Long-Term Opioid Use: How It Lowers Hormones and Hurts Sexual Function
 Jan, 26 2026
Jan, 26 2026
Opioid Hormone Impact Calculator
Hormone Risk Assessment
When you're on opioids for long-term pain, you might not think about your sex life or your energy levels. But if you've noticed a drop in desire, trouble getting or keeping an erection, missed periods, or just feeling flat - it's not just in your head. It's your hormones. And it's happening more often than doctors admit.
How Opioids Break Your Hormone System
Opioids don't just block pain signals. They also shut down your body's natural hormone production. The main target? The hypothalamic-pituitary-gonadal (HPG) axis - the system that tells your testes or ovaries to make testosterone and estrogen. When opioids like oxycodone, morphine, or fentanyl hit your brain, they slow down or stop the release of GnRH, the hormone that kicks off the whole chain. Without GnRH, your pituitary gland doesn't signal your gonads. Testosterone drops. Estrogen stays steady in women, but free testosterone still plummets. The result? A hormonal crash.
It doesn't take years. Studies show testosterone levels in men can fall 30-50% within just 30 days of starting daily opioid therapy. By six months, 63% of men on long-term opioids meet the clinical definition of hypogonadism: total testosterone below 300 ng/dL. For women, the pattern is different but just as real. Up to 87% of premenopausal women on chronic opioids develop menstrual problems - some stop getting periods entirely, others get irregular, unpredictable cycles. These aren't rare side effects. They're the rule.
Sexual Function Takes a Hit - For Everyone
If you're a man, the symptoms are often obvious: low libido, erectile dysfunction, reduced morning erections, and sometimes even breast tenderness. On Reddit’s r/ChronicPain, one user wrote: “After two years on oxycodone, my testosterone was 180. My doctor didn’t test it until I asked. Took six months to get help.” That story isn’t unusual. In surveys, 89% of men on long-term opioids report sexual issues. Many say their doctors dismissed it as “just aging” or “depression from pain.” But it’s not depression. It’s biology.
Women experience it differently. Low libido is the most common complaint - 78% of women in one survey reported it. But it’s not just about desire. Many report vaginal dryness, reduced arousal, and even pain during sex. The hormonal imbalance also links to mood changes - increased anxiety, irritability, and depression - which can make things worse. And because research on women has been minimal, most doctors don’t know what to look for. Only 2% of opioid trials include proper female sexual function assessments.
Not All Pain Meds Are the Same
Opioids are uniquely bad for your hormones. Compare them to other pain treatments:
- Opioids: 63% of men develop hypogonadism. 87% of women get menstrual issues.
- Gabapentinoids (like pregabalin): Only 12% of men show testosterone drops.
- NSAIDs (ibuprofen, naproxen): Minimal effect on hormones at standard doses.
- Acetaminophen: May cause mild sexual side effects in 5-15% of users - but nothing like opioids.
The American Pain Society stopped recommending opioids as first-line treatment for chronic non-cancer pain back in 2019 - partly because of these endocrine effects. The CDC’s 2022 guidelines now require doctors to warn patients about sexual and hormonal side effects before prescribing opioids. But most don’t.
What Doctors Should Be Doing
