Mineral Bone Disorder in CKD: Understanding Calcium, PTH, and Vitamin D
 Dec, 1 2025
Dec, 1 2025
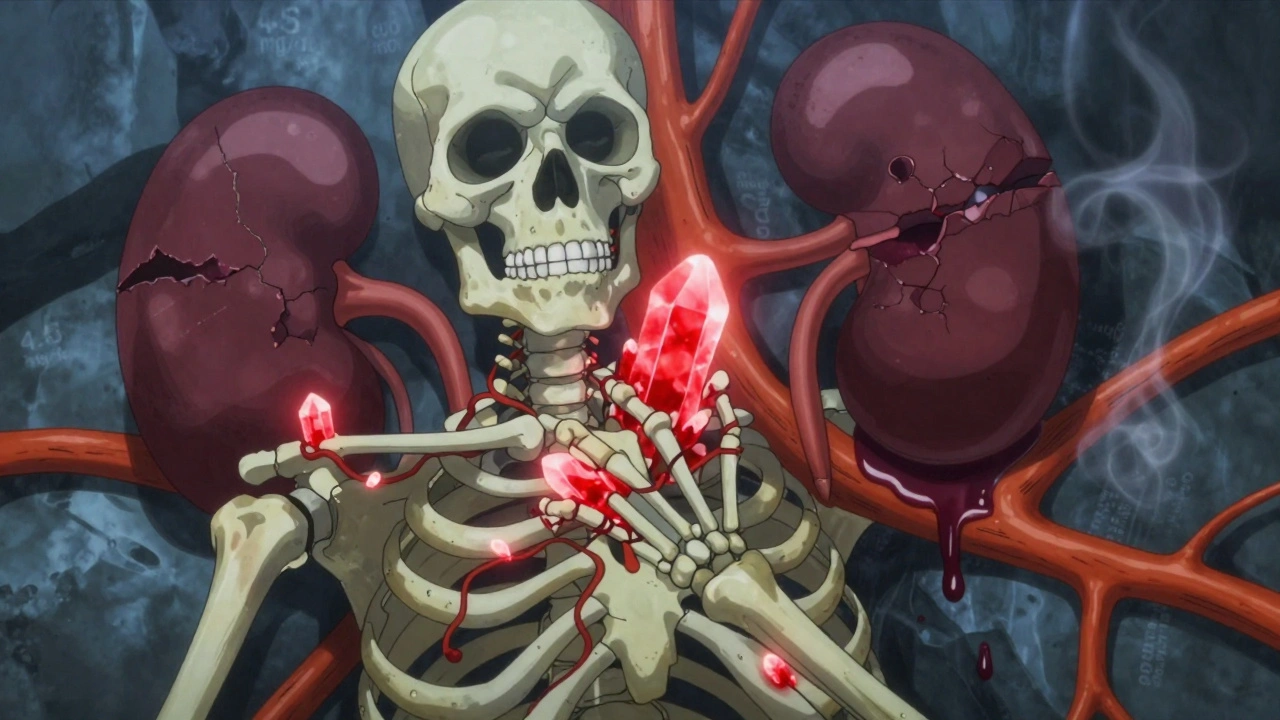
When your kidneys start to fail, they don’t just stop filtering waste-they also stop managing the minerals that keep your bones strong and your heart healthy. Mineral Bone Disorder in CKD, or CKD-MBD, is not a single problem. It’s a chain reaction: high phosphate, low vitamin D, and runaway PTH levels all feeding off each other, quietly damaging your bones and arteries long before you feel any symptoms.
What Exactly Is CKD-MBD?
