Respiratory Infections and COVID-19: How Blood Thinners Interact with Antiviral Treatments
 Dec, 12 2025
Dec, 12 2025
Blood Thinner & COVID-19 Drug Interaction Checker
Check how your blood thinner interacts with COVID-19 treatments. Based on current guidelines for warfarin, rivaroxaban, apixaban, dabigatran, and other anticoagulants.
Important: This tool provides general guidance based on current medical knowledge. Always consult with your healthcare provider before making changes to your medications.
When you're on a blood thinner like rivaroxaban or warfarin and catch a bad respiratory infection-especially COVID-19-the risk isn't just the virus itself. It's what happens when your antiviral meds collide with your anticoagulant. These interactions can turn a manageable condition into a life-threatening one. One patient in South Africa was admitted with internal bleeding after taking Paxlovid while still on full-dose apixaban. Another had a stroke because her dabigatran levels dropped too low after starting dexamethasone. These aren’t rare cases. They’re happening in hospitals and homes every day.
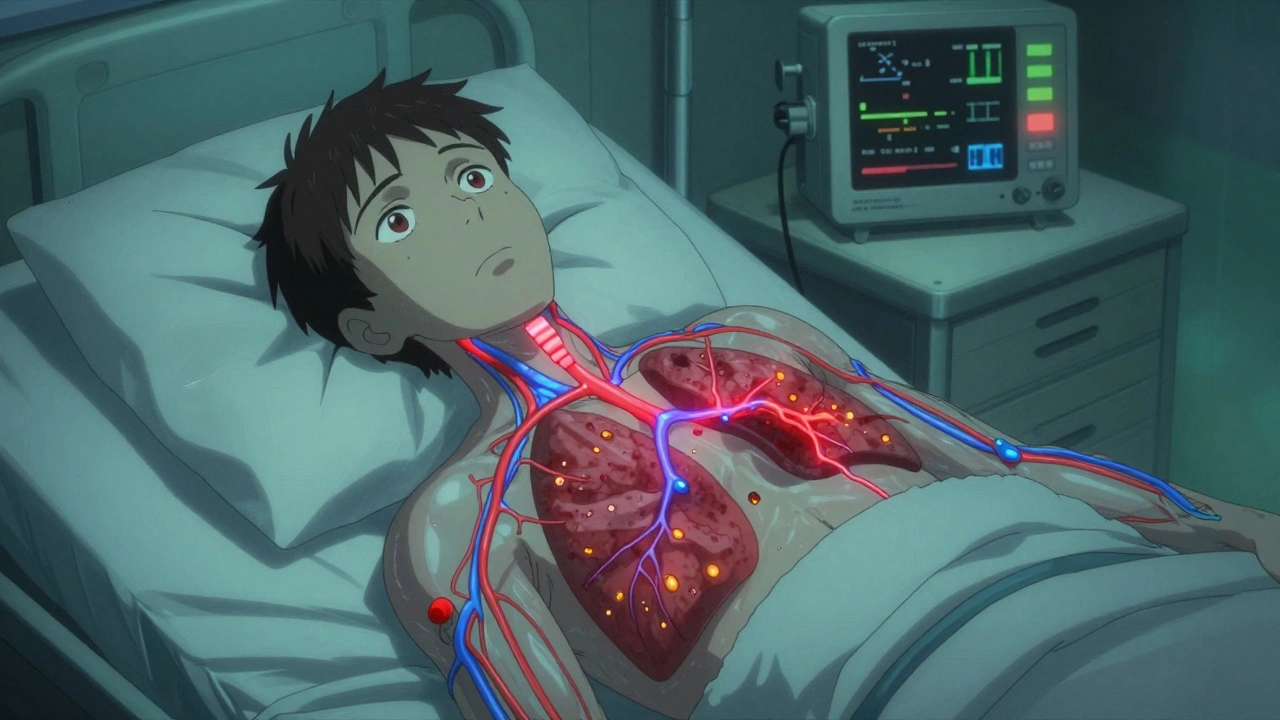
Why COVID-19 Makes Blood Clots More Likely
COVID-19 doesn’t just attack your lungs. It triggers your body’s clotting system to go into overdrive. In severe cases, up to 70% of critically ill patients show signs of tiny clots blocking blood vessels in the lungs. This isn’t just a side effect-it’s a core part of how the disease kills. The inflammation from the virus turns your blood into something thicker, stickier, and more likely to clot. That’s why doctors started giving anticoagulants to hospitalized patients early in the pandemic. The American Society of Hematology confirmed in 2021 that therapeutic-intensity anticoagulation (higher doses) works better than standard prophylactic doses for these patients.