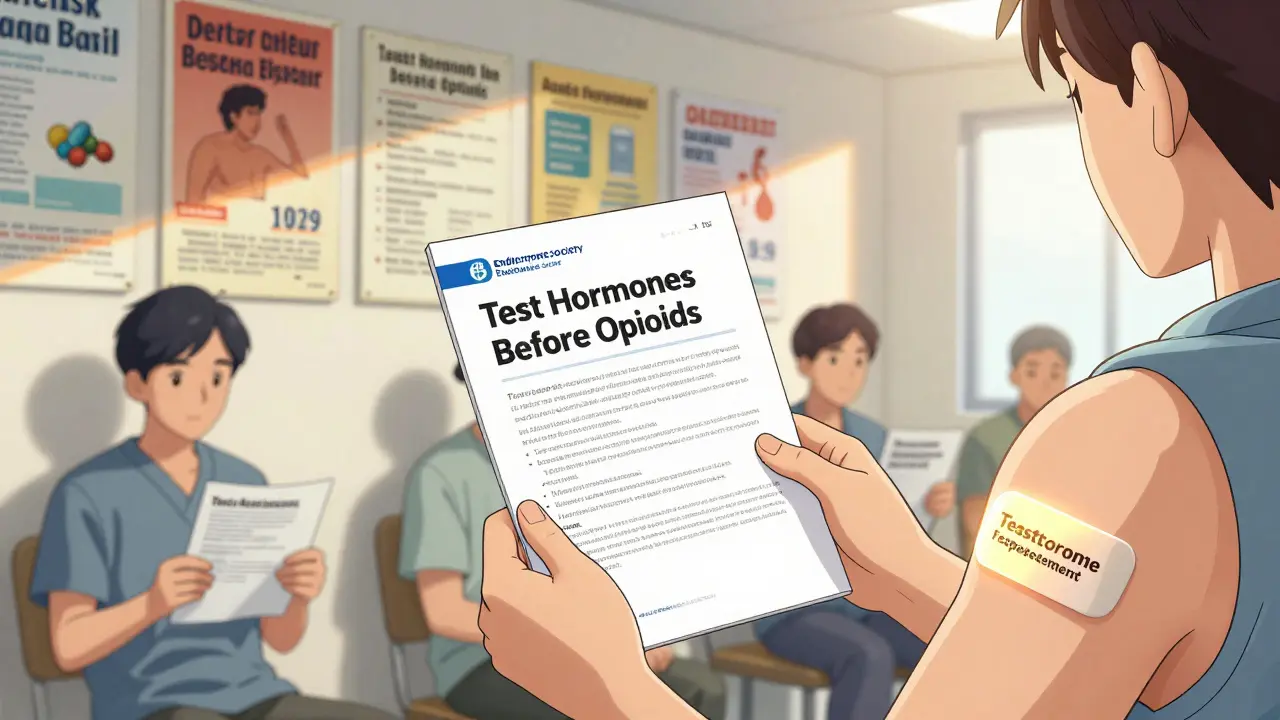
The Endocrine Society’s 2019 guidelines say it plainly: Testosterone levels should be checked in all men before starting chronic opioid therapy, and again every six months. For women, track menstrual cycles. Yet a 2023 study found only 38% of primary care doctors routinely screen for this. That’s not just negligence - it’s substandard care.
Here’s what effective care looks like:
- Baseline hormone test before starting opioids.
- Repeat testosterone test every 6 months for men.
- Ask women about period changes - don’t assume it’s stress.
- Don’t ignore complaints about sex drive or performance.
And if the tests show low testosterone? Treatment exists. Testosterone replacement therapy (TRT) - gels, injections, patches - improves sexual function in 70-85% of men. It’s not a cure for pain, but it fixes the hormone problem. For women, off-label testosterone patches (1-2 mg daily) show promise in small studies, improving libido in half the users. But there’s no standardized protocol. That’s a gap.
What You Can Do Right Now
If you’re on opioids and noticing changes in your body or sex life:
- Ask for a blood test: total testosterone, free testosterone, LH, FSH, and cortisol.
- Track your menstrual cycle if you’re a woman - note missed or irregular periods.
- Don’t let your doctor brush off your concerns. Say: “I’ve read this is a known side effect. Can we check my hormone levels?”
- If your levels are low, ask about TRT or other options - don’t wait.
- Consider non-opioid alternatives. Physical therapy, CBT, acupuncture, and certain antidepressants (like duloxetine) can help chronic pain without wrecking your hormones.
And if you want to reduce your opioid dose? Don’t quit cold turkey. Withdrawal can be brutal. Work with your doctor on a slow taper. New approaches like low-dose naltrexone combined with reduced opioids are showing success - boosting testosterone by 25-35% in 68% of patients while keeping pain under control.
The Bigger Picture
This isn’t just about sex. Low testosterone links to muscle loss, fatigue, bone thinning, and increased risk of heart disease. For women, long-term menstrual disruption can affect fertility and bone health. The body doesn’t just “get used to” this damage - it accumulates.
Meanwhile, the market is shifting. The testosterone replacement therapy market hit $3.2 billion in 2022 and is growing fast. Non-opioid pain treatments are projected to hit $59 billion by 2027. The FDA now requires opioid labels to mention endocrine risks. In January 2024, the Endocrine Society updated its guidelines to make hormone screening mandatory.
But here’s the hard truth: most patients still don’t know this is happening. And most doctors still aren’t checking. That’s why you have to be your own advocate. Your pain matters. But so does your body’s ability to function - including your sex life, your energy, your mood, and your long-term health.
Chronic pain doesn’t have to mean a broken hormone system. You don’t have to choose between relief and vitality. Better options exist. You just need to ask for them - and know what to look for.
Can long-term opioid use cause low testosterone?
Yes. Up to 63% of men on chronic opioid therapy develop biochemical hypogonadism, meaning their testosterone levels drop below 300 ng/dL. This happens because opioids suppress the brain signals that tell the testes to produce testosterone. The drop can occur within 30 days and worsens over time.
Do opioids affect women’s hormones too?