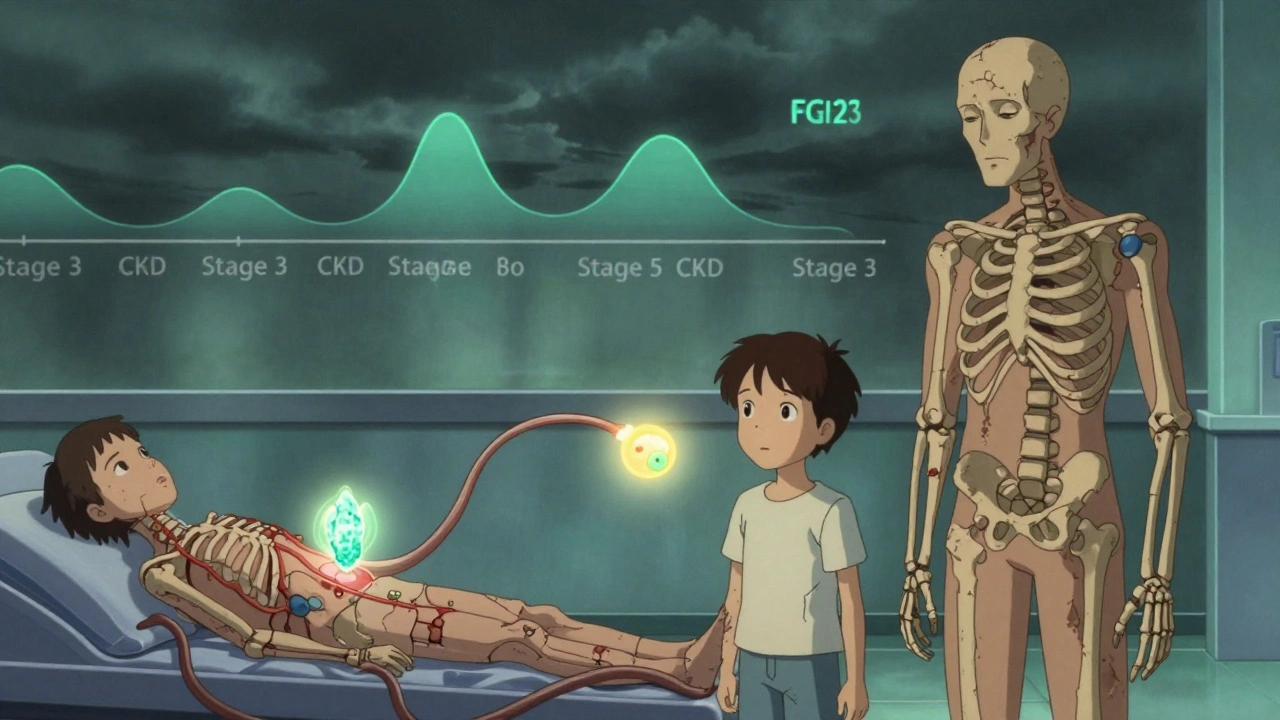
CKD-MBD isn’t just about weak bones, even though that’s what many people think. The old term, renal osteodystrophy, only described bone changes. But in 2006, experts realized the issue goes deeper. It’s a systemic disorder affecting how your body handles calcium, phosphorus, parathyroid hormone (PTH), and vitamin D. By Stage 3 of chronic kidney disease (CKD), when kidney function drops below 60% of normal, this imbalance begins. By Stage 5-when dialysis is needed-nearly everyone has it.
Think of it like a broken thermostat. Your kidneys used to keep mineral levels in check. Now, they can’t. Phosphate builds up because the kidneys can’t flush it out. That triggers a cascade: your body tries to compensate, but ends up making things worse. The result? Fractures, heart disease, and early death.
The Three-Pillar Problem: Phosphate, PTH, and Vitamin D
CKD-MBD runs on three interconnected problems:
- High phosphate: When kidneys fail, phosphate sticks around. Levels above 4.5 mg/dL are common in Stage 3-5 CKD. That’s not just a lab number-it’s a ticking time bomb for your blood vessels.
- Low vitamin D: Healthy kidneys convert vitamin D into its active form, calcitriol. In CKD, that process drops by 50-80%. Without it, your gut can’t absorb calcium, and your bones weaken.
