Lung Cancer Screening for Smokers: What You Need to Know About Low-Dose CT
 Dec, 18 2025
Dec, 18 2025
Smoking is the biggest risk factor for lung cancer. But if you’ve smoked for years, you don’t have to wait for symptoms to appear before taking action. Low-dose CT screening can find lung cancer early-when it’s most treatable. And it’s not just for heavy smokers anymore. The rules changed in 2021, and now millions more people qualify. If you’re between 50 and 80, have smoked at least 20 pack-years, and either still smoke or quit within the last 15 years, this screening could save your life.
What Is Low-Dose CT Screening?
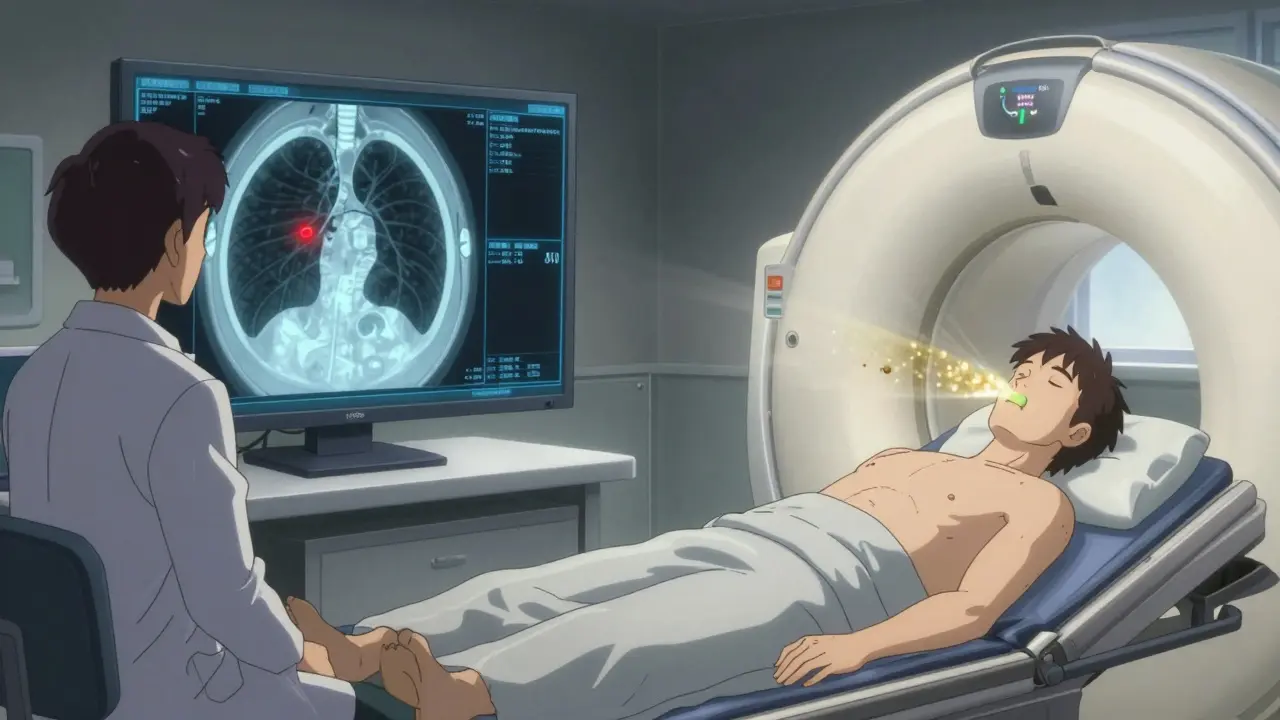
Low-dose CT, or LDCT, is a special type of chest scan that uses far less radiation than a regular CT scan. Instead of 7-8 millisieverts, it delivers about 1.5 millisieverts-roughly the same as a standard chest X-ray. You lie on a table, breathe in, hold your breath for a few seconds, and the machine takes detailed pictures of your lungs. The whole thing takes less than 10 minutes. No needles, no fasting, no prep. It’s quick, painless, and non-invasive.
