Proton Pump Inhibitors: Long-Term Risks and When to Stop
 Feb, 7 2026
Feb, 7 2026
Proton pump inhibitors, or PPIs, are among the most commonly prescribed medications in the world. If you’ve ever had heartburn, acid reflux, or a stomach ulcer, chances are you’ve been on one. Brands like Prilosec, Nexium, and Prevacid sound familiar because they’re everywhere - in medicine cabinets, pharmacy shelves, and even sold over the counter. But here’s the thing: many people take them for months, even years, without ever asking if they still need them. And that’s where the real problem starts.
What PPIs Do - and Why They Work So Well
PPIs work by shutting down the final step of acid production in your stomach. They block the proton pump - a tiny engine in the stomach lining that pumps acid out. No pump, no acid. That’s why they’re so effective. For someone with severe GERD or an ulcer, PPIs can be life-changing. Healing rates for erosive esophagitis? Over 90%. That’s why doctors reach for them first.
But they’re not quick fixes. Unlike antacids or H2 blockers like Pepcid, PPIs take 1 to 4 days to kick in. That’s why they’re meant to be taken before meals, not after symptoms hit. And they’re not meant to be taken forever. The FDA says over-the-counter PPIs should only be used for 14 days at a time, and no more than once every three months. Yet, studies show nearly 25% of people keep using them beyond that - often without ever talking to a doctor.
The Hidden Risks of Long-Term Use
Just because a drug is widely used doesn’t mean it’s risk-free. The FDA has issued seven safety warnings about PPIs since 2010. Some of these risks are rare. Others are more common than you’d think.
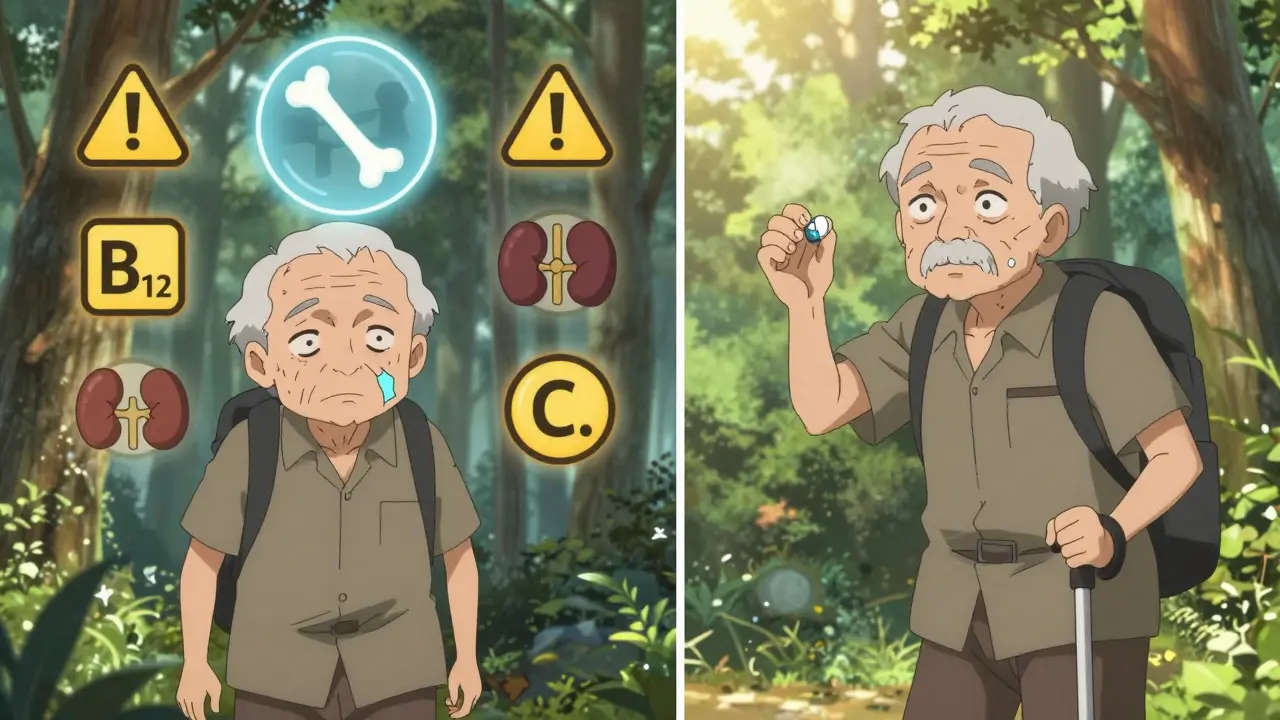
- Fractures: Long-term PPI use (4+ years) is linked to a 42% higher risk of hip fractures. Why? Acid suppression reduces calcium absorption. Women on PPIs for 6-8 years had a 55% higher fracture risk in one study. The good news? Risk drops back to normal after stopping.
