How to Tell a Side Effect from a True Drug Allergy
 Dec, 15 2025
Dec, 15 2025
Many people say they’re allergic to penicillin-or ibuprofen, or sulfa drugs-because they got sick after taking it. But here’s the truth: most of those reactions aren’t allergies at all. In fact, only 5 to 10% of people who think they have a drug allergy actually do. The rest? They’re experiencing side effects. And that mix-up isn’t just confusing-it’s dangerous.
What’s the real difference?
A side effect is what happens when a drug does something it’s supposed to do… just not where you want it to. Take antibiotics like amoxicillin. They kill bacteria. But they also mess with the good bacteria in your gut. That’s why nausea, diarrhea, or stomach cramps happen. These aren’t surprises-they’re expected. They’re listed right on the bottle. And if you stop taking the drug, they usually go away. A true drug allergy? That’s your immune system going haywire. It sees the drug as an invader-like a virus or pollen-and attacks it. That triggers real inflammation. You might get hives, swelling, trouble breathing, or even go into anaphylaxis. These aren’t side effects. They’re immune responses. And they get worse every time you’re exposed again.Timing tells the story
When did the reaction happen? That’s your first clue. If you took a pill and within minutes to an hour, your face swelled up, your throat closed, or you broke out in itchy red bumps? That’s an allergic reaction. IgE antibodies kicked in fast. This is the kind that needs an EpiPen and a trip to the ER. But if you started a new medication and three days later, you got a rash? Or two weeks later, your skin started peeling? That’s a delayed reaction-and it’s still an allergy. These are T-cell driven. They’re slower, but just as serious. Conditions like DRESS or Stevens-Johnson Syndrome fall here. They don’t show up right away, but they can kill you if ignored. Now, if you got a headache after taking ibuprofen? Or felt dizzy after your blood pressure pill? That’s a side effect. It’s not your immune system. It’s just the drug doing its job too well-or in the wrong place.One system or many?
Side effects usually stick to one system. Nausea? That’s your stomach. Dizziness? Your inner ear or brain. Constipation? Your intestines. Allergies? They hit multiple systems at once. You get a rash and swollen lips and wheezing. That’s not coincidence. That’s your immune system going full alert. A 2023 analysis of 10,000 patient records found that 87% of true drug allergies involved at least two body systems. Only 22% of side effects did. Think of it like this: if your phone overheats because you’re playing a game for hours? That’s a side effect. If your phone suddenly catches fire because of a faulty battery? That’s an allergic reaction. One is predictable. The other is a system failure.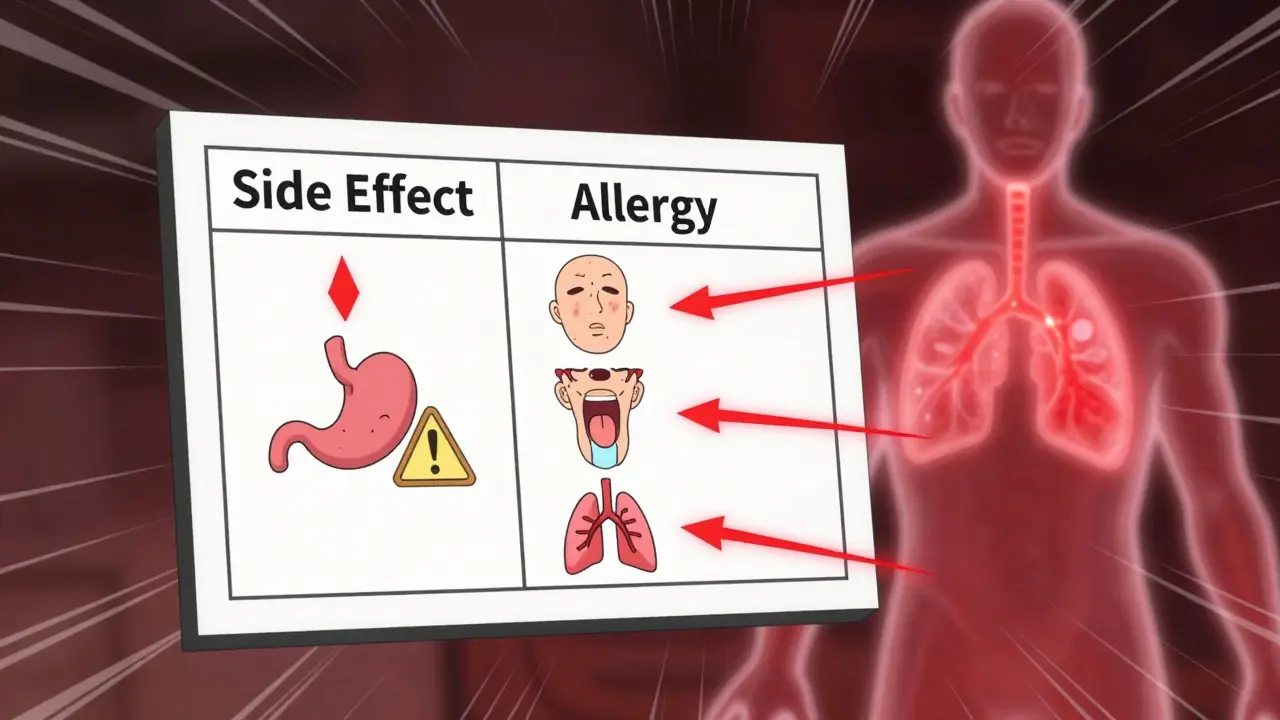
The penicillin myth
About 7% of Americans say they’re allergic to penicillin. But when tested properly, 90 to 95% of them aren’t. They had nausea, or a mild rash that faded on its own, or a headache-and labeled it an allergy. That’s a problem. Doctors then prescribe stronger, more expensive antibiotics. These drugs don’t just cost more. They’re worse for you. They kill off good bacteria. They raise your risk of C. diff infections. They contribute to antibiotic resistance. A 2022 JAMA Network Open study showed people with false penicillin allergies had 69% higher rates of C. diff and stayed in the hospital 30% longer. The FDA now requires drug labels to clearly separate side effects from allergies. But patients still mislabel. On Reddit’s r/Allergy, 63% of people who claimed a drug allergy described nausea or diarrhea. Only 22% described hives or swelling. That’s a massive gap between perception and reality.What to do if you think you’re allergic