This isn’t a diagnostic test. It’s a screening tool. That means it doesn’t tell you if you have cancer-it finds suspicious spots that need closer look. Most of these spots turn out to be harmless. But catching the real ones early makes a huge difference.
Who Should Get Screened?
The U.S. Preventive Services Task Force (USPSTF) updated its guidelines in 2021, and the changes matter. Before, you had to be 55 or older with 30 pack-years of smoking. Now, you qualify if you’re 50-80, have smoked at least 20 pack-years, and either still smoke or quit within the past 15 years.
What’s a pack-year? Simple: smoking one pack a day for one year equals one pack-year. Two packs a day for 10 years? That’s 20 pack-years. Smoking half a pack a day for 40 years? Also 20 pack-years. It’s not about how hard you smoked-it’s about total exposure.
Screening stops when you’ve quit smoking for 15 years or if your health makes curative surgery unlikely. If you have heart failure, severe COPD, or other conditions that limit life expectancy to under 10-15 years, screening won’t help. It’s not about age alone-it’s about whether you’d benefit from treatment if cancer is found.
Why It Works: The Evidence
The National Lung Screening Trial (NLST), published in 2011, was the first big study to prove LDCT saves lives. It compared over 53,000 high-risk smokers who got either LDCT or chest X-rays annually for three years. Those who got LDCT had a 20% lower chance of dying from lung cancer. That’s not a small win. It’s life-changing.
Since then, modeling studies estimate that expanding screening to the new criteria could prevent up to 15,000 extra lung cancer deaths each year in the U.S. alone. That’s because the updated rules catch cancer in people who are younger and have smoked less-but still at high risk. A 53-year-old who smoked a pack a day for 25 years is just as likely to develop early-stage lung cancer as a 65-year-old who smoked two packs a day for 30 years.
The Downsides: False Positives and Anxiety
LDCT isn’t perfect. About 13.9% of screenings show something suspicious-something that needs follow-up. But in most cases, it’s not cancer. It could be scar tissue, inflammation, or a benign nodule. Still, that leads to more tests: repeat scans, biopsies, even surgeries.
One in three people who get a false positive report feeling anxious for months. Some avoid future screenings because of the stress. A 2022 study in Cancer Epidemiology, Biomarkers & Prevention found 37% of patients with false positives had moderate to severe anxiety lasting longer than six months.
There’s also radiation. While low-dose, it’s still radiation. Getting scanned every year adds up. But the risk from radiation is tiny compared to the risk of missing early lung cancer in someone with a long smoking history.
And then there’s overdiagnosis-finding cancers that would never have caused harm. These slow-growing tumors might never spread. But once found, they’re often treated anyway. That means surgery, chemo, or radiation you didn’t need. Experts estimate this happens in 5-10% of screen-detected cancers.
Who Shouldn’t Get Screened?
Not everyone who smokes needs LDCT. If you’re under 50, even with a heavy smoking history, your risk isn’t high enough yet to make screening worthwhile. If you’ve quit for more than 15 years, your risk drops significantly. Screening isn’t recommended then.
People with serious health problems that make surgery risky-like advanced heart disease or severe lung disease-are usually not candidates. If you can’t tolerate surgery if cancer is found, then screening won’t help you live longer. It might just add stress.
And if you’ve never smoked? Screening isn’t for you. The benefits don’t outweigh the risks. Lung cancer in never-smokers happens, but it’s rare and often caused by different factors like radon or genetics. Screening isn’t designed for those cases.
Getting Started: What Happens Before the Scan?
You can’t just walk in and ask for a low-dose CT. Medicare and most insurers require a shared decision-making visit first. That means a 20-30 minute talk with your doctor or nurse. They’ll explain:
- The 1.5-2% absolute reduction in lung cancer death risk
- The 13.9% chance of a false positive
- What happens if something is found
- Why quitting smoking still matters-even if you’re getting screened
This isn’t a formality. It’s required. And it’s important. Many people skip this step and end up confused when they get called back for another scan.
