Low Back Pain: What Red Flags Mean, When to Get Imaging, and How Exercise Therapy Works
 Dec, 19 2025
Dec, 19 2025
Most people will experience low back pain at some point in their life. It’s not rare-it’s normal. But not all back pain is the same. Some cases are just stiff muscles from sitting too long or lifting wrong. Others? They’re warning signs of something serious. Knowing the difference can save you from unnecessary scans, wasted time, and even permanent damage.
What Are Red Flags, Really?
Red flags aren’t just scary words doctors throw around. They’re specific symptoms that signal possible serious conditions like cancer, infection, a broken bone, or nerve damage. These make up only 1-2% of all low back pain cases. The other 98%? Mechanical pain-no tumor, no fracture, no emergency. But if you miss the 2%, the cost can be high. Here’s what to watch for:- History of cancer-If you’ve had cancer before, especially breast, lung, or prostate, new back pain needs attention. The chance of it spreading to your spine is small, but real.
- Unintentional weight loss-Losing 5% or more of your body weight in 6 months without trying? That’s not just dieting. It’s a red flag.
- Pain that wakes you up at night-If you’re tossing and turning because your back hurts more when you’re lying still, that’s different from soreness after a long day.
- Bladder or bowel control issues-Leaking urine or stool, or being unable to urinate even when your bladder feels full? This is a medical emergency. It could mean cauda equina syndrome.
- Saddle anesthesia-Numbness around your inner thighs, buttocks, or genitals. Think of it as the area that touches a saddle when you ride a horse. If that zone goes numb, get help now.
- Fever with back pain-Not just a cold. A fever above 38°C (100.4°F) with deep, constant pain in your lower spine? Could be an infection in the vertebrae.
- Major trauma-A fall from height, car crash, or direct blow to your back. Even if you feel okay afterward, get checked.
- Long-term steroid use-People on steroids for asthma, arthritis, or autoimmune diseases have weaker bones. A simple twist can cause a fracture.
Some things people think are red flags-but aren’t: age over 50 or 55, mild numbness in the leg, or pain that gets worse with movement. These are common and usually not dangerous. Yet, a 2022 survey found nearly 7 out of 10 doctors still order X-rays just because a patient is over 50. That’s not evidence-based. That’s over-testing.
When Do You Need an X-Ray or MRI?
Imaging doesn’t fix back pain. It just shows what’s going on inside. And in most cases, what’s shown doesn’t match your symptoms. A 55-year-old with chronic back pain might have bulging discs on an MRI-but so does a healthy 30-year-old who’s never had pain. That’s why guidelines say: don’t image unless there’s a red flag.The American College of Radiology and other major groups agree:
- No imaging needed for acute low back pain (under 4 weeks) without red flags. Rest, movement, and time are all you need.
- MRI without contrast is the go-to test if cauda equina syndrome, cancer, or infection is suspected. It shows soft tissue, nerves, and bone marrow better than anything else.
- X-rays have almost no role in chronic back pain without trauma or red flags. They won’t show disc problems, nerve pinching, or early infections. They only show bone alignment or fractures.
- Bone scans or CT with contrast are used only if infection is likely-especially if you’ve had recent surgery, IV drug use, or a weakened immune system.
Here’s the hard truth: Getting an MRI for non-specific back pain doesn’t make you feel better faster. It often leads to more tests, more anxiety, and sometimes unnecessary surgery. A 2021 study found that patients who got early MRIs were 30% more likely to have surgery within a year-even when their pain wasn’t getting worse.
Doctors are under pressure to do something. Patients want answers. But sometimes, the best answer is: wait, move, and monitor.
