Subclinical Hyperthyroidism: Heart Risks and When to Treat
 Dec, 1 2025
Dec, 1 2025
Most people don’t know they have subclinical hyperthyroidism until a routine blood test shows it. No shaky hands. No weight loss. No racing heart. Just a low TSH number on a lab report, with everything else normal. But that quiet abnormality? It’s not harmless. Especially if you’re over 60. Or if you already have heart trouble. This isn’t just a lab quirk. It’s a hidden risk to your heart - and ignoring it can cost you dearly.
What Exactly Is Subclinical Hyperthyroidism?
Subclinical hyperthyroidism means your thyroid is working a little too hard - but not enough to spill over into your bloodstream. Your TSH (thyroid-stimulating hormone) drops below 0.45 mIU/L, while your free T4 and T3 levels stay perfectly normal. It’s like your thyroid is revving its engine in neutral. No one else sees it. But your heart feels it.
This condition sneaks up on people. It’s often found during check-ups for other things - maybe a blood pressure check or a routine blood panel. Older adults are most at risk. Up to 15% of people over 75 have it. The main causes? Toxic nodules in the thyroid (one or more overactive lumps) or too much thyroid hormone from medication, especially in people being treated for hypothyroidism.
Unlike overt hyperthyroidism - where you feel jittery, lose weight, and sweat through your shirts - subclinical hyperthyroidism gives you almost no warning signs. That’s why it’s so dangerous. You can’t feel it. But your heart still pays the price.
Why Your Heart Is in Danger
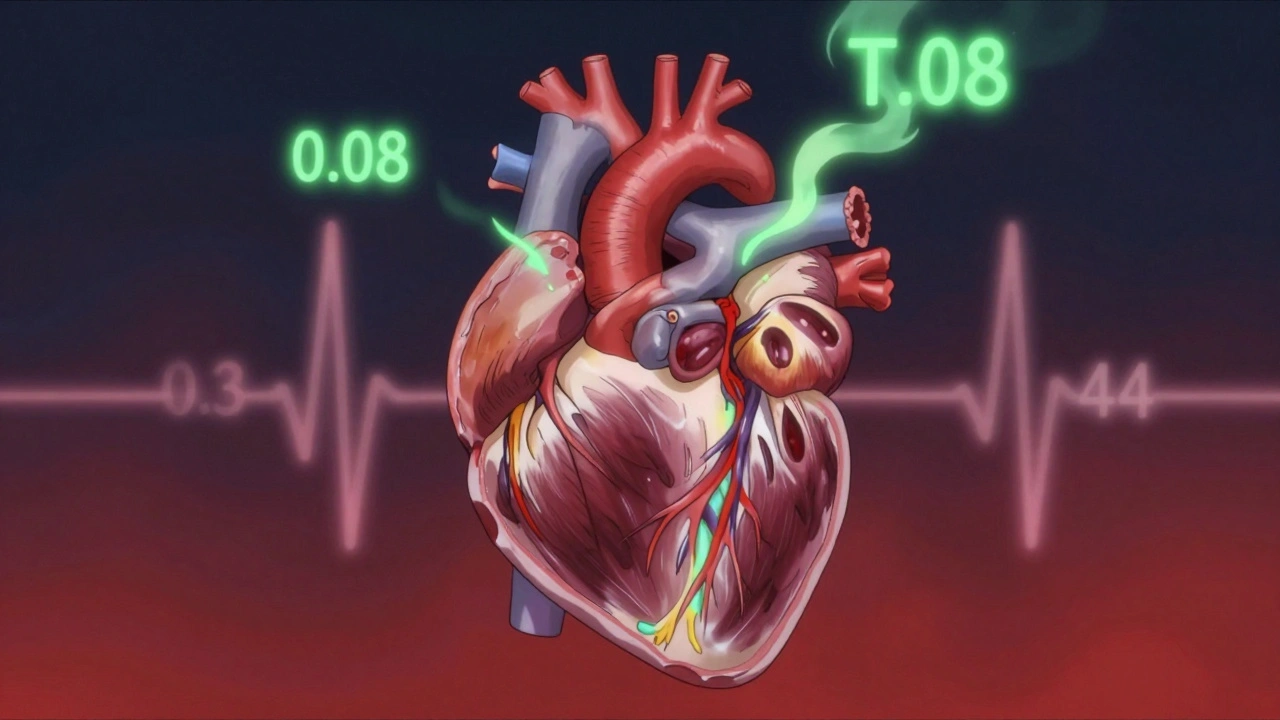
When TSH drops below 0.1 mIU/L, your heart starts changing. Not in a good way.
- Atrial fibrillation becomes 2.5 times more likely. That’s the irregular, often rapid heartbeat that can lead to stroke. Studies tracking over 8,700 people found this link clearly.
- Heart failure risk jumps by nearly double. One study of 71 patients showed a 2.93 times higher chance of heart failure - and if your TSH was below 0.1, the risk shot up to 4.6 times.
- Left ventricular mass increases. Your heart muscle thickens. It’s not training - it’s straining.