But here’s the catch: once you leave the hospital, your blood doesn’t suddenly return to normal. Studies show that 65% of patients still have elevated D-dimer levels-signs of ongoing clotting activity-for two to three weeks after discharge. That means the danger doesn’t end when you stop feeling sick. You’re still at risk.
How Antivirals Like Paxlovid Disrupt Blood Thinners
Paxlovid (nirmatrelvir-ritonavir) is one of the most effective antivirals for early COVID-19 treatment. But ritonavir, one of its components, is a powerful inhibitor of CYP3A4 and P-glycoprotein-two systems your body uses to break down and clear many drugs, including direct oral anticoagulants (DOACs). When these systems are blocked, your blood thinner builds up in your system. That’s like doubling or tripling your dose without knowing it.
Studies show that patients on DOACs who take Paxlovid can see their drug levels spike by 300-500%. That leads to major bleeding: gastrointestinal, brain, or internal. The FDA reported 147 cases of serious bleeding between January 2022 and June 2023 linked to this interaction. One Reddit user shared how their neighbor ended up in the ER after continuing rivaroxaban during Paxlovid treatment. He needed two units of blood transfusions.
On the flip side, dexamethasone-a steroid used to reduce lung inflammation in severe COVID-19-is a strong inducer of CYP3A4 and P-gp. It speeds up how fast your body clears DOACs. One study found it can reduce rivaroxaban levels by up to 50%. That means your blood thinner stops working. You’re unprotected. Clots form. You might not even know until it’s too late.
Warfarin vs. DOACs: Different Risks, Different Rules
Warfarin works differently than DOACs. It’s older, slower, and requires regular INR blood tests. But it’s not safer during COVID-19. While warfarin doesn’t rely as heavily on CYP3A4, it’s still affected by other drugs. Azvudine, an antiviral used in some countries, can raise INR levels. Dexamethasone can lower them. One case study showed a 70-year-old man’s INR jumping from 2.5 to 3.8 after starting both drugs-putting him at high risk for bleeding.
DOACs like apixaban, rivaroxaban, dabigatran, and edoxaban are more convenient-no weekly blood tests-but they’re far more sensitive to drug interactions. The problem? Guidelines aren’t consistent. The U.S. says: avoid dabigatran with Paxlovid if your kidney function is low. Europe says: you can use it, but cut the dose. For rivaroxaban, the EMA recommends halving the dose. The FDA says: don’t use it at all during Paxlovid treatment. This confusion leaves doctors and patients guessing.

Real-World Chaos in Pharmacies and Clinics
During the height of the pandemic, anticoagulation clinics saw a 20% drop in patients keeping their INR in the safe range. Why? No one could get to the lab. Telehealth didn’t fully replace blood draws. At the same time, emergency visits for anticoagulant problems rose by 37% at Mayo Clinic. Over 28% of those were due to interactions with COVID-19 drugs.
Community pharmacists were on the front lines. A 2022 survey found that 63% of U.S. outpatient pharmacists dealt with at least one dangerous anticoagulant-COVID drug interaction every month. Dabigatran and Paxlovid made up 42% of those cases. One pharmacist in Atlanta told me she had to call three different doctors before someone agreed to pause a patient’s rivaroxaban. The patient was 78, had atrial fibrillation, and was on Medicare. No one wanted to take responsibility.
How to Stay Safe: Clear Protocols for Patients and Providers
There’s no one-size-fits-all answer, but here’s what works based on current guidelines:
- If you’re on apixaban or rivaroxaban and need Paxlovid: Stop the DOAC for the full 5-day course. Restart it 2 days after the last Paxlovid dose. If you’re at high risk for clots (CHA₂DS₂-VASc score ≥3), ask about bridging with daily enoxaparin injections during those 5 days.
- If you’re on dabigatran: If your kidney function is normal (CrCl ≥50 mL/min), reduce your dose to 75 mg twice daily during Paxlovid treatment. Take it at least 12 hours before or after Paxlovid. If your kidneys are impaired, avoid it entirely.
- If you’re on warfarin: You can keep taking it, but check your INR every 2-3 days during and after Paxlovid treatment. Dexamethasone can make your INR drop fast. Azvudine can make it spike.
- Always check before starting any new medication: Use the Liverpool COVID-19 Drug Interactions website. It’s updated daily and has processed over 1.2 million queries since 2020. Type in your meds and the new drug-it tells you exactly what to do.
Monitoring matters. If you’re on a DOAC, anti-Xa levels should be checked every 2-3 days during overlapping treatment. Normal range is 50-200 ng/mL. If you’re on warfarin, INR should stay between 2.0 and 3.0. Anything outside that range needs immediate attention.
What’s Coming Next: Better Drugs, Better Tools
Pharmaceutical companies are already working on solutions. Pfizer’s next antiviral, PF-07817883, is in Phase 2 trials and shows almost no CYP3A4 inhibition. That means it won’t interfere with blood thinners. If it works, it could replace Paxlovid in the next few years.
