SSRIs and Opioids: Understanding Serotonin Syndrome Risk and How to Prevent It
 Dec, 26 2025
Dec, 26 2025
SSRI-Opioid Risk Assessment Tool
Combining SSRIs and opioids might seem like a harmless mix-after all, one treats depression and the other relieves pain. But for thousands of people, this combination is a quiet ticking clock. Serotonin syndrome isn’t rare. It’s not theoretical. It’s happening in hospitals, ERs, and homes right now, often mistaken for something else entirely. And the most dangerous part? Many people don’t even know they’re at risk.
What Exactly Is Serotonin Syndrome?
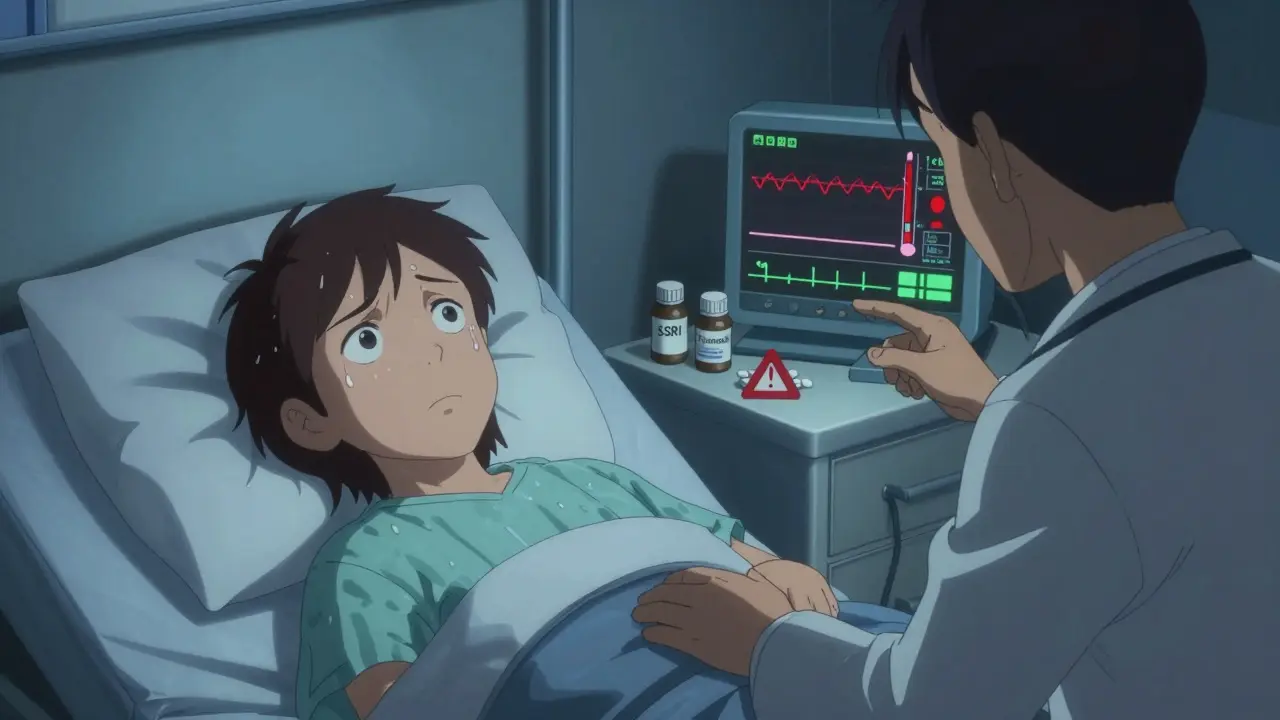
Serotonin syndrome is a dangerous overstimulation of your nervous system caused by too much serotonin. It doesn’t happen from taking one drug alone. It happens when two or more drugs that boost serotonin levels are used together. SSRIs like sertraline, fluoxetine, and escitalopram increase serotonin by blocking its reabsorption. Some opioids-especially tramadol, methadone, and pethidine-do the same thing. When they meet, serotonin piles up in your brain and nerves faster than your body can clear it.The result? Your body goes into overdrive. You might start shivering uncontrollably, your heart races, your muscles twitch, and you break out in sweat even when it’s cool. In severe cases, your temperature can spike past 41°C (106°F), your muscles lock up, and seizures can occur. Without quick treatment, serotonin syndrome can be fatal. About 10% of severe cases end in death if not recognized in time.