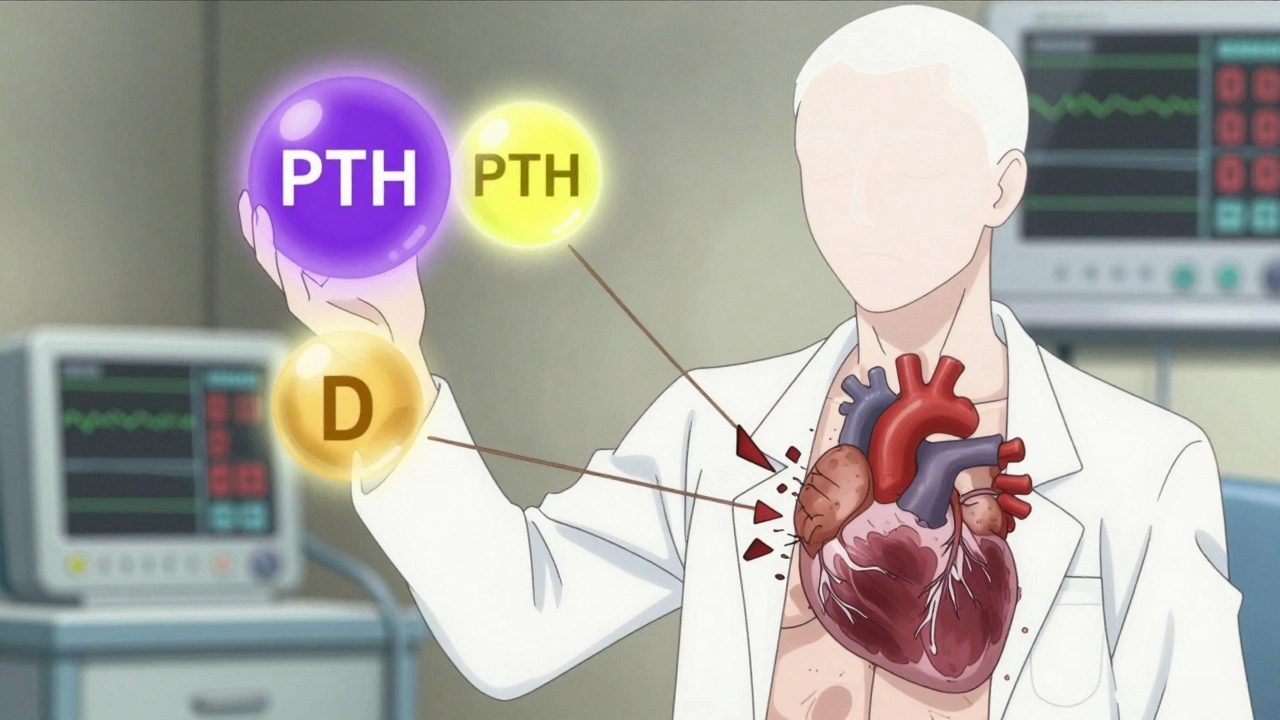
- High PTH: Low calcium and low vitamin D trick your parathyroid glands into overproducing PTH. This hormone tries to pull calcium from your bones to fix the imbalance. But in CKD, your bones stop responding properly. So you get high PTH, but your bones still break.
These three don’t act alone. High phosphate boosts another hormone called FGF23, which further blocks vitamin D production. And as FGF23 rises, it damages your heart. Meanwhile, a protein called sclerostin increases, shutting down bone-building cells. So your bones don’t just weaken-they stop repairing themselves.
Why This Matters: Fractures and Heart Attacks
People with CKD on dialysis have a 4-5 times higher risk of hip fractures than healthy adults their age. But here’s the twist: many of these patients have normal bone density scans. That’s because the real problem isn’t density-it’s quality. Their bones are brittle, poorly formed, or too soft.
Even more dangerous is vascular calcification. Calcium and phosphate don’t just deposit in bones-they start sticking to your arteries. By Stage 5, 75-90% of dialysis patients have visible calcification in their heart vessels. Each 1 mg/dL rise in phosphate means an 18% higher risk of dying. Each 30% rise in PTH adds another 12% risk. Vitamin D deficiency, which affects 80-90% of CKD patients, bumps up mortality by 30%.
This isn’t theoretical. In a 2023 study, patients with phosphate levels above 5.5 mg/dL had a 40% higher chance of dying within two years compared to those within target range. And the damage doesn’t wait. By Stage 3, FGF23 is already rising-years before phosphate spikes. That’s why early detection matters.
How Doctors Diagnose It
There’s no single test for CKD-MBD. Instead, doctors watch a few key numbers:
- Serum phosphate: Target is 2.7-4.6 mg/dL for Stage 3-5 CKD; 3.5-5.5 mg/dL for dialysis.
- PTH: Target is 2-9 times the upper limit of normal for your lab’s assay. That’s usually 150-600 pg/mL, but varies.
- Calcium: Keep between 8.4-10.2 mg/dL. Too high? You risk calcification. Too low? Bones suffer.
- 25-hydroxyvitamin D: Aim for at least 30 ng/mL. Most CKD patients are below 20.