Don’t just assume. Don’t avoid the drug forever. Get it checked. If you had a reaction years ago, ask your doctor about a referral to an allergist. They can do skin tests or blood tests (like the new Penicillin ImmunoCAP test) to see if your body actually makes IgE antibodies to the drug. These tests are 95% accurate for penicillin. If the reaction was mild-a rash that went away after stopping the drug-you might be a candidate for a supervised drug challenge. You take a tiny dose under medical watch. If nothing happens? You’re not allergic. You’re just someone who got a side effect. And if you’ve been avoiding a drug for years because of a vague memory of feeling sick? You’re probably not helping yourself. You’re limiting your treatment options. A 2023 study at Kaiser Permanente found that 78% of patients who thought they had drug allergies could safely take the drug after proper testing.
When to panic
Not every reaction needs an ambulance. But some do. Call 911 or go to the ER immediately if you have:- Hives or swelling of the face, lips, or tongue
- Wheezing or trouble breathing
- Feeling faint or your heart racing
- Severe dizziness or loss of consciousness
What’s changing in medicine
Hospitals are catching on. In 2020, only 15% of U.S. hospitals had formal programs to re-evaluate drug allergies. By 2023, that number jumped to 42%. Mayo Clinic’s program successfully de-labeled 92% of low-risk patients. That means people who thought they couldn’t take penicillin? Now they can. And their care got better. Electronic health records now have checkboxes to mark whether a reaction was an allergy or a side effect. Pharmacists are trained to ask: “Did you break out in hives? Or just feel sick to your stomach?” That small question changes everything. The American College of Allergy, Asthma, and Immunology is pushing for new terminology too. By 2024, doctors will start using “allergy” for immune reactions, “intolerance” for non-immune side effects, and “side effect” for expected, dose-related reactions. No more mixing terms.Bottom line
You’re not allergic just because a drug made you feel bad. Allergies mean your immune system attacked it. Side effects mean the drug did something it wasn’t meant to do-like upset your stomach or make you dizzy. If you’ve ever said, “I’m allergic to this,” ask yourself: Did I get hives? Swelling? Trouble breathing? Or did I just feel queasy? If it’s the latter? You’re probably not allergic. You’re just one of the millions who got a side effect-and you’ve been avoiding a safe, effective drug for years. Get it checked. Don’t let a mislabelled reaction limit your health.Can a side effect turn into a drug allergy?
No. A side effect is a direct result of the drug’s chemistry and doesn’t involve the immune system. You can’t “develop” an allergy from a side effect. But you can mistake a side effect for an allergy-and then, if you take the drug again, you might have a true allergic reaction because your immune system was never involved the first time. The confusion comes from labeling, not biology.
Is a rash always a sign of a drug allergy?
