Pediatric Sleep Apnea: When Tonsils, Adenoids, and CPAP Are the Answer
 Jan, 10 2026
Jan, 10 2026
What Is Pediatric Sleep Apnea?
When a child stops breathing briefly-multiple times-during sleep, it’s not just snoring. It’s pediatric obstructive sleep apnea (OSA), a real and often overlooked condition. Unlike adults, kids with OSA don’t always wake up gasping. Instead, they might toss and turn, sweat heavily at night, breathe through their mouths, or seem overly tired during the day-even if they slept "all night."
This isn’t normal. About 1 to 5 out of every 100 children have it, and it hits hardest between ages 2 and 6. That’s when their tonsils and adenoids are biggest relative to their small airways. When those tissues swell, they block the path to the lungs. Every time the child tries to breathe, the airway collapses. Their body struggles. Their oxygen drops. Their brain wakes them up-just enough to restart breathing, but not enough for real rest.
Why Tonsils and Adenoids Are the Main Culprits
Most kids with sleep apnea don’t have it because they’re overweight or have a narrow jaw. They have it because their tonsils and adenoids are too big. These are not just "glands"-they’re lymphatic tissues meant to fight germs. But in many children, they grow too large and stay that way, turning into physical roadblocks.
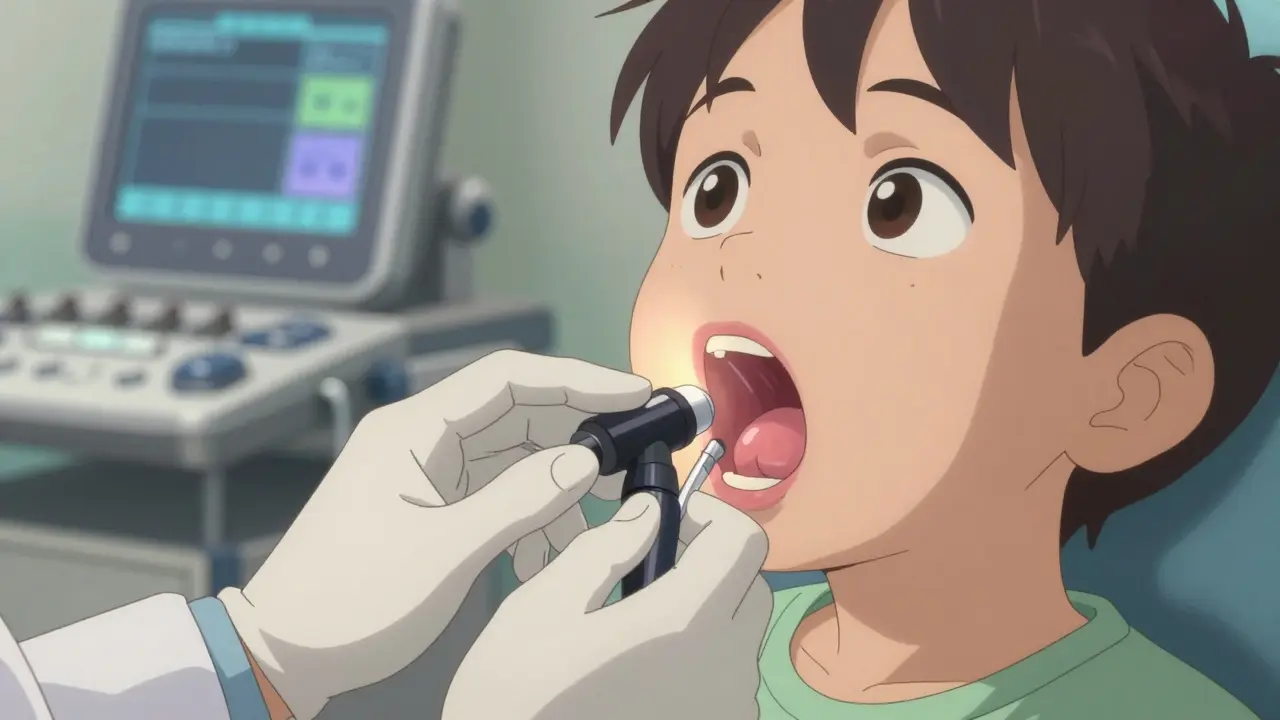
Doctors don’t just guess. They look. A simple exam can show tonsils that are Grade 3 or 4-almost touching each other in the back of the throat. The adenoid, hidden behind the nose, can be checked with a small camera or X-ray. When both are enlarged, the problem multiplies. Even if one looks bigger, removing just one isn’t enough. Studies show OSA comes back if both aren’t taken out.
That’s why the American Academy of Pediatrics says: for healthy kids with clear signs of enlarged tonsils and adenoids, surgery is the first step. Not medicine. Not sleep position tricks. Surgery.
Adenotonsillectomy: The Go-To Solution
Removing both tonsils and adenoids-called adenotonsillectomy-is the most common treatment. It’s done under general anesthesia, takes about 30 minutes, and most kids go home the same day. Recovery takes about a week to two. They need soft foods, lots of fluids, and quiet time.
Success rates? Between 70% and 80% in kids without other health issues. That means most stop snoring, sleep through the night, and wake up alert. Their behavior improves. Their grades get better. Their heart doesn’t have to work so hard.
But it’s not perfect. About 1 in 5 kids still have sleep apnea after surgery. Why? Maybe their airway is narrow for other reasons-like obesity, a small jaw, or muscle tone issues. Or maybe the adenoid didn’t get fully removed. That’s why doctors recommend a follow-up sleep study 2 to 3 months later. If the problem lingers, they don’t just shrug. They look for other answers.