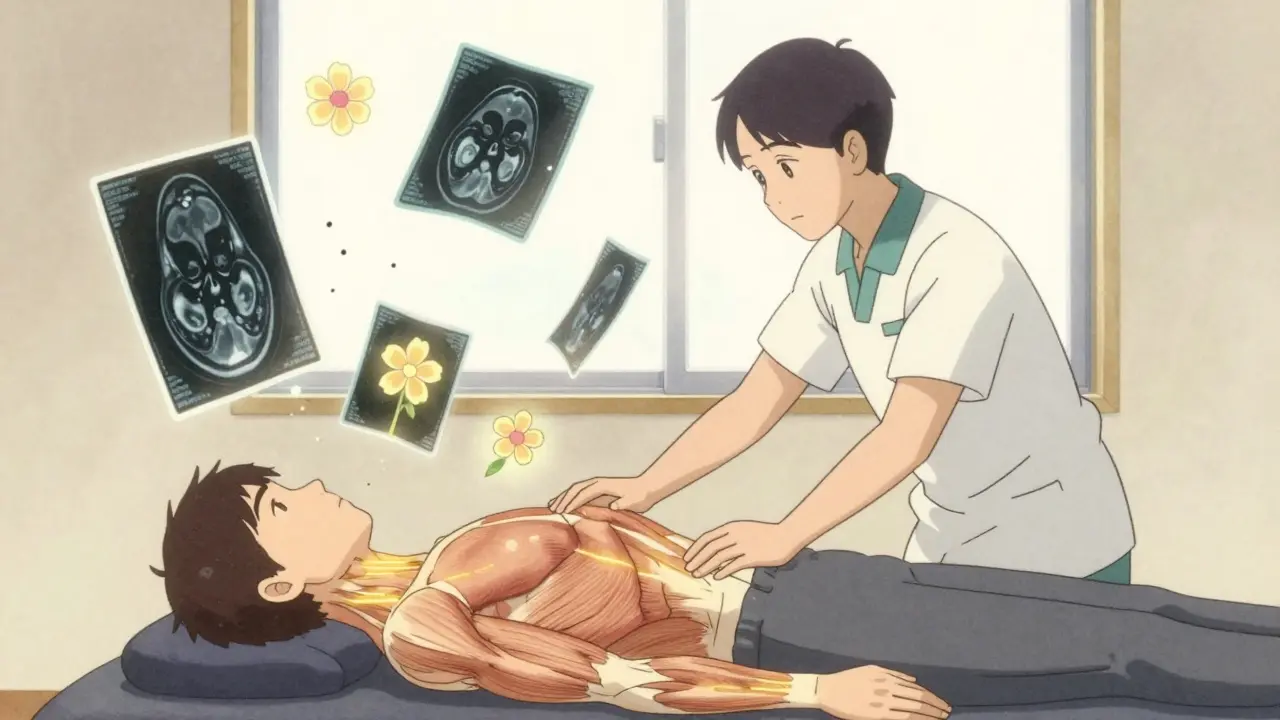
Exercise Therapy: The Most Proven Treatment
If you’ve been told to rest your back for weeks, you’ve been given bad advice. Movement isn’t the enemy. It’s the medicine.A 2020 Cochrane Review looked at 97 studies with nearly 20,000 people. The result? Exercise therapy reduced pain by an average of 6.6 points on a 100-point scale-and improved function by the same amount. That’s not a little improvement. That’s life-changing.
Not all exercise is equal. The best types for low back pain are:
- Motor control exercises-These teach your deep core muscles (like the transverse abdominis and multifidus) to fire properly. They’re not about crunches. They’re about learning to stabilize your spine before you lift, bend, or twist.
- Graded activity-This means slowly increasing your activity level, even if you’re in pain. You don’t wait until you’re pain-free to move. You move within your limits and build up over time.
- Combined programs-Mixing strength training, aerobic exercise (like walking or cycling), and flexibility work gives the best long-term results.
How much? At least 8 to 12 weeks. Two to three sessions per week with a physiotherapist or certified trainer. Then, keep going at home. Studies show that if you stick with it for more than 6 months, your chance of another episode drops by half.
Intensity matters too. Start light: 40-60% of your max strength. Build up to 70-85% over time. For cardio, aim for 60-80% of your max heart rate-enough to break a sweat but still hold a conversation. Twenty to thirty minutes, three times a week.
And here’s what no one tells you: adherence is everything. If you do only 30% of your exercises, you get 30% of the benefit. If you stop after 4 weeks? You’re back where you started. The goal isn’t to be perfect. It’s to be consistent.
Why Do So Many People Get Unnecessary Scans?
You’d think guidelines would be followed. But they’re not.A 2022 survey of over 1,200 primary care doctors found:
- 68% still thought age over 50 was a red flag.
- 43% routinely ordered X-rays for acute back pain-even without trauma or warning signs.
- Doctors spent an average of just 12.7 minutes per patient. The recommended time? 18 to 22 minutes.
Why? Time pressure. Fear of missing something. Patient demand. Insurance rules. All of it adds up.
But the cost isn’t just financial. Unnecessary imaging leads to overdiagnosis. People see a “degenerative disc” on their scan and start believing their back is broken. They avoid movement. They get scared. They become disabled by fear-not by anatomy.
