IgA Nephropathy: Prognosis and Current Therapies in 2025
 Dec, 3 2025
Dec, 3 2025
When your kidneys start failing silently, you don’t always feel it. For many people with IgA Nephropathy, the first sign isn’t pain or fatigue-it’s blood in the urine after a cold or sore throat. This autoimmune kidney disease, first identified in 1968, is now the most common cause of primary glomerulonephritis worldwide. And in 2025, how we treat it has changed completely.
What IgA Nephropathy Actually Does to Your Kidneys
IgA Nephropathy, also called Berger’s disease, happens when your immune system makes too much of a specific antibody called IgA. Instead of fighting infections properly, this antibody clumps together and gets stuck in the filtering units of your kidneys-the glomeruli. These clumps trigger inflammation. Over time, that inflammation scars the filters. Once scarred, they can’t clean your blood anymore.
It often shows up in teens and young adults. Some people notice dark, cola-colored urine after an infection. Others never have symptoms until a routine blood test shows high protein or low kidney function. About 30-40% of cases are found this way-by accident. But here’s the scary part: up to half of those with persistent proteinuria will lose kidney function within 10 to 20 years. That means dialysis or a transplant could be coming.
The Big Shift in Treatment: KDIGO 2025 Guidelines
Before 2025, doctors treated IgA Nephropathy in steps. First, they’d give blood pressure meds-usually ACE inhibitors or ARBs-to reduce protein leakage. Wait three months. If protein didn’t drop enough, then they’d add steroids or other immune drugs. That approach let the disease keep damaging kidneys while waiting.
The KDIGO 2025 guidelines changed all that. Now, if you’re at high risk, you start multiple treatments at once. No more waiting. The goal isn’t just to slow things down-it’s to stop them before they get worse.
The new strategy has two parts. One targets the root cause: the bad IgA and the immune complexes that wreck your kidneys. The other targets the body’s response to the damage: high blood pressure, protein loss, and kidney stress. Both are treated together from day one.
What Works Now: The Four Key Therapies
Four main treatments are now standard for high-risk patients:
- Nefecon - This is the first drug approved specifically for IgA Nephropathy. It’s a targeted-release steroid that acts in the gut, where IgA is made. Unlike regular steroids that flood your whole body, Nefecon reduces side effects like weight gain, mood swings, and bone loss. In patient surveys, 72% reported fewer side effects compared to traditional steroids.
- Systemic glucocorticoids - Still used, especially where Nefecon isn’t available. But they come with risks: diabetes, infections, cataracts. Doctors now use lower doses for shorter times, and only for those with high proteinuria and fast-progressing disease.
- RAS inhibitors + SGLT2 inhibitors - ACE or ARB drugs (like losartan or lisinopril) lower blood pressure and reduce protein in urine. Now, SGLT2 inhibitors (like dapagliflozin) are added. Originally for diabetes, they’ve proven to protect kidneys even in non-diabetics. They cut proteinuria and slow decline in kidney function.
- DEARA drugs (like sparsentan) - A newer class that blocks two systems that cause kidney damage: endothelin and angiotensin. Approved in Europe in 2024 and under review in the U.S., it’s especially helpful for patients with heavy proteinuria who can’t tolerate steroids.