What If Surgery Doesn’t Work-or Isn’t an Option?
Not every child can have surgery. Some have bleeding disorders. Others have Down syndrome, cerebral palsy, or other neuromuscular conditions. Some are too young. Others have had bad reactions to anesthesia. For them, CPAP is the next best thing.
CPAP stands for continuous positive airway pressure. It’s a small machine that blows gentle, steady air through a mask worn over the nose-or nose and mouth-while the child sleeps. The air keeps the throat open. No collapse. No pauses. No oxygen drops.
The pressure is set just right: usually between 5 and 12 cm H2O. Too low? It won’t help. Too high? It hurts. That’s why every child needs a titration sleep study first. They spend one night hooked up to sensors while the machine adjusts pressure automatically until every breath is smooth.
When used correctly, CPAP works in 85% to 95% of cases. It’s not a cure, but it’s a powerful tool. And it’s not just for kids who can’t have surgery. It’s also used when surgery doesn’t fix everything.
Why Kids Struggle With CPAP-and How to Help
Here’s the hard truth: kids hate CPAP masks. At first. They feel claustrophobic. The tubing tangles. The mask leaks. They pull it off in the middle of the night. Studies show 30% to 50% of kids give up or use it inconsistently.
But it’s not hopeless. The key is patience and smart adaptation. Pediatric sleep centers don’t hand out adult masks. They use smaller, softer designs made for kids-like nasal pillows or silicone masks that hug the bridge of the nose. Some even come in fun colors or with favorite cartoon characters.
Parents are taught to introduce it slowly. First, let the child hold the mask. Then wear it while watching TV. Then with the machine off. Then with low air pressure. Then at bedtime. It can take weeks. But once they get used to it, many kids say they sleep better without the snoring.
And masks need to be replaced. Kids grow fast. A mask that fits at age 4 won’t fit at age 6. Most clinics recommend checking fit every 6 to 12 months. If the mask leaks or leaves red marks, it’s time for a new one.
Other Treatments: What Else Can Help?
Surgery and CPAP aren’t the only options. For mild cases, doctors sometimes try nasal steroid sprays-like fluticasone. These reduce swelling in the adenoids and tonsils. It takes 3 to 6 months to see results, but for kids with allergies or mild OSA, it can cut symptoms in half.
Another option is rapid maxillary expansion. This is an orthodontic device worn at night that slowly widens the upper jaw. It works best in kids with narrow palates, which is common in mouth-breathers. Over 6 to 12 months, it can open up the airway by a few millimeters-and that’s enough to make a big difference. Success rates? Around 60% to 70%.
And then there’s montelukast. It’s a pill usually given for asthma, but research shows it can shrink lymphoid tissue by blocking inflammation. It’s not a first-line treatment, but for kids who can’t have surgery and won’t use CPAP, it’s a bridge. It takes months to work, and it’s not a cure-but it can help.

When to Worry-and When to Act
Not every snorer has sleep apnea. But if your child does all of these, it’s time to talk to a doctor:
- Snoring louder than talking, three or more nights a week
- Stopping breathing during sleep, even briefly
- Restless sleep, sweating, or sleeping in weird positions
- Daytime sleepiness, trouble concentrating, or behavioral issues
- Mouth breathing, dry mouth, or frequent ear infections
Don’t wait. Untreated OSA can lead to learning problems, high blood pressure, and even heart strain. Kids with severe OSA can have 15 to 30 breathing pauses every hour. That’s not normal sleep. That’s constant stress on their body.
And if your child had surgery but still snores or acts tired? Go back. The problem might not be gone. CPAP might be needed. Or maybe they need a different kind of evaluation-like a sleep endoscopy, where a tiny camera watches the airway while the child is asleep on medicine.
What’s Next for Pediatric Sleep Apnea?
Science is moving fast. New techniques like partial tonsillectomy-where only part of the tonsil is removed-are gaining ground. They mean less pain, faster recovery, and fewer complications. But only a few centers in the U.S. and Europe do them yet.
And there’s hypoglossal nerve stimulation-a tiny implant that nudges the tongue forward during sleep to keep the airway open. It’s FDA-approved for kids in rare cases, but still very new.
Still, the basics haven’t changed. For most kids, removing the tonsils and adenoids fixes the problem. For others, CPAP is the lifeline. The goal isn’t just to stop snoring. It’s to let a child sleep deeply, grow strong, and learn without fatigue dragging them down.
Final Thought: It’s Not Just About Breathing
Every child deserves restful sleep. Sleep apnea isn’t a phase. It’s a medical issue with real consequences. The good news? We know how to fix it. We just need to look for it.
If your child snores, struggles to wake up, or seems "off" during the day-ask. Get them checked. Don’t assume it’s just growing pains. Their brain, their heart, their future-they’re all counting on you to notice.

Eileen Reilly
January 12, 2026 AT 05:03Cecelia Alta
January 12, 2026 AT 17:49Monica Puglia
January 13, 2026 AT 18:52Alex Fortwengler
January 14, 2026 AT 10:18jordan shiyangeni
January 15, 2026 AT 15:25steve ker
January 16, 2026 AT 05:52Abner San Diego
January 17, 2026 AT 20:39gary ysturiz
January 18, 2026 AT 23:58Jessica Bnouzalim
January 19, 2026 AT 13:14TiM Vince
January 21, 2026 AT 04:20