Not always. Many drugs cause rashes as side effects-especially antibiotics. A non-itchy, flat rash that appears after several days is often a benign side effect. A true allergic rash is usually raised, red, itchy (hives), and shows up quickly-within minutes to hours. If the rash is accompanied by swelling, fever, or blistering, it’s likely immune-mediated and needs urgent care.
Can I outgrow a drug allergy?
Yes, especially with penicillin. Studies show that 80% of people who had a penicillin allergy in childhood lose it within 10 years. The immune system can forget the drug. That’s why retesting is so important-even if you had a reaction decades ago, you might be able to take the drug safely now.
What if I had a reaction but didn’t see a doctor at the time?
You’re not alone. Most people don’t. But that’s why documentation matters. If you remember symptoms-like swelling, trouble breathing, or hives-you should still get tested. If you only remember feeling sick or getting a rash, talk to an allergist. They’ll ask detailed questions and may recommend a challenge test. Never assume. Always verify.
Are there tests to confirm a drug allergy?
Yes. For immediate reactions (like anaphylaxis or hives), skin tests and blood tests for IgE antibodies are highly accurate-for penicillin, they’re 95% reliable. For delayed reactions, patch tests or lymphocyte tests are used. These aren’t available everywhere, but allergists know where to send you. If you’ve been avoiding a drug for years, testing is the only way to get your options back.
Why do doctors still prescribe stronger antibiotics if I say I’m allergic to penicillin?
Because they don’t know your reaction was a side effect. If you just say “I’m allergic,” they assume it’s immune-mediated and avoid all penicillin-type drugs. But if you can prove it wasn’t, they can switch you back to safer, cheaper, more effective options. That’s why accurate labeling saves lives-and money.
Can I try the drug again at home if I think I’m not allergic?
Never. Even if you think your reaction was mild, trying the drug again without medical supervision is risky. Allergic reactions can get worse with each exposure. Always get tested by a specialist first. A supervised challenge in a clinic is safe. Doing it yourself is not.

Dave Alponvyr
December 15, 2025 AT 14:36So let me get this straight-I took amoxicillin once and got a stomachache, so now I’m ‘allergic’? Yeah, I’ve been saying that for 10 years. Turns out I just have a weak gut and a bad memory. Thanks for the wake-up call.
Ron Williams
December 17, 2025 AT 08:40My mom used to say she was allergic to penicillin because she got a rash after taking it as a kid. She never got tested. Last year, she finally did-and turned out she’s fine. Now she’s on the cheapest antibiotic in the world and her bills dropped by half. Weird how we just accept nonsense as truth.
Aditya Kumar
December 18, 2025 AT 02:55Whatever. I don’t care. Just give me the pill and shut up.
Billy Poling
December 19, 2025 AT 22:05It is of paramount importance to recognize that the conflation of pharmacological side effects with immunologically mediated hypersensitivity reactions constitutes a critical public health concern, as it leads to suboptimal therapeutic decision-making, increased healthcare expenditures, and the inadvertent promotion of antimicrobial resistance through the unnecessary use of broad-spectrum alternatives. The data presented here, while statistically compelling, lacks sufficient longitudinal cohort analysis to fully account for confounding variables such as comorbidities, polypharmacy, and recall bias in patient self-reporting.
Randolph Rickman
December 21, 2025 AT 11:22This is exactly why we need better patient education-and why doctors should be required to ask, ‘Did you break out in hives or just feel sick?’ every single time someone says they’re allergic. I work in a clinic and I’ve seen people avoid life-saving meds for decades because they got a headache once. You’re not allergic because you felt dizzy. You’re just human. Get tested. You’ll thank yourself later.
Tiffany Machelski
December 22, 2025 AT 09:39i had a rash after sulfa and thought i was allergic… but it was just a sun reaction and i took it in the summer lol. i never told anyone. now i feel dumb.
Souhardya Paul
December 22, 2025 AT 18:19One thing I’ve noticed-people don’t realize how many antibiotics are just variations of penicillin. If you say you’re allergic, you’re often denied amoxicillin, ampicillin, even some cephalosporins. And yet, most of those cross-reactions are super rare. I had a patient who avoided all beta-lactams for 20 years because of a stomachache at age 8. Turned out she could’ve taken amoxicillin the whole time. Allergist confirmed it. She cried. We all did.
Josias Ariel Mahlangu
December 24, 2025 AT 01:36People today are too lazy to distinguish between discomfort and danger. A rash is a rash. If you can’t tell the difference between feeling sick and nearly dying, maybe you shouldn’t be self-diagnosing medical conditions at all. This isn’t a TikTok trend. Lives are at stake.