- Heart rate variability drops. That means your heart loses its ability to adapt to stress. Less flexibility. More risk.
These aren’t theoretical risks. They come from real data - large studies, long-term follow-ups, and meta-analyses. The risk doesn’t disappear just because you feel fine. Your heart doesn’t care how you feel. It responds to hormones. And when TSH is too low, your heart gets pushed too hard.
Even TSH levels between 0.1 and 0.44 mIU/L aren’t safe if you’re over 60 or have existing heart disease. One review found these patients had triple the risk of atrial fibrillation over 10 years. That’s not a small bump. That’s a red flag.
Who Needs Treatment - And Who Doesn’t?
Not everyone with subclinical hyperthyroidism needs treatment. But not treating the right people can be deadly.
Treat if:
- Your TSH is below 0.1 mIU/L - no exceptions. This is the clear danger zone. Experts like Dr. Anne R. Cappola say treat regardless of symptoms.
- You’re over 65. Age is a major risk multiplier. Your heart doesn’t bounce back like it used to.
- You have heart disease, high blood pressure, or a history of heart failure.
- You have osteoporosis or a high fracture risk. Subclinical hyperthyroidism weakens bones too.
Monitor, don’t treat, if:
- Your TSH is between 0.1 and 0.44 mIU/L and you’re under 65 with no heart or bone issues.
- You’re otherwise healthy and asymptomatic.
But here’s the catch: even if you’re not treated, you need regular check-ups. If your TSH drops further, or if you develop high blood pressure, palpitations, or bone loss, you need to reevaluate.
What Does Treatment Look Like?
Treatment isn’t one-size-fits-all. It depends on the cause.
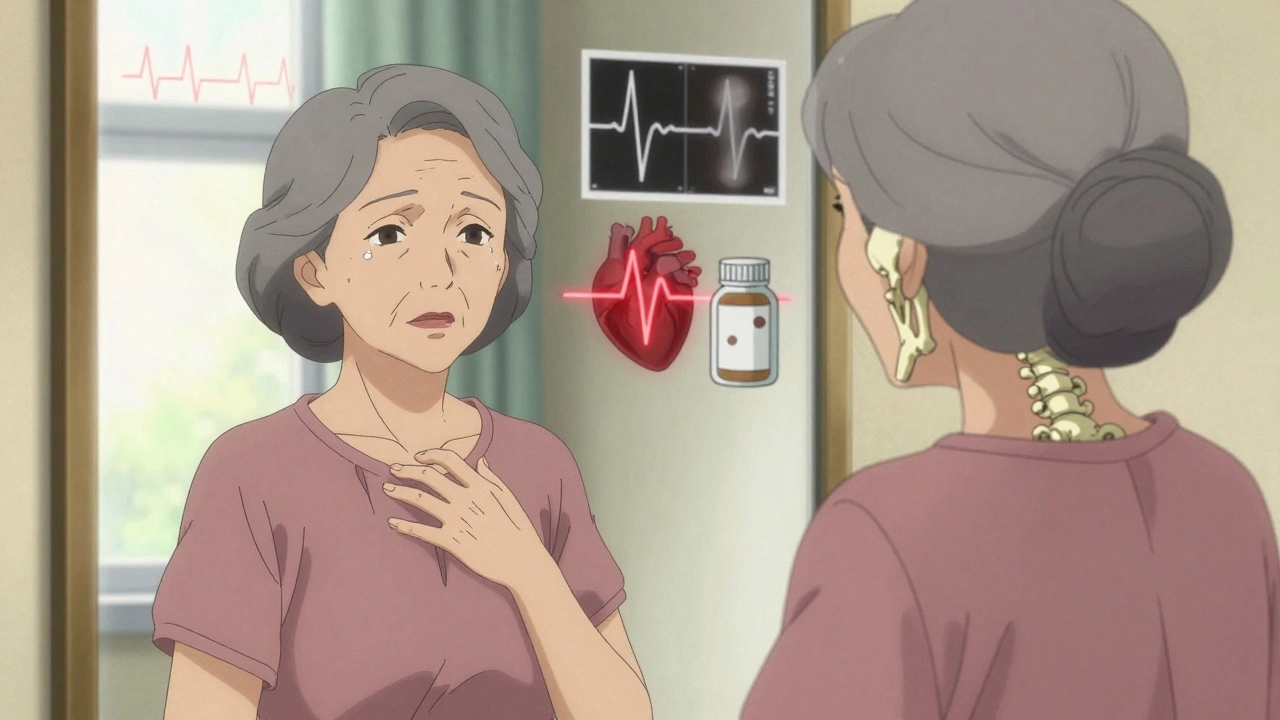
If your subclinical hyperthyroidism comes from too much thyroid medication - say, you’re on levothyroxine and your dose is too high - the fix is simple: lower the dose. Many people don’t realize their thyroid levels were fine until their doctor overcorrected. Reducing the dose often brings TSH back to normal without side effects.
