Medications Safe While Breastfeeding: Evidence-Based Choices
 Jan, 19 2026
Jan, 19 2026
When you’re breastfeeding, every pill you take feels like a decision that could affect your baby. You might wonder: Is this headache medicine safe? What about my antidepressant? Can I take allergy pills without risking my milk supply? The truth is, most medications are safe to use while breastfeeding - but not all. And too often, mothers stop nursing because they’re told to, when they don’t have to.
Most Medications Are Safe - Here’s Why
The big myth is that if a drug gets into breast milk, it’s dangerous. But that’s not how it works. The amount of medicine that passes into milk is usually tiny - often less than 1% of the mother’s dose. What matters isn’t just whether it’s present, but how much the baby actually absorbs and whether their body can handle it. According to the American Academy of Pediatrics and the U.S. National Library of Medicine, over 85% of prescription drugs have enough safety data to be used while breastfeeding. Only a handful are truly contraindicated. The key is knowing which ones are safe and which ones need caution. Resources like LactMed a free, evidence-based database from the National Institutes of Health that tracks drug levels in breast milk, infant exposure, and documented side effects make it easy to check. If a medication is safe for a baby to take directly - like acetaminophen for fever - it’s almost always safe for a breastfeeding mom too.Pain Relief: What You Can Take Without Worry
For pain or fever, you have two rock-solid choices: acetaminophen and ibuprofen. Both are first-line recommendations across every major medical group, including the Mayo Clinic and the American Academy of Family Physicians. Acetaminophen (Tylenol) transfers at only 0.04-0.23% of the maternal dose. That’s less than a drop in a bath. Ibuprofen (Advil, Motrin) transfers a bit more - up to 1.85% - but still far below levels that would affect an infant. Neither drug has ever been linked to side effects in breastfed babies, even with long-term use. Avoid naproxen (Aleve) for more than a few days. It stays in your system longer (12-17 hours), and there are rare case reports of anemia or vomiting in babies after prolonged exposure. If you need longer-term pain relief, stick with acetaminophen or ibuprofen. Opioids are trickier. Codeine is risky because some people metabolize it too quickly, turning it into dangerous levels of morphine. The FDA issued a black box warning for this reason. Morphine and hydromorphone are safer options - but only if used at the lowest dose for the shortest time. Always watch your baby for unusual sleepiness, trouble feeding, or slow breathing.Antibiotics: Common Prescriptions and Real Risks
If you have an infection, you don’t need to stop breastfeeding. Most antibiotics pass into milk in tiny amounts and don’t harm the baby. Penicillins like amoxicillin and cephalosporins like cephalexin are ideal. They’ve been used for decades in newborns and have near-zero risk. The Relative Infant Dose (RID) for amoxicillin is just 0.3-1.5% - and no adverse effects have been documented. Macrolides like azithromycin are also safe. It transfers at only 0.05-0.1% of the maternal dose. Erythromycin is mostly safe too, but there’s a small theoretical link to infant pyloric stenosis - a rare condition that causes vomiting. That’s why azithromycin is preferred. Fluoroquinolones like ciprofloxacin have an RID of 0.5-1.0%. Animal studies raised concerns about joint damage, but no cases have ever been seen in breastfed babies. Still, they’re usually reserved for serious infections. Doxycycline is okay for short courses (under 21 days). Long-term use could theoretically affect tooth color, but no cases have been reported in breastfed infants. For longer treatments, your doctor might switch you to a safer option.
Psychiatric Medications: Managing Mental Health While Nursing