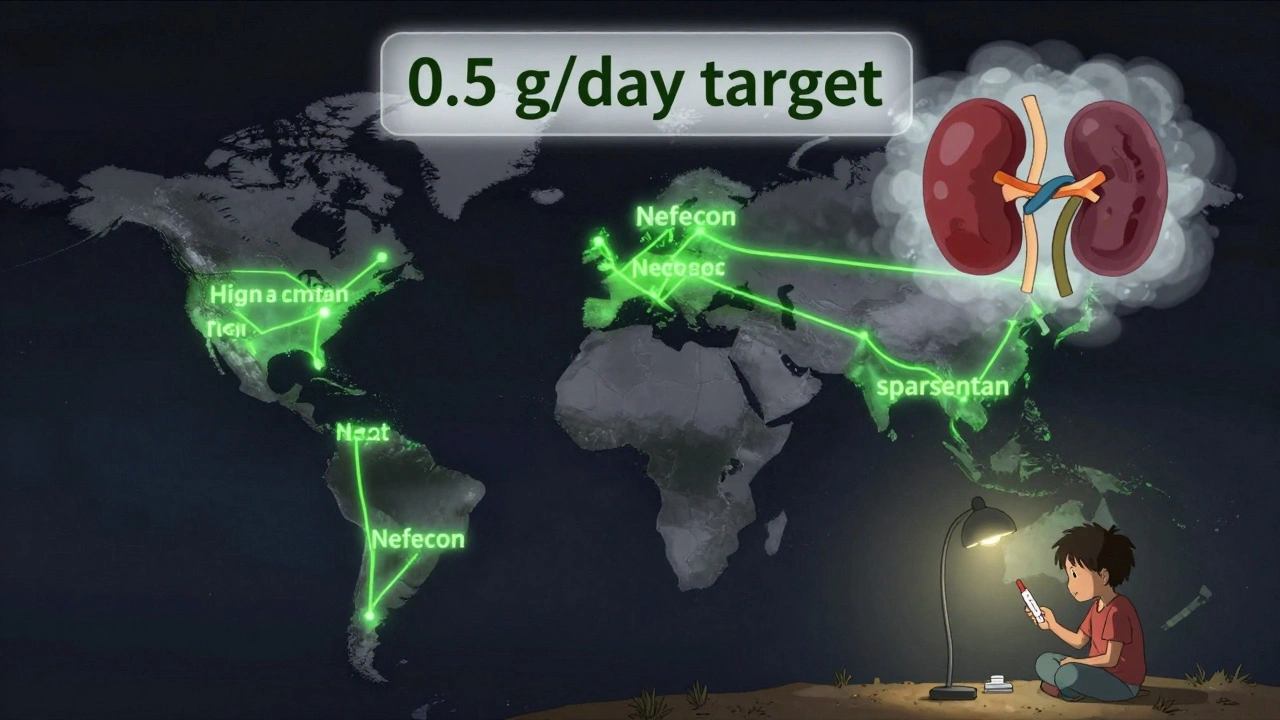
Proteinuria is now the main measure of success. The goal? Less than 0.5 grams per day. That’s half of what was considered acceptable just a few years ago. Studies show even patients with proteinuria between 0.44 and 0.88 g/g still had a 30% chance of kidney failure within 10 years. So lowering it further isn’t just a preference-it’s critical.

Regional Differences in Treatment
Not every treatment works the same everywhere. In Japan, removing the tonsils (tonsillectomy) is common. About 45% of eligible patients get it. The theory? Tonsils produce abnormal IgA. In China, mycophenolate mofetil and hydroxychloroquine are widely used. In Western countries, these aren’t standard-because the data doesn’t support them as strongly.
That’s a problem. A patient in South Africa or Nigeria might not have access to Nefecon, sparsentan, or even a nephrologist who knows how to use the new guidelines. Global access is the biggest gap. Only 22% of patients in low- and middle-income countries get guideline-recommended care. In high-income countries, it’s 85%.
The Cost Problem: Can You Afford to Live?
Nefecon costs $125,000 a year in the U.S. Sparsentan isn’t far behind. Insurance often denies coverage. Patients report spending months appealing denials. One Reddit user wrote: “I got approved after six letters, three phone calls, and a letter from my doctor. By then, my kidney function dropped 15%.”
Even if you get the drugs, managing them is hard. A 16-year-old on Nefecon, an SGLT2 inhibitor, an ARB, and a steroid has to take four pills at different times of day. One parent on Facebook said: “It’s overwhelming. He forgets, we panic, we double-check. It’s not just medicine-it’s a full-time job.”
What’s Next? Biomarkers and Personalized Treatment
Right now, doctors guess who will progress based on protein levels, blood pressure, and kidney biopsy results (MEST-C score). But that’s not enough. The field is racing toward biomarkers-blood or urine tests that tell you exactly which pathway is driving your disease.
Is it your gut? Your complement system? Your B-cells? If we can tell, we can pick the right drug: Nefecon for gut-driven IgA, complement blockers for inflammation-driven damage, APRIL inhibitors for B-cell overactivity.
Trials like TARGET-IgAN (expected to finish in 2027) are testing this. The hope? In five years, your treatment won’t be based on your age or protein level-but on your unique biology.
What Patients Really Care About
A survey of 1,200 IgA patients found that 83% said their top goal wasn’t just to live longer-it was to live well. They want to keep working, playing sports, traveling, being parents. They fear the side effects more than the disease sometimes.
That’s why the new guidelines stress minimizing treatment burden. No one wants to trade kidney failure for diabetes, depression, or a lifetime of steroid-related weight gain. The best therapy isn’t the one that lowers protein the most-it’s the one you can stick with without wrecking your life.