There’s a better way. Tools like the Red Flag Decision Tool help doctors ask the right questions in under 5 minutes. A 2021 trial showed it cut unnecessary imaging by 28%. Simple. Smart. Effective.
What’s Changing in 2025?
Guidelines keep evolving. In 2023, the UK’s NICE guidelines removed “age over 55” as a standalone red flag. Why? Because data showed it didn’t predict serious disease any better than flipping a coin.Artificial intelligence is stepping in. A 2022 study in Nature Digital Medicine tested an AI tool that analyzed patient history, symptoms, and exam findings. It spotted serious spinal conditions with 89% accuracy-up from 73% with traditional checklists.
And research is moving toward personalized risk. The SPINE Act of 2022 funded $15 million to find blood markers or genetic signals that could predict who’s at risk for infection or cancer spreading to the spine. That’s the future: not one-size-fits-all red flags, but tailored risk scores.
But for now, the best tools are still the ones you’ve had for decades: listening, asking, moving.
What Should You Do Right Now?
If you have low back pain:- Check for red flags. If you have any of the serious signs (night pain, weight loss, bladder issues, fever, cancer history), see a doctor within 24 hours.
- If no red flags, stay active. Don’t rest for more than 1-2 days. Walk. Stretch. Move gently.
- Start exercise therapy. Find a physiotherapist who specializes in back pain. Don’t just do random YouTube videos. Get a plan.
- Don’t rush to imaging. Unless you have a red flag, an X-ray or MRI won’t help you feel better faster-and might make things worse.
- Be patient. Back pain improves over weeks, not days. Improvement is slow, but lasting.
Low back pain is common. But it doesn’t have to control your life. You don’t need a scan. You don’t need surgery. You need movement, knowledge, and time.
Is low back pain always serious?
No. About 98% of low back pain cases are caused by muscle strain, poor posture, or minor joint irritation-none of which are dangerous. Only 1-2% involve serious conditions like cancer, infection, or nerve damage. Most cases improve with movement and time.
Should I get an MRI if my back hurts?
Only if you have red flags like loss of bladder control, unexplained weight loss, fever, or a history of cancer. For most people, an MRI won’t change treatment and can lead to unnecessary worry or surgery. Imaging is not a first step-it’s a last resort for specific warning signs.
Can exercise make back pain worse?
If you do it too fast or with bad form, yes. But avoiding movement makes it worse long-term. Start slow-walking, gentle stretching, or core stabilization exercises. Pain during exercise should be mild and go away quickly. Sharp, shooting, or lasting pain means stop and adjust.
How long does exercise therapy take to work?
Most people notice small improvements in 2-4 weeks. Meaningful change takes 8-12 weeks of consistent exercise. Studies show benefits last for years if you keep moving. It’s not a quick fix-it’s a lifestyle change.
Is age a red flag for serious back pain?
No. Age alone-even over 60-is not a reliable indicator of serious spine problems. Many older adults have degenerative changes on scans but no pain. Guidelines now say age should not trigger imaging unless other red flags are present.
What should I avoid if I have low back pain?
Avoid prolonged bed rest (more than 48 hours), heavy lifting with poor form, and sudden twisting motions. Also avoid rushing into surgery or imaging without trying conservative care first. And don’t believe claims that your spine is “out of alignment”-that’s not a medical diagnosis.
If you’ve been told your back pain is “just aging” or “all in your head,” that’s wrong. It’s real-but it’s also manageable. You don’t need a scan. You don’t need surgery. You need to move, learn, and trust your body’s ability to heal.

Jackie Be
December 21, 2025 AT 10:07Jason Silva
December 21, 2025 AT 10:57Meina Taiwo
December 22, 2025 AT 06:34Stacey Smith
December 23, 2025 AT 02:35Adrian Thompson
December 23, 2025 AT 23:02Jerry Peterson
December 24, 2025 AT 09:46Hannah Taylor
December 24, 2025 AT 15:51Ben Warren
December 25, 2025 AT 01:16Peggy Adams
December 26, 2025 AT 07:33Teya Derksen Friesen
December 26, 2025 AT 23:15Swapneel Mehta
December 28, 2025 AT 14:34Theo Newbold
December 29, 2025 AT 19:51mukesh matav
December 30, 2025 AT 07:11Jay lawch
December 30, 2025 AT 21:36