- Magnesium deficiency: This one’s serious but rare. Affects about 0.5-1% of long-term users. Symptoms? Muscle cramps, tremors, irregular heartbeat. The FDA now says doctors should check magnesium levels if you’ve been on PPIs for over a year.
- Vitamin B12 deficiency: Up to 15% of people on PPIs for more than two years develop low B12. Why? Acid helps break down food to release B12. Less acid = less absorption. Fatigue, numbness, memory issues - all possible signs.
- C. diff infection: PPIs raise your risk of this dangerous gut infection by nearly 2x. It’s especially dangerous in hospitals or for older adults. The FDA calls this one a confirmed risk.
- Acute interstitial nephritis: A rare but serious kidney inflammation. The FDA flagged this in 2016. While most cases reverse after stopping PPIs, some lead to lasting kidney damage.
Then there are the rumors - dementia, heart disease, kidney failure. Some studies link PPIs to these, but the evidence is shaky. Experts like Dr. William Ravich from Yale point out: many of these studies didn’t control for other health problems. People on long-term PPIs are often older, sicker, or on other meds. It’s hard to say if the PPI caused the issue - or if the underlying illness did.
Why So Many People Are Taking PPIs Unnecessarily
Here’s the uncomfortable truth: up to 70% of PPI prescriptions have no clear medical reason. You don’t need a PPI for occasional heartburn. You don’t need one for mild indigestion. And you definitely don’t need one for more than 8 weeks unless you have a confirmed diagnosis like Barrett’s esophagus or severe ulcers.
So why are so many people on them? For starters, doctors sometimes prescribe them “just in case.” Patients ask for them because they’ve seen ads. And once you start, it’s easy to keep going. The problem? PPIs don’t cure the root cause. They mask it. Lifestyle factors - obesity, late-night eating, alcohol, smoking - are often the real culprits. But those are harder to fix than popping a pill.
In the U.S. alone, inappropriate PPI use costs over $12 billion a year. That’s billions spent on drugs that aren’t helping - and might be harming.
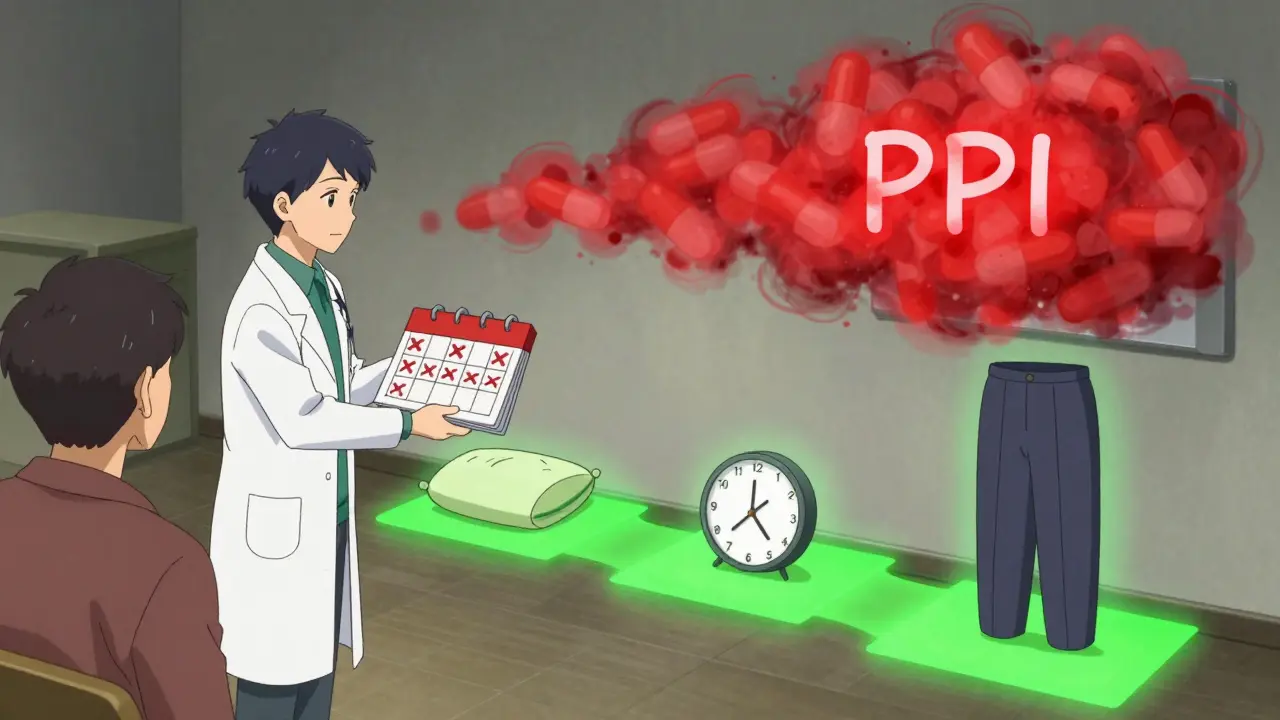
When and How to Stop PPIs
If you’ve been on a PPI for more than 4-8 weeks - especially for mild symptoms - it’s time to talk to your doctor about stopping. But don’t quit cold turkey. That’s a recipe for disaster.