What You Should Do If You Have IgA Nephropathy
If you’ve been diagnosed:
- Ask for a full risk assessment using the KDIGO calculator-proteinuria, eGFR, blood pressure, and biopsy score.
- Don’t wait three months to start treatment if you’re high risk. Push for combination therapy now.
- Track your proteinuria monthly. Use a home dipstick test if available.
- Ask about SGLT2 inhibitors-even if you don’t have diabetes.
- If Nefecon or sparsentan are options, talk to your doctor about access, cost, and insurance appeals.
- Join a patient group. You’re not alone. The IgA Nephropathy Support Group on Facebook has over 8,500 members sharing tips, insurance hacks, and emotional support.
Progress isn’t guaranteed. But the tools to stop it are better than ever. The goal is simple: keep your kidneys working, keep your life intact, and avoid dialysis for as long as possible.
Can IgA Nephropathy be cured?
No, IgA Nephropathy cannot be cured yet. But it can be controlled. With the right combination of treatments-like Nefecon, SGLT2 inhibitors, and blood pressure control-many patients can stop or dramatically slow kidney damage. The goal isn’t to eliminate the disease, but to prevent it from leading to kidney failure.
How long does it take to see results from treatment?
Proteinuria usually starts to drop within 3 to 6 months of starting treatment. But it can take a year or more to reach the new target of under 0.5 g/day. Kidney function (eGFR) changes more slowly-it may stay stable for years if treatment works. Patience is key, but so is consistency. Missing doses or stopping meds early can undo progress.
Is Nefecon better than steroids?
For most patients, yes. Nefecon targets the source of bad IgA in the gut, so it doesn’t flood your whole body with steroids. That means fewer side effects: less weight gain, no high blood sugar, lower risk of infections. In surveys, patients report better quality of life on Nefecon. But it’s not for everyone. If you’re in a region where it’s not available or too expensive, steroids may still be the best option-used carefully and for the shortest time possible.
Should I get a tonsillectomy if I have IgA Nephropathy?
It depends on where you live and your doctor’s experience. In Japan, tonsillectomy is a standard part of treatment and has strong evidence there. But in the U.S. and Europe, studies haven’t shown clear benefit for most patients. Unless you’re in a region with proven success using this method, or you have frequent tonsil infections that trigger flare-ups, it’s not routinely recommended.
Can I still exercise or play sports with IgA Nephropathy?
Yes, unless your doctor says otherwise. Regular physical activity helps control blood pressure and reduces inflammation. Many patients continue running, swimming, or cycling. Avoid extreme endurance sports if your eGFR is below 30, and stay hydrated. But don’t stop moving-activity is part of protecting your kidneys.
What if I can’t afford the new treatments?
Start with what’s available and effective: ACE/ARB drugs and SGLT2 inhibitors. These are often cheaper and covered by insurance. Ask your doctor about patient assistance programs-pharmaceutical companies offer them for Nefecon and sparsentan. Nonprofits like the IgA Nephropathy Foundation help with appeals and cost navigation. Even without the newest drugs, strict blood pressure control and low proteinuria can still delay kidney failure for years.
Final Thoughts: Hope, But Not Complacency
The future for IgA Nephropathy is brighter than it’s ever been. We have drugs that target the disease at its source. We have data that tells us exactly how to measure success. We have patients speaking up, demanding better care.
But progress isn’t automatic. It needs doctors who know the guidelines. It needs insurers that cover the drugs. It needs systems that deliver care equally, no matter where you live.
If you have IgA Nephropathy, your job is simple: know your numbers, ask the right questions, and don’t accept waiting as the default. The tools to protect your kidneys are here. Now it’s about using them-before it’s too late.

Rebecca Braatz
December 4, 2025 AT 11:43Just had my third kidney biopsy this year and honestly? The new KDIGO guidelines are a game-changer. I started Nefecon + dapagliflozin six months ago and my proteinuria dropped from 2.1 to 0.38 g/day. No moonface, no insomnia, no crushing fatigue. I’m back hiking on weekends. If you’re high-risk and your doc is still waiting three months? Push back. Your kidneys don’t have time for bureaucracy.
zac grant
December 5, 2025 AT 00:41From a nephrology fellow: the real win here isn’t just the drugs-it’s the biomarker shift. We’re moving from MEST-C scores to IgA glycosylation patterns and APRIL levels. Soon we’ll be able to say ‘your disease is gut-driven’ or ‘complement-mediated’ and match therapy like precision oncology. TARGET-IgAN will be the tipping point. Just wish more community docs knew this was coming.