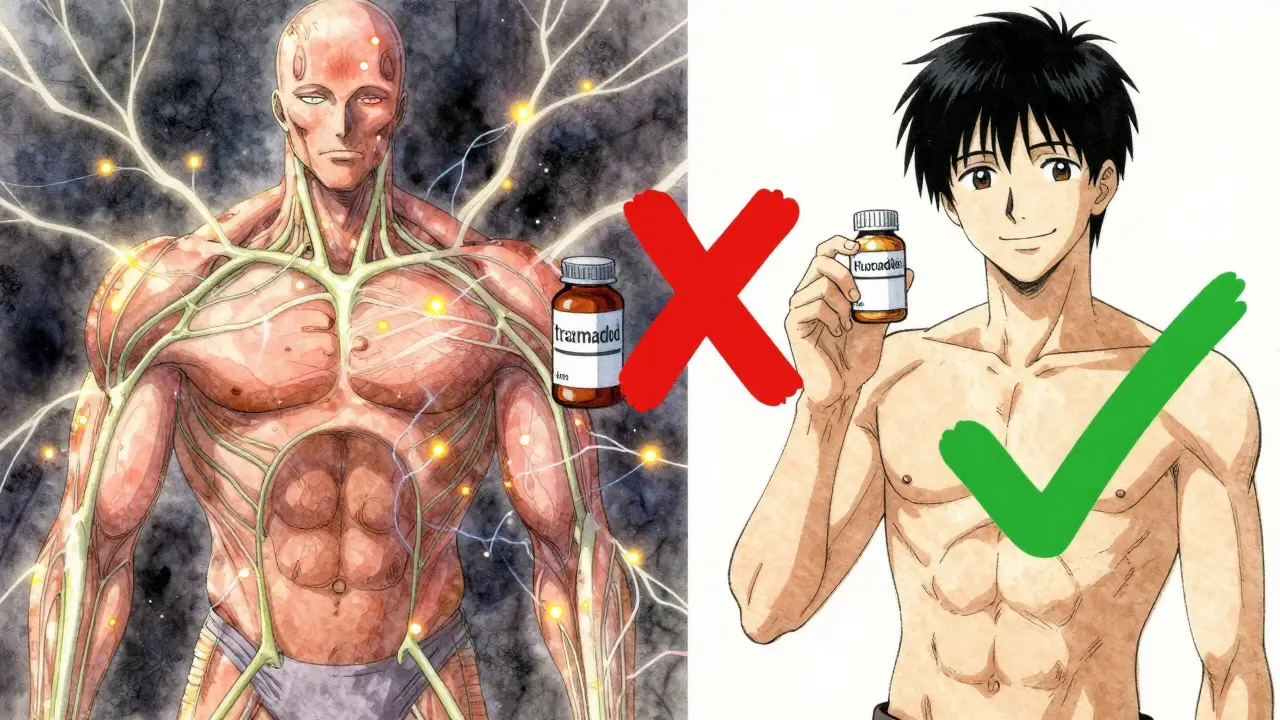
Not All Opioids Are Created Equal
Here’s where things get tricky: not every opioid carries the same risk. Many people assume all painkillers are equally dangerous when mixed with antidepressants. That’s not true.Tramadol, methadone, and pethidine are high-risk opioids. They don’t just relieve pain-they directly block serotonin reuptake, just like SSRIs do. Tramadol is especially concerning. Studies show it’s 30 times more potent at blocking serotonin than morphine. In the U.S., between 2018 and 2022, nearly 900 cases of serotonin syndrome linked to opioid-SSRI combinations were reported to the FDA. Tramadol was involved in over one-third of them.
On the other hand, morphine, oxycodone, buprenorphine, and hydromorphone have little to no effect on serotonin. They’re much safer choices if you’re already on an SSRI. Codeine was once thought to be safe, but case reports now show it can trigger serotonin syndrome too-especially in people with certain genetic differences that affect how their body processes it.
Fentanyl is another curveball. Lab tests show it doesn’t block serotonin reuptake. Yet, over 120 real-world cases of serotonin syndrome have been linked to fentanyl. Why? It might directly stimulate serotonin receptors instead. This is why lab results don’t always predict real-life risk.
Who’s Most at Risk?