Depression and anxiety don’t take a break after birth - and neither should your treatment. Untreated mental illness is far riskier for your baby than most medications. Sertraline (Zoloft) is the gold standard. It transfers at 1.7-7.0% of the maternal dose, and infant blood levels are often undetectable. Multiple studies show no developmental delays or behavioral issues in babies exposed to sertraline long-term. Paroxetine (Paxil) is another top choice. It’s similar in safety, though some moms report it causes more drowsiness in their babies. If that happens, switching to sertraline often helps. Fluoxetine (Prozac) is not ideal. It has a very long half-life - up to 6 days - and can build up in the baby’s system. Studies show about 2% of exposed infants develop irritability or feeding problems. If you’re already on fluoxetine and doing well, don’t stop abruptly - talk to your doctor about switching. For anxiety, lorazepam (Ativan) is preferred. It’s short-acting (10-20 hour half-life) and transfers minimally. Avoid clonazepam (Klonopin) - its long half-life (30-40 hours) means it can pile up in your baby’s system, leading to drowsiness or poor feeding. Quetiapine (Seroquel) and risperidone (Risperdal) are safe for psychosis or bipolar disorder. Quetiapine at doses up to 400 mg daily results in less than 1% of the maternal dose in milk, with normal infant development in long-term follow-ups.Allergy and Cold Medicines: Don’t Let Sinus Pressure Stop You
Allergies and colds are common postpartum - and you don’t need to suffer. But not all OTC meds are created equal. Nasal sprays like fluticasone (Flonase) and budesonide (Rhinocort) are ideal. They’re absorbed so poorly in your nose that almost none enters your bloodstream - meaning virtually nothing reaches your milk. Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) are safe. Their RIDs are below 0.5%, and there are hundreds of case reports with no side effects. First-generation antihistamines like diphenhydramine (Benadryl) are risky. They cross into milk more easily (RID 1.0-2.0%) and can make babies sleepy or fussy. They may also reduce milk supply slightly. Use them only for occasional sleep aid, not daily allergy relief. Pseudoephedrine (Sudafed) is the worst offender for milk supply. Studies show it can drop production by 24% on average. Some moms lose up to half their supply after one dose. If you need a decongestant, try saline rinses, steam, or a humidifier instead.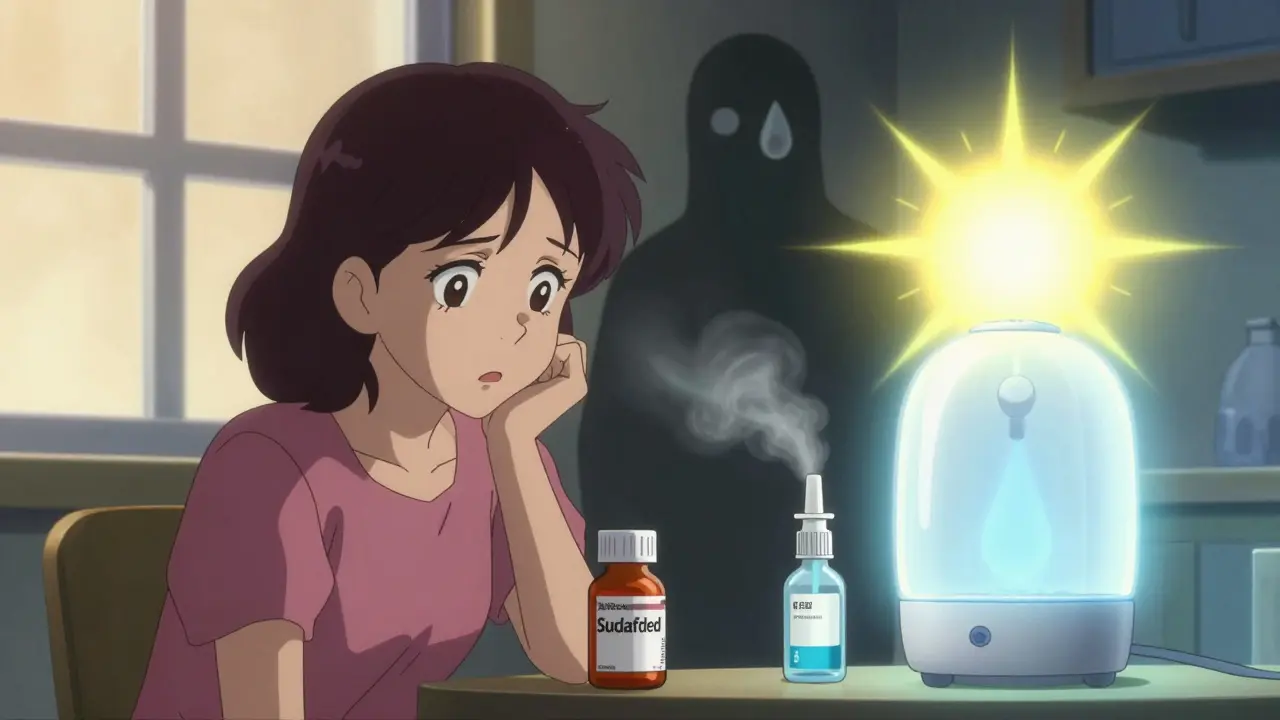
When to Stop Breastfeeding - And When You Don’t Have To
There are only a few situations where breastfeeding must pause. Radioactive iodine (I-131) for thyroid cancer requires you to stop breastfeeding for 3-6 weeks. The radiation can damage your baby’s thyroid. You’ll need to pump and dump during this time to maintain supply. Chemotherapy drugs (antineoplastics) are generally avoided. Each drug has different risks, so work with your oncologist and a lactation consultant. Some can be paused during treatment and resumed afterward. Lithium is high-risk. It passes into milk at 30-50% of maternal levels. Babies can develop toxicity - tremors, poor feeding, or even kidney issues. If you’re on lithium, your baby needs weekly blood tests to monitor levels. Only continue if you can commit to close monitoring. For everything else - antibiotics, antidepressants, painkillers, allergy meds - you can usually keep nursing. The risk of stopping breastfeeding often outweighs the risk of the medication.What to Do If You’re Unsure
Don’t guess. Don’t rely on internet forums or well-meaning but misinformed advice. Use trusted resources:- LactMed Free, peer-reviewed, updated quarterly, with exact drug levels and infant effects
- InfantRisk Center Offers real-time advice from experts; handles over 15,000 calls a year
- MotherToBaby Provides personalized risk assessments based on your specific medication and baby’s age
Final Thought: Breastfeeding Is Worth Protecting
About 10-15% of mothers stop breastfeeding because they’re told a medication isn’t safe - when it actually is. That’s not just a loss of nutrition. It’s a loss of bonding, immune protection, and long-term health benefits for both you and your baby. The science is clear: most medications are compatible with breastfeeding. The key is choosing wisely, using evidence, and not letting fear make the decision for you. If your baby can take it, you can usually take it too - with the right guidance.Can I take ibuprofen while breastfeeding?