Doctors are supposed to use Lung-RADS (Lung Imaging Reporting and Data System) to classify results. Category 1 means normal-come back next year. Category 2 is benign-no action needed. Category 3 is probably benign-check again in 6 months. Category 4 is suspicious-need biopsy or more tests. Knowing what the results mean helps reduce panic.
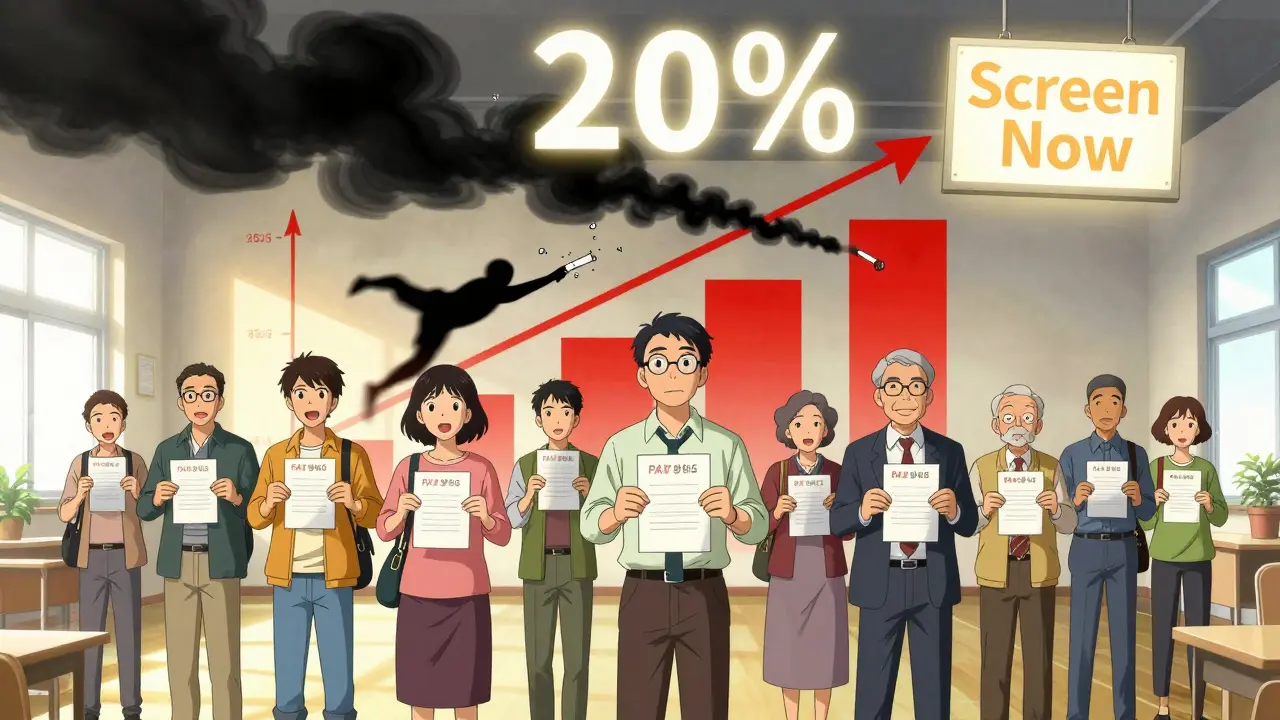
Access and Barriers: Why So Few Get Screened
Here’s the hard truth: even though 14.5 million Americans now qualify, only about 8.3% got screened in 2022. That’s up from 5.7% in 2020, but still way too low.
Why? First, most people don’t know they qualify. A 2022 Medicare survey found 68% of eligible people didn’t even realize they were candidates. Second, doctors don’t always bring it up. Nearly half of missed screenings happened because no provider recommended it.