Augusta Barlow
December 5, 2025 AT 20:04Let’s be real-this whole ‘new treatment revolution’ is just Big Pharma repackaging old steroids under a fancy name. Nefecon? It’s still a steroid. Sparsentan? Just another angiotensin blocker with a $125K price tag. And don’t get me started on SGLT2 inhibitors being pushed to non-diabetics like they’re magic bullets. The FDA’s asleep at the wheel. This is all about profit margins, not patients. They’ve been doing this since the 90s-sell fear, then sell the cure. Meanwhile, real solutions like tonsillectomy get ignored because it’s not profitable. Wake up, people.
Joe Lam
December 7, 2025 AT 17:10Wow. So you’re telling me we’re finally treating IgA like a real disease and not just ‘watch and wait’? I mean, it’s about damn time. My nephrologist in Boston had me on ARBs for 18 months before even considering steroids. By then, I’d lost 20% eGFR. Now I’m on Nefecon and I swear I feel 10 years younger. If your doc isn’t following KDIGO 2025, fire them. This isn’t debate-it’s standard of care now.
Chase Brittingham
December 9, 2025 AT 09:56As someone who’s been on this journey for 7 years, I just want to say: you’re not alone. I was scared to death when I got diagnosed at 22. Thought I’d be on dialysis by 30. Now I’m 29, working full-time, and my proteinuria is under 0.4. It’s not perfect, but it’s manageable. The key? Consistency. Not perfection. Miss a dose? Don’t panic. Just get back on track. And if you’re struggling with cost or side effects-reach out. There are people who’ve been there.
Jake Deeds
December 10, 2025 AT 04:24It’s fascinating how the medical community suddenly discovered IgA Nephropathy only after the pharmaceutical industry had a viable profit model. The ‘new’ guidelines feel less like science and more like a marketing rollout for Nefecon. And don’t get me started on how they’re framing steroid avoidance as a moral victory-when in reality, it’s just a cost-cutting maneuver disguised as patient-centered care. The truth? We’re still guessing. We just have more expensive guesses now.
Ollie Newland
December 10, 2025 AT 11:12UK perspective: we’ve had access to Nefecon since late 2024 via the NHS, but only for those with eGFR >30 and proteinuria >1g/day. The real barrier isn’t the drug-it’s the lack of nephrologists who know how to interpret the new biomarkers. Most GP referrals still come in with ‘proteinuria’ and no MEST-C or urinary IgA glycosylation data. We’re years behind the US in implementation, even if we have the drugs.
Michael Feldstein
December 10, 2025 AT 20:18My 15-year-old son started Nefecon last month. We’re on day 22. He’s had zero side effects so far-no weight gain, no mood swings. He’s still playing soccer. The hardest part? The pill schedule. Four meds, three different times a day. We have alarms on his phone, a printed chart on the fridge, and a spreadsheet that tracks every dose. It’s exhausting. But if this keeps his kidneys alive? Worth it. Just wish insurance didn’t make us beg for every pill.
Bill Wolfe
December 11, 2025 AT 08:55Let me just say-this is the most irresponsible medical advice I’ve seen in years. You’re telling people to start four drugs at once? Without even knowing the underlying mechanism? That’s not medicine, that’s shotgun therapy. And now you’re telling parents to give their 16-year-old a steroid-like drug that’s been on the market for 18 months? Where’s the long-term safety data? This isn’t progress-it’s a clinical trial on real people with no informed consent. And the cost? $125k a year? Are you kidding me? This is medical apartheid.
Benjamin Sedler
December 12, 2025 AT 08:25So we’re now treating IgA like it’s cancer and throwing every drug we’ve got at it? Cool. But here’s the thing nobody’s saying: what if the real problem is our diet? Gluten? Sugar? Processed junk? I’ve seen patients go keto and their proteinuria drop faster than any drug. No one talks about it because Big Pharma doesn’t sell kale. But ask yourself-why does IgA spike after infections? Maybe it’s not just your immune system… maybe it’s your gut microbiome screaming for help. Just saying.
George Graham
December 12, 2025 AT 23:24I just want to say thank you to everyone who shared their stories here. I was diagnosed last month and felt so alone. Reading this made me feel seen. I’m scared, but also hopeful. I’m starting Nefecon next week. I don’t know if I’ll ever be ‘cured,’ but I’m learning how to live with this. And that’s enough for now.