Technology is helping too. A 2023 study in Nature Medicine built a machine learning model that predicts interaction severity with 89.4% accuracy. It uses your age, kidney function, current meds, and infection severity to tell you if you’re at high, medium, or low risk. Hospitals in the U.S. are starting to integrate this into their EHR systems.
But the biggest cost isn’t just medical-it’s financial. The Institute for Clinical and Economic Review estimates that managing these interactions will cost the U.S. $1.2 billion annually by 2025. That’s because of hospitalizations, emergency visits, blood transfusions, and lost work time. The real cost? The fear patients feel when they don’t know if their pill is safe to take.
What You Should Do Right Now
If you’re on a blood thinner and get sick with a respiratory infection:
- Don’t stop or change your anticoagulant on your own.
- Tell your doctor or pharmacist exactly what you’re taking-including vitamins, supplements, and over-the-counter meds.
- Ask: "Is this antiviral safe with my blood thinner?" If they don’t know, ask them to check the Liverpool website.
- Request a blood test (INR or anti-Xa) if you’re on therapy during treatment.
- If you’re hospitalized, make sure your anticoagulant plan is reviewed daily.
COVID-19 changed how we treat blood clots. But it also exposed how little we knew about how drugs interact in real-world illness. The science is catching up. The protocols are improving. But for now, the safest thing you can do is be informed, ask questions, and never assume your meds are safe together.
Can I keep taking my blood thinner if I get COVID-19?
It depends on the medication and how sick you are. If you’re on warfarin, you can usually continue with close INR monitoring. If you’re on a DOAC like rivaroxaban or apixaban and are taking Paxlovid, you should pause it during the 5-day treatment and restart 2 days after. If you’re hospitalized with severe COVID-19, you may need therapeutic anticoagulation-your doctor will decide. Never stop or change your dose without medical advice.
Does dexamethasone make blood thinners less effective?
Yes. Dexamethasone speeds up how quickly your body breaks down DOACs like rivaroxaban and apixaban. Studies show it can reduce their levels by up to 50%, which means you’re not protected from clots anymore. If you’re on a DOAC and prescribed dexamethasone, your doctor should check your anti-Xa levels or consider switching to a different anticoagulant like enoxaparin during treatment.
Is Paxlovid safe with warfarin?
Paxlovid can be used with warfarin, but it requires close monitoring. Ritonavir in Paxlovid doesn’t strongly affect warfarin’s metabolism, but other drugs you’re taking might. Your INR could go up or down unpredictably. Check your INR every 2-3 days during and after Paxlovid treatment. If your INR goes above 4.0, contact your doctor immediately.
What should I do if I experience bleeding while on a blood thinner and COVID-19 meds?
Seek emergency care immediately. Signs include unusual bruising, nosebleeds that won’t stop, blood in urine or stool, vomiting blood, or severe headaches. Tell the ER staff exactly what medications you’re taking-including Paxlovid, dexamethasone, or any antiviral. Bring a list of all your drugs. Time matters-bleeding from anticoagulant interactions can be life-threatening if not treated quickly.
Are there any apps or tools to check for drug interactions?
Yes. The Liverpool COVID-19 Drug Interactions website (liverpoolcovid19.com) is the most trusted free tool. It’s updated daily and includes over 300 drugs. Type in your anticoagulant and the new medication-it tells you if it’s safe, what to do, and whether to adjust the dose. Many hospitals and pharmacies now use it as their standard reference. Don’t rely on generic drug interaction checkers-they often miss COVID-specific risks.
Final Thoughts
The pandemic showed us that even simple decisions-like taking a pill for a cold-can have deadly consequences when you’re on a blood thinner. We now know more than ever about how these drugs interact. The tools are here. The guidelines exist. But the biggest barrier isn’t science-it’s communication. Patients don’t always tell their doctors about every pill they take. Pharmacists don’t always get the full picture. Doctors are overwhelmed. The solution isn’t a new drug. It’s asking the right questions, checking the right resources, and never assuming safety.

Cole Newman
December 12, 2025 AT 13:30Emily Haworth
December 13, 2025 AT 16:37Tom Zerkoff
December 14, 2025 AT 19:19Yatendra S
December 16, 2025 AT 14:45Himmat Singh
December 17, 2025 AT 03:29nithin Kuntumadugu
December 17, 2025 AT 18:48John Fred
December 17, 2025 AT 20:29Harriet Wollaston
December 18, 2025 AT 06:52Lauren Scrima
December 20, 2025 AT 02:02sharon soila
December 21, 2025 AT 06:54nina nakamura
December 22, 2025 AT 14:08Hamza Laassili
December 23, 2025 AT 09:23Rawlson King
December 23, 2025 AT 22:35