Then there’s access. In rural areas or low-income neighborhoods, there might not be an ACR-accredited screening center nearby. One Reddit user said they drove 127 miles for their scan. Transportation, cost, and lack of awareness are huge barriers.
Black Americans are 20% less likely to get screened than White Americans, even though they have higher lung cancer rates. That’s a gap that needs fixing.
What’s New in 2025?
AI is starting to help. In September 2023, the FDA cleared the first AI tool for LDCT analysis-LungAssist by VIDA Diagnostics. In trials, it cut false positives by 15.2%. That means fewer unnecessary biopsies and less anxiety. It’s not replacing radiologists-it’s helping them spot things faster and more accurately.
Another advance is the PLCOm2012 risk model. It doesn’t just look at pack-years. It adds in family history, education level, breathing problems, and even past infections. This could help doctors decide who benefits most from screening-and who might be better off focusing on quitting.
And the number of accredited centers is growing. As of December 2023, there were 1,842 ACR-accredited lung cancer screening sites in the U.S. That’s up from under 1,000 in 2020. Coverage is still uneven, but it’s improving.
What to Do Next
If you’re 50-80 and have smoked 20 pack-years or more:
- Ask your doctor if you’re a candidate for LDCT screening.
- Don’t wait for them to bring it up. Bring it up yourself.
- Be ready to talk about your smoking history-how much, how long, when you quit.
- Ask about Lung-RADS and what happens if something is found.
- If your doctor says no, ask why. Get a second opinion if needed.
If you’re still smoking? Screening isn’t a substitute for quitting. It’s a backup plan. Quitting now still cuts your lung cancer risk by half within 10 years. And it helps your heart, your lungs, your whole body.
Screening doesn’t prevent cancer. But it can catch it early enough to cure it. And for someone who’s smoked for decades, that’s the best shot they’ve got.
Who qualifies for low-dose CT lung cancer screening?
You qualify if you’re between 50 and 80 years old, have a smoking history of at least 20 pack-years (like one pack a day for 20 years), and either still smoke or quit within the past 15 years. Screening stops if you’ve quit for 15 years or if your health makes curative treatment unlikely.
Is low-dose CT the same as a regular CT scan?
No. A low-dose CT (LDCT) uses about 1.5 millisieverts of radiation-much less than a standard CT, which can use 7-8 millisieverts. It’s designed to find early signs of lung cancer with minimal radiation exposure. It’s not meant for full-body imaging or diagnosing other conditions.
How often should I get screened?
Annual screening is recommended for all eligible individuals. You should get a low-dose CT scan once every year as long as you meet the criteria. Skipping years reduces the benefit. Consistency matters.
What if the scan shows something abnormal?
An abnormal result doesn’t mean you have cancer. About 14 out of every 100 scans show something suspicious, but most turn out to be harmless. You’ll likely need a follow-up scan in 3-6 months, or possibly a biopsy. Your doctor will use Lung-RADS to guide next steps based on the size, shape, and growth of the spot.
Does Medicare cover low-dose CT screening?
Yes. Medicare covers annual low-dose CT screening for people aged 50-77 who meet the smoking history criteria. You must have a shared decision-making visit with your provider first, and the scan must be done at an ACR-accredited facility. No copay is required if your provider accepts Medicare assignment.
Can I get screened if I’ve never smoked?
No. Current guidelines only recommend LDCT for people with a significant smoking history. Lung cancer in never-smokers is rare and often caused by different factors like radon, genetics, or air pollution. Screening isn’t proven to help these groups and isn’t covered by insurance.
Does quitting smoking make screening unnecessary?
Not immediately. If you quit within the last 15 years, you still qualify for screening because your cancer risk remains elevated. After 15 years of being smoke-free, your risk drops enough that screening is no longer recommended. But quitting is still the best way to reduce your risk long-term.