Bone biopsy is the gold standard to tell if bone turnover is high, low, or mixed. But it’s invasive. So most clinics use blood markers instead: PTH plus bone-specific alkaline phosphatase (BSAP) or PINP to estimate bone activity. Vascular calcification is checked with a simple chest X-ray or a CT scan that gives an Agatston score-higher scores mean more calcification.
Here’s what’s often missed: many patients with low PTH (<150 pg/mL) still have fragile bones. That’s called adynamic bone disease. It’s not rare-it affects half of dialysis patients. And it’s often caused by too much calcium-based binder or too much active vitamin D.
Treatment: It’s Not Just About Taking Pills
Treating CKD-MBD means balancing three things: lowering phosphate, fixing vitamin D, and controlling PTH-without making one problem worse.
Phosphate Control
Diet is step one. Most people with CKD need to limit phosphate to 800-1,000 mg per day. That means avoiding processed foods, colas, and dairy substitutes with added phosphate. But it’s nearly impossible to stay within limits without binders.
Phosphate binders stick to phosphate in your gut so it doesn’t get absorbed. Calcium-based binders (like calcium carbonate) are cheap and effective-but they add more calcium to your system, which can worsen calcification. Guidelines now limit them to 1,500 mg of elemental calcium per day.
Non-calcium binders like sevelamer or lanthanum are safer for arteries but cost more. Sevelamer has been shown to lower PTH and even slow artery hardening. Lanthanum is effective but can cause nausea.
Vitamin D: Nutritional vs. Active
Many patients are given active vitamin D (calcitriol or paricalcitol) to lower PTH. But here’s the catch: they raise calcium and phosphate. That’s why they’re only used when PTH is very high-above 500 pg/mL.
For most, the better choice is nutritional vitamin D (cholecalciferol). It’s safer, cheaper, and lowers mortality by 15%. It doesn’t spike calcium. It just helps your body make enough active vitamin D on its own, if the kidneys can still do a little work.
2024 guidelines now recommend checking 25(OH)D levels yearly starting at Stage 3 CKD. If it’s below 30 ng/mL, start cholecalciferol at 1,000-4,000 IU daily.
Controlling PTH
When PTH is sky-high (above 800 pg/mL), doctors turn to calcimimetics like cinacalcet or etelcalcetide. These drugs trick the parathyroid gland into thinking calcium levels are higher than they are-so it stops overproducing PTH.
Cinacalcet is taken daily. Etelcalcetide is injected three times a week during dialysis. Both lower PTH by 30-50%. They don’t raise calcium or phosphate, making them safer than active vitamin D.
But they’re not for everyone. If your PTH is low and your bone turnover is already slow (adynamic disease), these drugs can make it worse. That’s why PTH alone isn’t enough-you need to know your bone status.
What’s New in 2025?
Research is moving fast. Anti-sclerostin antibodies like romosozumab, which help build bone, are now in Phase 2 trials for CKD patients. Early results show a 30-40% increase in bone density without increasing fracture risk.
Scientists are also exploring Klotho protein replacement. In animal studies, adding Klotho cuts vascular calcification by 50-60% and improves bone strength. Human trials are expected by 2026.
And the biggest shift? Treatment is starting earlier. CKD-MBD doesn’t wait for dialysis. FGF23 rises as early as Stage 3. That’s why monitoring phosphate and vitamin D from the start-before bones break or arteries harden-is now the standard.
What You Can Do
If you have CKD, here’s what to ask your doctor:
- Can I get my phosphate, calcium, PTH, and vitamin D levels checked every 3-6 months?
- Am I on a calcium-based binder? Could I switch to sevelamer or lanthanum?
- Am I taking active vitamin D? Is my PTH really high enough to need it?
- Have I had a bone density scan? What’s my bone turnover status?
- Are my processed foods, sodas, or cheese substitutes adding hidden phosphate?
Don’t wait for a fracture or a heart attack to realize something’s wrong. CKD-MBD is silent until it’s too late. But with the right monitoring and adjustments, you can protect your bones, your heart, and your future.
Is CKD-MBD the same as osteoporosis?
No. Osteoporosis is about losing bone density with age. CKD-MBD is a systemic disorder caused by kidney failure that affects bone quality, mineral balance, and blood vessel health. People with CKD-MBD can have normal bone density but still break bones easily because their bone structure is weak or poorly formed.
Can I fix CKD-MBD with supplements alone?