You don’t have to be overdosing to get serotonin syndrome. Sometimes, it happens after just one new dose. People most at risk include:- Those taking tramadol with any SSRI or SNRI
- Patients switching from an MAOI (an older type of antidepressant) to an SSRI without waiting long enough
- Older adults on multiple medications-people over 65 take, on average, 31% more drugs than younger adults
- People with liver or kidney problems, which slow down how fast drugs are cleared from the body
- Those with a genetic variation in the CYP2D6 enzyme, which affects how tramadol and other drugs are metabolized
Fluoxetine is especially risky because it sticks around in your system for weeks. Even if you stop taking it, the active metabolite can linger for up to 16 days. That means if you start tramadol just a week after quitting fluoxetine, you’re still at risk.
What Does Serotonin Syndrome Look Like?
It’s not always obvious. Many doctors mistake it for infections, drug withdrawal, or even a stroke. The key is recognizing the pattern.The Hunter Criteria, the most reliable diagnostic tool, looks for these combinations:
- Spontaneous clonus (involuntary muscle contractions)
- Inducible clonus + agitation or sweating
- Inducible clonus + muscle stiffness + high temperature
- Tremor + overactive reflexes
Early signs are subtle: shivering you can’t stop, a racing heart, sudden sweating, diarrhea, or feeling unusually anxious. Later signs are more alarming: high fever, rigid muscles, confusion, seizures. If you’re on an SSRI and start a new opioid, watch for these symptoms in the first 24 to 72 hours. That’s when the risk peaks.
One study found that nearly half of all serotonin syndrome cases involving opioids and antidepressants were misdiagnosed at first. That delay can cost lives.
How to Prevent It
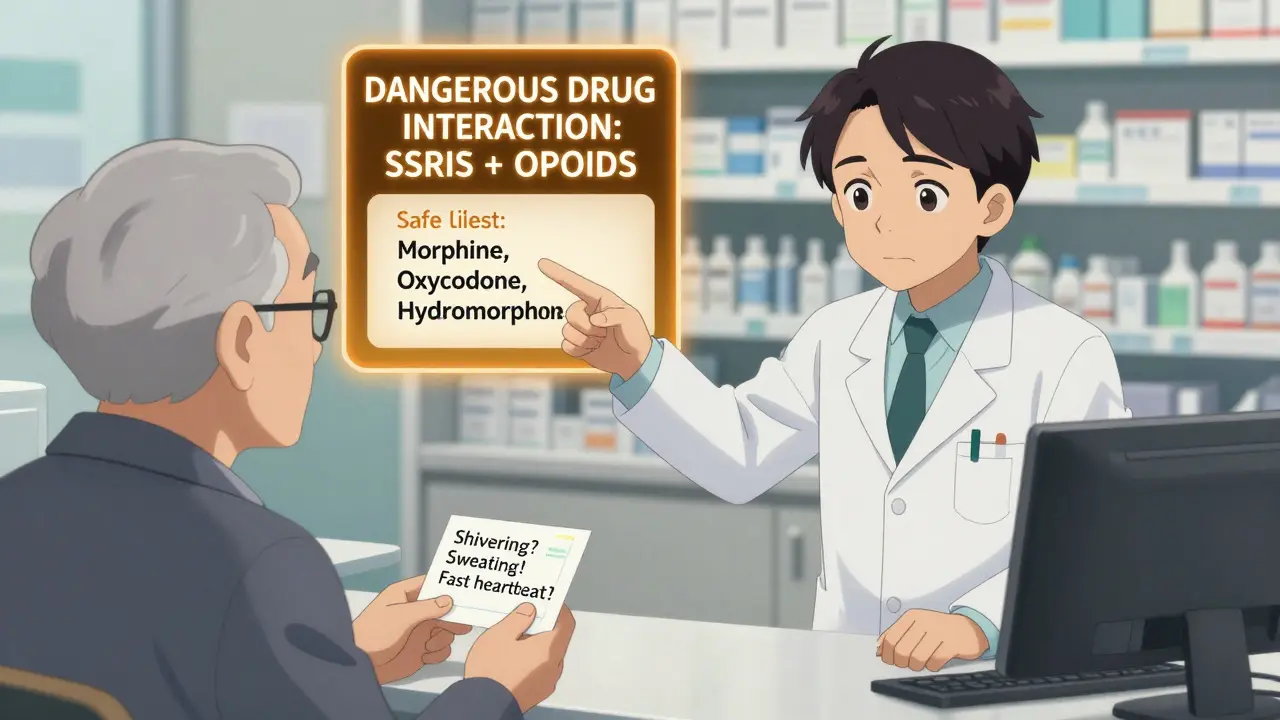
Prevention isn’t about avoiding pain relief or depression treatment. It’s about making smarter choices.- Avoid high-risk combinations. If you’re on an SSRI, ask your doctor to avoid tramadol, methadone, and pethidine. Use morphine, oxycodone, or hydromorphone instead.