Yes. While estrogen levels usually stay normal, free testosterone drops significantly. About 87% of premenopausal women on long-term opioids develop menstrual problems - including missed periods (amenorrhea) in up to 67% of cases and irregular cycles in half of users. Libido loss is also extremely common.
Is testosterone replacement safe for people on opioids?
For men with confirmed low testosterone due to opioids, testosterone replacement therapy (TRT) is generally safe and effective - improving libido, energy, and mood in 70-85% of cases. But it requires monitoring. Risks include increased red blood cell count (polycythemia) in 15-20% of users. TRT doesn’t interfere with pain control and can be used alongside opioids under medical supervision.
What are alternatives to opioids for chronic pain?
Non-opioid options include physical therapy, cognitive behavioral therapy (CBT), certain antidepressants like duloxetine, gabapentinoids (for nerve pain), acupuncture, and NSAIDs (for inflammation). Studies show these often provide better long-term outcomes than opioids for non-cancer pain - without harming hormone levels or sexual function.
Should I stop opioids if I have sexual side effects?
Don’t stop suddenly - withdrawal can be dangerous. Talk to your doctor about a slow, supervised taper. In many cases, lowering the opioid dose or switching to a lower-risk option like buprenorphine can improve hormone levels without losing pain control. Combining reduced opioids with hormone therapy or non-opioid pain strategies often leads to the best results.
Why don’t doctors test for this more often?
Many doctors aren’t trained to connect sexual dysfunction with opioid use. It’s seen as a taboo topic, or assumed to be psychological. But guidelines from the Endocrine Society and CDC have been clear since 2019: routine hormone screening is standard of care. The gap between guidelines and practice is huge - only 38% of primary care doctors do it regularly.
Are there new treatments that reduce these side effects?
Yes. In 2023, the FDA approved buprenorphine buccal film (Belbuca), which causes 40% less hormone disruption than traditional opioids. New research also shows that adding low-dose naltrexone to reduced opioid regimens can restore testosterone levels in nearly 70% of patients. These aren’t widely used yet - but they’re promising.

Nicholas Miter
January 27, 2026 AT 03:00Been on oxycodone for 5 years for back pain. Didn't even realize my libido was gone until my girlfriend called me out. Thought it was just stress. Turns out my T was at 190. Doctor didn't test it until I brought up the article. Took 8 months to get TRT sorted. Now I'm back to feeling like myself. Not a cure for pain, but it fixed the hidden cost.
Suresh Kumar Govindan
January 28, 2026 AT 10:56This is a classic example of pharmaceutical industry manipulation. Opioids are deliberately engineered to induce endocrine suppression to create dependency through psychological degradation. The FDA's silence on this is not oversight-it is complicity.
James Nicoll
January 29, 2026 AT 07:51So let me get this straight. You're telling me the same drugs that make my back stop screaming also make my dick stop caring? And the doc just shrugs? I mean... cool. Guess I'm just supposed to be grateful I can still sit down.
Also, anyone else feel like we're living in a dystopian sitcom where the punchline is 'your hormones are broken but your insurance covers the opioids'?
Uche Okoro
January 31, 2026 AT 06:17The pathophysiological cascade initiated by mu-opioid receptor agonism induces hypothalamic suppression of GnRH pulsatility, leading to downstream inhibition of LH/FSH secretion and consequent gonadal hypofunction. This is not anecdotal-it is neuroendocrinological fact. The medical community’s failure to implement routine screening constitutes a systemic violation of the standard of care.
Peter Sharplin
February 1, 2026 AT 07:40I'm a nurse in pain management. I see this every week. Men don't talk about it. Women feel too ashamed. I had a 42-year-old woman cry because she thought her missed periods were 'just menopause coming early.' She was 31. We checked her T levels. She was in full hypogonadism. Started TRT. She cried again-this time because she could finally hug her husband without feeling empty.
Doctors need to ask. Not assume. Not dismiss. Ask.
John Wippler
February 2, 2026 AT 00:42You're not broken. You're just being treated with a blunt instrument. Opioids are like using a chainsaw to fix a squeaky hinge. Yeah, it stops the noise-but now your whole door’s in pieces.
I’ve helped 17 people taper off opioids and replace them with CBT + physical therapy + low-dose naltrexone. Every single one saw their libido and energy come back. Not all at once. But it came back. You don’t have to choose between pain relief and being human. There’s a third way.
And if your doctor won’t help? Find one who will. You deserve more than silence.
Faisal Mohamed
February 3, 2026 AT 07:13TL;DR: Opioids = hormone murder 🧬💀
But also… why are we still using opioids for chronic pain? We have better tools. We just don't fund them because pharma makes more money selling pills than teaching people how to move again.
Also, if your doc says 'it's just depression'-walk out. That's not care. That's negligence with a stethoscope.