No. While vitamin D supplements help, CKD-MBD requires a combination of diet, binders, medication, and dialysis adjustments. Taking extra calcium or vitamin D without medical supervision can worsen vascular calcification or cause dangerous spikes in phosphate or PTH.
Why is phosphate so dangerous in CKD?
High phosphate doesn’t just harm bones-it triggers calcification in arteries, heart valves, and lungs. It also increases FGF23, which damages the heart muscle and reduces vitamin D production. Each 1 mg/dL rise in phosphate increases death risk by 18%. It’s one of the strongest predictors of mortality in CKD.
Do all CKD patients need phosphate binders?
Not everyone. If your phosphate is within target and you’re on a strict low-phosphate diet, you may not need them early on. But by Stage 4 or 5, most patients do. The goal isn’t to bring phosphate to zero-it’s to keep it stable within the target range to avoid spikes that trigger calcification.
Can children with CKD develop CKD-MBD?
Yes-and it’s especially serious. In children, CKD-MBD disrupts bone growth and can cause stunted height. By Stage 5, many have height Z-scores 1.5 to 2.0 standard deviations below normal. Aggressive vitamin D and phosphate control are critical to allow normal growth.
What’s the biggest mistake doctors make treating CKD-MBD?
Treating one piece in isolation. Fixing PTH with active vitamin D without checking phosphate can cause dangerous calcification. Lowering phosphate with calcium binders without monitoring bone turnover can cause adynamic bone disease. CKD-MBD requires a system-wide approach-not a checklist of pills.
What Comes Next?
If you’re managing CKD, don’t assume your labs are fine just because they’re “in range.” Ask for a full mineral panel every six months. If your PTH is low but you’ve had a fracture, ask about bone turnover. If your phosphate is high despite binders, review your diet with a renal dietitian.
CKD-MBD is not inevitable. With early detection, smart choices, and coordinated care, you can slow the damage. Your bones and your heart will thank you.

Declan Flynn Fitness
December 1, 2025 AT 10:17Man, this is one of those topics that gets buried under all the flashy stuff in nephrology. But honestly? If you’re managing CKD, this is the silent killer no one talks about enough. I’ve seen patients with perfect eGFRs but shattered hips because their phosphate was creeping up for years. It’s not just about meds-it’s about diet, timing, and consistency. And yeah, vitamin D isn’t just a supplement you take and forget-it’s a hormone, and your kidneys are the factory that makes it work. Skip the basics, and your bones turn to dust while your arteries harden like old cement.
Also, FGF23? That’s the real villain. It’s not even on most patient’s radar. But if you’re tracking phosphate and PTH, you’re already seeing FGF23’s shadow. Early Stage 3 is when you need to act-not when you’re on dialysis.
Michelle Smyth
December 2, 2025 AT 18:52How quaint. Another clinical pamphlet dressed up as existential wisdom. The entire paradigm of CKD-MBD is a construct of pharmaceutical incentives masked as pathophysiology. Phosphate binders? Vitamin D analogs? All of it’s a Rube Goldberg machine designed to keep the nephrology-industrial complex solvent. The real issue? We’ve medicalized a natural consequence of metabolic decay. The body isn’t ‘dysfunctional’-it’s adapting. We’re just too arrogant to admit we can’t fix what evolution didn’t intend us to survive.
Patrick Smyth
December 3, 2025 AT 23:32I lost my mum to this. She was 68, went in for a hip fracture, and they found her arteries were basically lined with rock. They told us it was ‘just kidney disease’-but it wasn’t just that. It was the silence. No one warned us. No one said, ‘Your mom’s bones are turning to powder and her heart is calcifying like a fossil.’ I sat there in that office and cried because they gave me a pamphlet and a number to call. That’s not care. That’s negligence wrapped in jargon.
Louise Girvan
December 4, 2025 AT 12:44They’re lying. They always lie. The FDA, the pharma giants, the nephrologists-they all know phosphate isn’t the problem. It’s the fluoridated water. The aluminum in antacids. The glyphosate in your oat milk. They’re poisoning you slowly. And then they sell you binders to ‘fix’ it. But the binders? They’re just more toxins. You’re being turned into a lab rat. Check your tap water. Check your supplements. They’re not helping. They’re hiding.
soorya Raju
December 5, 2025 AT 21:19bro this is wild but like… what if the real villain is not phosphate but… capitalism? like why do we even have dialysis centers in the first place? if we just ate real food and stopped drinking soda and took vitamin d from the sun like our ancestors did, would we even need this? also i think the pth thing is just your body screaming for more sunlight and less sugar. my cousin in delhi, no meds, no binders, just millet and chai and walks at dawn-his numbers are better than my nephrologist’s.
