For example, thinking a 30 mL bottle means you take 30 mL each day, when it’s actually 5 mL per dose. Always read the label slowly. Write it down if you need to.

Nicole Beasley
December 28, 2025 AT 14:16OMG I just realized I’ve been squinting at my insulin label like it’s a cryptic emoji 😅 Thank you for the magnifier app tip-I just zoomed in and saw I was reading 100 units as 10. I almost took a whole extra vial. 🙌
James Hilton
December 29, 2025 AT 06:07Pharmacies are just glorified fast food joints with white coats. You think they care if you live or die? Nah. They’re counting your pills like they’re M&Ms. Check your label-or don’t. Your funeral will have better signage.
Mimi Bos
December 30, 2025 AT 00:22i just checked my amoxicillin and it said 500mg but i swear last time it was 250… i think i misread it but now im paranoid lol. also the bottle looks different?? did they change the recipe??
Payton Daily
December 31, 2025 AT 01:40Let me tell you something about power. The real power isn’t in the pill. It’s in the silence between the doctor’s words and the pharmacist’s haste. We live in a world where your life is printed in 8-point font on a sticky label while someone behind a counter scrolls TikTok. You think this is medicine? No. It’s a gamble with your DNA. And you’re the only one who can call the bluff.
They say ‘trust your instincts.’ But your instincts were trained by a system that wants you passive. So now you’re awake. Good. Now don’t go back to sleep.
Kelsey Youmans
January 1, 2026 AT 03:13Thank you for this comprehensive and meticulously structured guide. The emphasis on patient agency in medication safety is both commendable and long overdue. I have shared this with my elderly patients at the clinic, and several have expressed gratitude for the clarity. The inclusion of practical tools-such as the magnifier app and large-print label requests-is particularly thoughtful and accessible.
Gran Badshah
January 2, 2026 AT 05:26bro why are you even reading the label? just take it. i live in india and we dont even know what's in our pills. i take 3 different meds and i just crush them in chai. works fine. you americans overthink everything.
Ellen-Cathryn Nash
January 2, 2026 AT 21:47People who don’t check their prescriptions are just one bad pharmacy away from becoming a cautionary tale on a billboard. You think your life is worth less than a $12 co-pay? You’re not just risking yourself-you’re disrespecting every nurse who’s ever cleaned up the mess you made. Check the damn label. Or don’t. But don’t cry when your kidneys give up.
Samantha Hobbs
January 4, 2026 AT 05:43Wait so if I use my phone to zoom in… does that mean I’m not supposed to trust my glasses? 😭 I’ve had these for 7 years and they’re my best friend. Are you saying they’re useless now??
sonam gupta
January 4, 2026 AT 10:36usa thinks it owns medicine now? we in india use herbal and still live till 90. you people are addicted to pills and labels. just eat turmeric and chill
Julius Hader
January 6, 2026 AT 07:19My grandma reads her labels out loud every time she takes something. Says it helps her remember. I thought it was weird… until I saw her catch a wrong dose last month. Now I do it too. Just say the name and the number. Weird? Maybe. Safe? Absolutely.
Vu L
January 6, 2026 AT 17:01Yeah right. Like the pharmacy doesn’t know what they’re doing. This whole post is just fear-mongering to sell you more apps. I’ve been taking the same pill for 12 years. It’s a blue oval. It looks the same. I’m fine.
Sydney Lee
January 7, 2026 AT 23:47It is not merely a label. It is a covenant between the scientific method and the vulnerable human. To neglect its scrutiny is to commit epistemic negligence-a betrayal of Enlightenment values, rendered in Helvetica 8pt. The pharmacy is not a sanctuary. It is a labyrinth of bureaucratic entropy. Only the vigilant survive. And you, dear reader, are either one of them… or a statistic in waiting.
oluwarotimi w alaka
January 9, 2026 AT 22:45you think america is safe? they put poison in pills and call it medicine. i heard the FDA is controlled by big pharma. your label? it’s a lie. they want you sick so you keep buying. check your water. check your air. check your soul. this is all part of the plan.