- Wait before switching. If you’re coming off an MAOI, wait at least 14 days before starting an SSRI. For fluoxetine, wait five weeks.
- Start low, go slow. If you must take a higher-risk opioid, begin with half the usual dose and monitor closely for 72 hours.
- Know your genes. If you’ve had unexplained reactions to medications before, ask about CYP2D6 testing. Poor metabolizers are at much higher risk with tramadol.
- Use electronic alerts. Many hospitals now have systems that block dangerous prescriptions. Ask if your pharmacy or clinic uses these tools.
Patients should also carry a simple symptom checklist: “Shivering I can’t control? Muscle twitching? Fast heartbeat? Sweating out of nowhere? Confusion or agitation?” If you answer yes to any of these after starting a new painkiller, seek help immediately.
What If It Happens?
If serotonin syndrome is suspected, stop all serotonergic drugs right away. That’s step one.For mild cases, symptoms often resolve in 24 to 72 hours with supportive care: fluids, cooling, and rest. Benzodiazepines like lorazepam can calm agitation and muscle spasms.
For severe cases, you need hospital care. Cyproheptadine, a serotonin blocker, is given orally or through a feeding tube. The first dose is usually 12 mg, followed by 2 mg every two hours if symptoms persist. Cooling measures, IV fluids, and breathing support may be needed if your temperature is dangerously high.
There’s no magic blood test for serotonin syndrome. Diagnosis is based on symptoms and medication history. That’s why knowing what you’re taking-and telling your doctor every drug, even over-the-counter ones-is critical.
Why This Matters Now More Than Ever
Between 2017 and 2022, serotonin syndrome cases rose by over 34%. Why? More people are taking both antidepressants and opioids. In 2022, over 21% of opioid prescriptions were written for patients already on antidepressants. That’s over 10 million people at potential risk.Regulators are catching on. The FDA now requires opioid medication guides to include serotonin syndrome warnings. The European Medicines Agency has strengthened labels on tramadol. In the U.S., Kaiser Permanente cut dangerous tramadol-SSRI prescriptions by 87% after adding automatic alerts in their electronic system.
But the real solution is awareness. Doctors need to ask about antidepressants before prescribing painkillers. Patients need to know to speak up if they feel strange after a new medication. Pharmacists need to flag combinations before the bottle is filled.
This isn’t about fear. It’s about control. You don’t have to choose between pain relief and mental health care. You just need to choose the right combination.
Can I take tramadol with an SSRI if I’m careful?
No. Even at normal doses, tramadol combined with an SSRI carries a high risk of serotonin syndrome. Studies show the risk is over four times higher than with morphine. There are safer painkillers available. Don’t rely on "being careful"-the reaction can happen after just one dose.
Is serotonin syndrome the same as an allergic reaction?
No. Allergic reactions involve your immune system and usually cause rashes, swelling, or breathing trouble. Serotonin syndrome is a toxic reaction from too much serotonin in your brain and nerves. It causes muscle spasms, high temperature, and rapid heartbeat-not hives or swelling.
What if I’m on an older antidepressant like amitriptyline?
Tricyclic antidepressants (TCAs) like amitriptyline also increase serotonin, though less than SSRIs or SNRIs. They still carry risk when combined with opioids like tramadol or methadone. Safer alternatives like morphine or oxycodone are preferred. Always check with your doctor before mixing any antidepressant with a painkiller.
Can I use over-the-counter medicines like dextromethorphan with SSRIs?
Dextromethorphan, found in many cough syrups, blocks serotonin reuptake just like tramadol. Combining it with an SSRI can cause serotonin syndrome-even if you’re only taking a few doses. Read labels carefully. Avoid any cough medicine with dextromethorphan if you’re on an SSRI.