Stopping suddenly can cause rebound acid hypersecretion. That’s when your stomach goes into overdrive, producing even more acid than before. About 40-80% of long-term users experience this. Symptoms? Worse heartburn than ever. It can last for weeks. People think the PPI stopped working - when really, their body overreacted.
Here’s how to stop safely:
- Reduce the dose: Cut your daily dose in half. If you’re taking 40mg, go to 20mg. Do this every 1-2 weeks.
- Switch to on-demand use: Once you’re on a lower dose, only take it when you feel symptoms - not daily.
- Try alternatives: Use antacids (Tums, Rolaids) or H2 blockers (famotidine) for occasional relief. They’re safe for short-term use.
- Give it time: It can take 2-4 weeks for your stomach to reset. Stick with the plan.
- Track symptoms: Keep a journal. What you eat, when you feel acid, how you feel after meals. This helps you and your doctor spot triggers.
Some people can stop completely. Others need to stay on a low dose. The goal isn’t to eliminate PPIs forever - it’s to use them only when truly needed.
What to Do Instead
Stopping PPIs doesn’t mean going back to suffering. Lifestyle changes can be just as powerful - and safer long-term.
- Eat earlier: Finish meals at least 3 hours before lying down. Gravity helps keep acid down.
- Watch your triggers: Coffee, chocolate, spicy food, citrus, alcohol, and fatty meals are common offenders.
- Loosen your belt: Tight clothes increase pressure on your stomach. A simple change - but it helps.
- Elevate your head: Use a wedge pillow or raise the head of your bed by 6 inches. It’s cheap, simple, and effective.
- Manage weight: Even a 10% weight loss can cut reflux symptoms in half.
- Quit smoking: Smoking relaxes the valve between your stomach and esophagus. No surprise it makes reflux worse.
These aren’t just "tips." They’re backed by studies. In fact, the American College of Gastroenterology says lifestyle changes should come before long-term PPI use - not after.
Who Should Definitely Keep Taking PPIs
Not everyone should stop. Some people need PPIs to avoid serious complications:
- People with Barrett’s esophagus (a precancerous condition)
- Those with recurrent bleeding ulcers
- Patients on long-term NSAIDs (like ibuprofen or aspirin) who have a history of ulcers
- Anyone with confirmed severe erosive esophagitis
If you fall into one of these groups, don’t stop without talking to your doctor. The risks of stopping outweigh the risks of continuing - for you.
The Bottom Line
PPIs are powerful tools - but they’re not harmless. They work too well, which is why so many people stay on them longer than they should. The truth? Most people don’t need daily PPIs. Not for occasional heartburn. Not for mild indigestion. Not for "just in case." The goal isn’t to fear PPIs. It’s to use them wisely. If you’ve been on one for more than 8 weeks, ask your doctor: "Do I still need this?" And if you’re using OTC PPIs regularly, ask yourself: "Why am I still taking this?" Your stomach doesn’t need constant suppression. It needs balance. And sometimes, that means stepping off the pill - slowly, safely, and with a plan.
Can I stop PPIs cold turkey?
No. Stopping PPIs suddenly can cause severe rebound acid reflux, making symptoms worse than before. Up to 80% of long-term users experience this. Always taper down slowly under medical guidance - reduce dose by half every 1-2 weeks, then switch to on-demand use before stopping completely.
How long is too long to be on a PPI?
For most conditions like GERD or mild ulcers, PPIs should be used for only 4-8 weeks. If symptoms return after stopping, you may need a short course again. If you’ve been on PPIs for more than 3 months without a clear diagnosis - especially for dyspepsia - it’s time to reassess. Long-term use (over a year) increases risk of fractures, low magnesium, and B12 deficiency.
Are over-the-counter PPIs safer than prescription ones?
No. OTC PPIs have the same active ingredients and risks as prescription versions. The only difference is dose - OTC is usually 20mg, while prescriptions can go up to 40mg. The FDA limits OTC use to 14 days every 3 months because long-term self-medication leads to overuse and hidden side effects.
Do PPIs cause stomach cancer?
No. High-quality studies have not found a link between PPIs and stomach cancer. Some early studies suggested a connection, but they didn’t account for H. pylori infection - a known cause of stomach cancer. In fact, PPIs are often used to treat H. pylori-related ulcers. The real concern is long-term use in people with untreated Barrett’s esophagus, not cancer caused by the drug itself.
Can I replace PPIs with natural remedies?
Natural remedies like ginger, aloe vera, or apple cider vinegar aren’t proven to replace PPIs for moderate to severe reflux. They might help mild symptoms, but they don’t reduce acid production like PPIs do. Lifestyle changes - eating earlier, losing weight, elevating your head - are far more effective than unproven supplements. Always consult your doctor before switching from medication to unverified remedies.