Yes. Ibuprofen is one of the safest pain relievers for breastfeeding mothers. It transfers in very small amounts (0.38-1.85% of the maternal dose), has no known side effects in infants, and is recommended by the American Academy of Family Physicians and Mayo Clinic. Use the lowest effective dose and avoid long-term daily use unless necessary.
Is Zoloft safe for breastfeeding moms?
Yes. Sertraline (Zoloft) is the most studied and preferred antidepressant for breastfeeding. It transfers minimally into breast milk, with infant blood levels often undetectable. Multiple long-term studies show no developmental delays or behavioral issues in babies exposed to sertraline. It’s considered a first-line choice by the American Academy of Pediatrics and Women’s Mental Health experts.
Does Sudafed reduce milk supply?
Yes. Pseudoephedrine (Sudafed) can reduce milk production by an average of 24%. Some mothers report losing up to half their supply after one dose. The American Academy of Family Physicians advises avoiding it if possible. Use saline sprays, humidifiers, or steam instead. If you must use it, take the lowest dose and monitor your supply closely.
Are antihistamines safe while breastfeeding?
Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) are safe. They transfer in tiny amounts (under 0.5%) and have no documented side effects in breastfed babies. Avoid first-generation options like diphenhydramine (Benadryl), which can cause drowsiness in infants and may reduce milk supply.
What should I do if I need antibiotics while breastfeeding?
Most antibiotics are safe. Penicillins (like amoxicillin) and cephalosporins are first-line choices with no known risks. Macrolides like azithromycin are also safe. Avoid clindamycin if your baby has a history of diarrhea. Always complete your full course - stopping early risks infection recurrence. If you’re unsure, check LactMed or call the InfantRisk Center.
Can I breastfeed after radioactive iodine treatment?
No. Radioactive iodine (I-131) passes into breast milk and can damage your baby’s thyroid. Breastfeeding must stop for 3-6 weeks after treatment. You’ll need to pump and dump during this time to maintain your supply. Consult your doctor for a plan to resume breastfeeding safely after the radiation clears.
If you’re taking any medication and breastfeeding, your best move is to check LactMed or call the InfantRisk Center. Don’t assume the worst. Most of the time, you can keep doing what you’re doing - safely.

Kelly McRainey Moore
January 20, 2026 AT 01:34Thank you for this. I was so scared to take ibuprofen after my c-section, but now I feel like I can finally breathe again. So many moms are told to stop nursing over nothing.
Barbara Mahone
January 21, 2026 AT 02:04The LactMed database is gold. I’ve been using it since my second kid. Doctors rarely know the details, but this resource is peer-reviewed, free, and updated quarterly. Bookmark it. Print it. Share it.
michelle Brownsea
January 22, 2026 AT 10:41Let’s be real-this post is dangerously oversimplified. Just because a drug transfers at ‘less than 1%’ doesn’t mean it’s harmless. Babies’ livers aren’t fully developed. You’re normalizing risk. Where’s the caution? Where’s the nuance? This is the kind of advice that gets babies hospitalized.
Amber Lane
January 22, 2026 AT 18:32My baby slept through the night after I switched from Benadryl to Zyrtec. No more fussiness. No more leaky breasts. Just peace.
Gerard Jordan
January 24, 2026 AT 13:21Big shoutout to the InfantRisk Center 🙌 I called them at 2 a.m. with a panic about my new antibiotic. They answered in 30 seconds. Real humans. Real expertise. No bots. This is the kind of support new moms need.
Andrew Rinaldi
January 24, 2026 AT 20:20It’s interesting how we treat breastfeeding like a moral obligation instead of a personal choice. The science here is solid, but the guilt around stopping? That’s cultural. If you need to stop for your mental health, or your physical health, that’s not failure. It’s wisdom.
Stephen Rock
January 25, 2026 AT 13:00Wow. Another feel-good mommy blog dressed up as medical advice. You know what’s really dangerous? Trusting a Wikipedia-style wiki with no peer review. LactMed? It’s a glorified wiki. And you’re telling moms to ignore their doctors? That’s not evidence-it’s ego. I’ve seen infants with liver enzyme spikes from ‘safe’ meds. You think it’s fine because you read a blog? Wake up.
Ashok Sakra
January 26, 2026 AT 14:00I am from India and my wife took Zoloft while breastfeeding. Baby fine. No problem. But people here say all medicine bad. They say breast milk must be pure. Pure? Like what? Water? My wife cried because they said she was poison. This post is true. Tell them.