How long should I wait after stopping an SSRI before taking tramadol?
It depends on the SSRI. For sertraline or escitalopram, wait at least 5 to 7 days. For fluoxetine, wait at least five weeks because it stays in your system so long. Never guess-ask your doctor or pharmacist for the exact timeline based on your medication.
If you’re currently taking both an SSRI and an opioid, don’t panic. But do take action. Talk to your doctor. Ask if your painkiller is high-risk. Ask about safer alternatives. Bring your full medication list-every pill, patch, and supplement-to your next appointment. Serotonin syndrome is preventable. But only if you know the signs and speak up.

Gerald Tardif
December 28, 2025 AT 12:30Been on sertraline for years and just started oxycodone for a bad back. Never even thought about serotonin syndrome until I read this. Thanks for laying it out so clearly. I’m gonna print this out and bring it to my next appt.
Robyn Hays
December 29, 2025 AT 21:14I’m a nurse and I’ve seen this go wrong too many times. A 72-year-old woman came in with fever, rigidity, and confusion-doc thought it was UTI. She was on fluoxetine and tramadol. Took three days to connect the dots. By then she was in ICU. This isn’t rare. It’s systemic. We need better training, not just warning labels.
Liz Tanner
December 31, 2025 AT 14:20My mom was on citalopram and got prescribed tramadol after her hip surgery. She started shaking uncontrollably and sweating like crazy. The ER doctor didn’t know what was going on. We had to push for serotonin syndrome. She’s fine now but scared to take anything. This info should be mandatory in every pharmacy.
Satyakki Bhattacharjee
January 1, 2026 AT 11:09People these days want everything easy. Take a pill for sadness, take a pill for pain. Then wonder why their body breaks. Nature didn’t design us to mix chemicals like cocktails. Stop being lazy. Talk to your doctor. Or better yet, get off the pills and pray.
Anna Weitz
January 3, 2026 AT 04:49They’re hiding the truth. The pharma companies know how dangerous this combo is. That’s why they market tramadol as "non-addictive" and "mild". It’s not. It’s a stealth serotonin bomb. And the FDA? They’re bought and paid for. Wake up people. This isn’t medicine. It’s corporate murder
Jane Lucas
January 4, 2026 AT 11:00just took my first dose of oxycodone yesterday and i’ve been on escitalopram for 3 years. i’m fine but now i’m paranoid. shivering? is that normal? heart racing? or just anxiety? why does no one tell you this stuff before you start
Elizabeth Alvarez
January 5, 2026 AT 19:47Did you know that the CDC has been quietly tracking serotonin syndrome cases since 2015 but never released the full data? They’re scared of the panic. And why? Because if people realized how many are dying from doctor-prescribed meds, the whole system would collapse. Fluoxetine? It’s designed to linger. Tramadol? Engineered to sneak in. This isn’t an accident. It’s a slow, quiet genocide disguised as healthcare. And they’re calling it "pharmacovigilance". LOL.
Miriam Piro
January 6, 2026 AT 12:14They don’t want you to know this. The FDA, the AMA, the drug reps - they all profit from this. Tramadol is cheap. SSRIs are lifelong. Combine them? You get addicted to both. And when you get sick? You go back to the same doctors who put you on it. It’s a loop. A money machine. And you’re the product. I’ve seen it. My cousin died. They said "heart attack." But she was on sertraline and tramadol. No one asked about the combo. No one cared. 😔
dean du plessis
January 8, 2026 AT 04:08cool post. i live in cape town and we dont have much access to good med info here. but i shared this with my cousin who’s on antidepressants and just got prescribed codeine. he had no clue. now he’s gonna ask his doc before taking it. small wins man
Kylie Robson
January 8, 2026 AT 18:15From a clinical pharmacology standpoint, the CYP2D6 polymorphism is the critical variable here. Poor metabolizers exhibit a 3- to 4-fold increase in tramadol’s active metabolite M1, which has higher mu-opioid affinity and potent serotonin reuptake inhibition. This creates a non-linear pharmacokinetic risk curve that’s exponentially elevated in polypharmacy scenarios. The Hunter Criteria remain the gold standard, but we need validated biomarkers - plasma 5-HIAA levels, CSF serotonin, or even PET ligands for 5-HT2A occupancy - to enable early detection before clinical decompensation.