Dennis Jesuyon Balogun
December 6, 2025 AT 06:18Let me speak plainly: this isn’t just a medical issue-it’s a spiritual one. The body is not a machine to be fixed. It’s a sacred vessel that reflects the neglect we inflict upon it. We poison our soil, our water, our diets-and then we marvel when our kidneys fail. We treat symptoms like enemies, not signals. CKD-MBD is the body’s last cry before surrender. We need humility, not algorithms. We need ancestral wisdom, not lab ranges. Vitamin D isn’t a pill-it’s a relationship with the sun. PTH isn’t a hormone-it’s your soul’s protest against systemic betrayal.
And to those who say ‘it’s just biology’-you’re wrong. Biology is politics. The body remembers what the system forgets.
Grant Hurley
December 7, 2025 AT 15:52big thanks for laying this out so clear. i’ve got a buddy on dialysis and i finally get why he’s always so tired and why his bones hurt even though he’s not old. i started helping him track his food-cut out the processed cheese, swapped soda for sparkling water, and he’s already feeling better. also, he’s taking his vit d with dinner now instead of breakfast-small change, but his levels are creeping up. if you’re reading this and you’re in stage 3 or 4-don’t wait. start now. your heart will thank you.
Lucinda Bresnehan
December 9, 2025 AT 03:04oh my gosh this is so important!! i just found out my mom has stage 3 and she’s been eating tons of cheese and soda because she thinks ‘it’s not that bad yet’… i’m gonna print this out and hand it to her with a cup of chamomile tea and hug her. i didn’t realize the bone thing was so sneaky. also, vit d levels under 20? that’s basically a national crisis in the US. we’re all inside all day and then wonder why we’re sick. 🙏
Shannon Gabrielle
December 9, 2025 AT 21:07Wow. Another overhyped medical myth. You’re telling me that after centuries of human evolution, we suddenly need pills and binders to survive? Pathetic. The only thing that’s broken is the medical system’s obsession with turning every biological process into a profit center. Bone density scans? Agatston scores? Please. Your body knows what to do. You just need to stop poisoning it with pharmaceuticals and processed food. Simple. Done. No more tests. No more meds. Just eat real food and shut up.
Jeremy Butler
December 11, 2025 AT 03:15One must interrogate the epistemological foundations of the CKD-MBD construct. The reductionist paradigm that isolates phosphate, PTH, and vitamin D as discrete variables obscures the ontological unity of renal homeostasis. The body does not suffer from ‘disorder’-it responds to systemic dissonance. To quantify these biomarkers as targets is to commit the reification fallacy. The therapeutic imperative, therefore, must transcend pharmacological intervention and return to the Aristotelian notion of eudaimonia: the cultivation of a life in harmony with nature’s rhythms.
Courtney Co
December 13, 2025 AT 00:17do you think… i mean… what if this is why i’ve been having so much joint pain? i’ve been on lisinopril for years and i never thought about my bones… i’m scared now. i’m gonna call my doctor tomorrow. i hope it’s not too late. i just want to be able to play with my niece without wincing. please tell me i’m not too late.
Eric Vlach
December 13, 2025 AT 14:48Just a heads up for anyone reading-bone biopsy isn’t always needed. If your PTH is over 600 and your BSAP is sky-high, you’ve got high turnover. If PTH is low and BSAP is low? That’s adynamic bone disease. And yeah, that’s dangerous too. But here’s the kicker: you can’t fix it with more vitamin D if you’re already overloaded. That’s why some docs miss it. They think ‘low PTH = good’. Nope. It’s a trap. Ask for BSAP or PINP. If they don’t know what you’re talking about, find a new doc.
Grant Hurley
December 14, 2025 AT 03:58^^^ YES. My buddy’s doc did that. They thought his PTH was ‘too low’ so they stopped his vitamin D. He got worse. Then they checked BSAP and realized his bones were basically sleeping. That’s when they switched to a different calcitriol and started a tiny bit of teriparatide. It’s wild how much one number can change everything. Don’t let them treat your PTH like a light switch.