Danielle Stewart
December 18, 2025 AT 18:16My mom got screened last year after I nagged her for months. She’s 62, smoked a pack a day for 28 years, quit 12 years ago. Found a tiny nodule-turned out to be scar tissue from an old pneumonia. Still, knowing it wasn’t cancer? Priceless. Don’t wait until you’re coughing up blood. Just get it done.
Ryan van Leent
December 19, 2025 AT 01:31Adrienne Dagg
December 20, 2025 AT 05:48Kinnaird Lynsey
December 22, 2025 AT 03:54I appreciate the nuance here. Most people think it’s either "just quit smoking" or "get scanned and hope for the best." But the reality is messier-false positives, anxiety, overdiagnosis. The fact that guidelines now include people with 20 pack-years instead of 30? That’s progress. Still, access is a joke in rural areas. My cousin drove 3 hours each way. No public transit. No ride-share. Just her and a rental car.
shivam seo
December 22, 2025 AT 09:01benchidelle rivera
December 23, 2025 AT 23:01This post is a public service. If you’re reading this and you qualify-do not delay. I’ve seen too many patients come in with stage IV disease because they thought "it wouldn’t happen to me." Screening isn’t about fear. It’s about agency. You have the power to catch this early. Use it. And yes, quitting is still the goal-but screening buys you time to make that change without dying before you get there.
Andrew Kelly
December 24, 2025 AT 08:46Let me guess-the government wants us to get scanned so they can sell us more chemo. Radiation exposure adds up. And what about all the people who get biopsied for nothing? That’s medical trauma. I know a guy who got 4 follow-ups over 2 years because of a benign cyst. He lost his job because he was too anxious to go to work. This isn’t prevention-it’s profit-driven fearmongering.
Anna Sedervay
December 25, 2025 AT 09:16One must question the epistemological underpinnings of population-based screening protocols when the base rate of malignancy among incidental pulmonary nodules remains suboptimal. The NLST trial, while statistically significant, suffers from selection bias and lacks generalizability to non-White, non-Medicare populations. Furthermore, the proliferation of Lung-RADS as a quasi-regulatory framework constitutes a form of diagnostic hegemony that pathologizes benign physiological variation.
And yet-despite these methodological concerns-I acknowledge that, pragmatically, for a 58-year-old former pack-a-day smoker with a family history of adenocarcinoma, the risk-benefit calculus remains nontrivial.
Matt Davies
December 26, 2025 AT 06:37Man, I’ve been a smoker since I was 16. 37 now. 25 pack-years. I’ve had a cough for years I just ignore. But reading this? I finally called my GP. Got the shared-decision thing scheduled. Honestly? I didn’t think I’d qualify. I thought I was "too young." Turns out, I’m exactly who this was made for. Feels weird to say it, but… I’m kinda proud of myself for doing this. Not because I’m brave. Because I’m done pretending I’m invincible.
mark shortus
December 27, 2025 AT 16:27Jedidiah Massey
December 27, 2025 AT 19:42LDCT is essentially a high-sensitivity radiological proxy for smoking-related epigenetic dysregulation. The PLCOm2012 model, when integrated with AI-assisted volumetric analysis (e.g., VIDA’s LungAssist), achieves a sensitivity of 92.3% and specificity of 84.7% in prospective cohorts. However, the cost per life-year saved remains contentious under QALY frameworks. The 15% reduction in false positives is statistically significant (p<0.01), but clinical utility hinges on equitable access to follow-up diagnostics-particularly in Medicaid-expansion states with fragmented care networks.
Alex Curran
December 29, 2025 AT 04:18Kathryn Featherstone
December 30, 2025 AT 08:13Thank you for writing this with such care. I work in community health and see so many people who don’t know they qualify. We’ve started handing out little cards with the criteria printed on them-pack-year calculator, age range, quit timeline. Simple. No jargon. One woman said, "I thought I had to be 60 and smoke three packs a day." She cried when she realized she qualified. We need more of this-not more ads. Just clear, kind, honest info.