If it’s caused by a toxic nodule or Graves’ disease, things get more serious. Radioactive iodine therapy is often the go-to. It shuts down the overactive part of the thyroid. Surgery is another option, especially if the nodule is large. Both carry risks - mainly, you’ll likely end up with hypothyroidism. But that’s often better than risking a stroke or heart failure.
For people with heart symptoms - like a fast heartbeat or palpitations - beta-blockers are used as a first step. They don’t fix the thyroid problem, but they calm the heart. They lower heart rate, reduce thickening of the heart muscle, and make you feel better while you decide on long-term treatment.
Dr. Kenneth D. Burman warns: “Treating mild thyroid dysfunction can create new problems.” Turning a subclinical case into full-blown hypothyroidism isn’t a win. It brings its own risks - including higher cholesterol and worse heart function. So treatment must be precise. Not too little. Not too much.
Monitoring Is Just as Important as Treatment
If you’re not treated, you still need to be watched.
- If your TSH is below 0.1 mIU/L: Check every 3 to 6 months.
- If your TSH is between 0.1 and 0.44 mIU/L and you’re low-risk: Check once a year.
Each visit should include a TSH test, a heart exam (maybe an ECG), and a bone density check if you’re over 60 or have other risk factors. Don’t wait for symptoms. By the time you feel something, the damage may already be done.
And don’t forget: your thyroid doesn’t work in isolation. Your heart, your bones, your brain - they’re all connected. Even subtle thyroid changes can affect memory and thinking in older adults. One 2016 study found subtle declines in executive function in elderly patients with persistent low TSH.
The Big Picture: It’s Not Just About Thyroid Levels
Doctors used to think: if you don’t feel sick, don’t treat it. But that thinking is outdated. Subclinical hyperthyroidism isn’t a “borderline” issue. It’s a cardiovascular risk factor - just like high cholesterol or smoking.
European guidelines say: treat everyone with TSH below 0.1. American guidelines are more cautious. But even the American Thyroid Association now says: if you’re over 65 and your TSH is low, think hard about treatment.
The future is coming. The THAMES trial and the DEPOSIT study are tracking thousands of older adults to see whether treating subclinical hyperthyroidism actually prevents heart attacks and strokes. Results won’t be in until 2026. But the evidence we have now is strong enough to act.
Don’t wait for a stroke. Don’t wait for a diagnosis of heart failure. If your TSH is below 0.1 - especially if you’re over 60 - talk to your doctor. Get an ECG. Check your bones. Ask if treatment makes sense.
This isn’t about chasing perfect numbers. It’s about protecting your heart - before it’s too late.
What Happens If You Do Nothing?
Some people with low TSH live for years without problems. That’s true. But others? They wake up one day with atrial fibrillation. Or they fall and break a hip because their bones are brittle. Or they’re hospitalized for heart failure.
The risk isn’t guaranteed. But it’s real. And it’s preventable.
Ignoring subclinical hyperthyroidism is like ignoring high blood pressure because you don’t have a headache. The damage builds silently. Then, when it hits - it hits hard.
Can subclinical hyperthyroidism go away on its own?
Yes, in some cases. If it’s caused by temporary inflammation or a mild thyroid flare-up, TSH can normalize without treatment. But if it’s due to a toxic nodule or long-term medication overuse, it usually doesn’t fix itself. That’s why repeated testing is needed - at least two or three blood tests over 3-6 months - to confirm it’s persistent.
Is subclinical hyperthyroidism common in younger people?
It’s rare under age 50. The prevalence jumps sharply after 60. In people under 50, it’s usually tied to Graves’ disease or medication errors. In older adults, toxic nodules are the main cause. That’s why screening is focused on seniors.
Can I just take less thyroid medication if my TSH is low?
If you’re on levothyroxine and your TSH is low, yes - but only under medical supervision. Dropping your dose too fast can cause hypothyroidism. Your doctor will usually lower it by small amounts (like 12.5 mcg) and retest in 6-8 weeks. Never adjust your dose on your own.
Does subclinical hyperthyroidism affect mental health?
It can. Some older adults report mild memory issues, trouble focusing, or mood swings - even without obvious thyroid symptoms. These changes are subtle and often mistaken for normal aging. But studies link persistent low TSH to reduced performance in executive function tasks. Treating it may help.
What’s the biggest mistake doctors make with this condition?
Over-treating mild cases. Some doctors panic at a low TSH and rush to radioactive iodine or surgery. But if you’re young, healthy, and your TSH is only slightly low (say, 0.3), you might be better off watching and waiting. The goal isn’t to get TSH into the “normal” range at all costs - it’s to avoid heart damage and fractures without creating new problems.
Should I get a bone density scan if I have low TSH?
If you’re over 60 - yes. Especially if you’re female, have a family history of osteoporosis, or have already had a fracture. Subclinical hyperthyroidism accelerates bone loss. A DEXA scan takes 10 minutes and can tell you if you need calcium, vitamin D, or medication to protect your bones.
Next Steps: What to Do Now
If you’ve been told you have subclinical hyperthyroidism:
- Get your TSH retested in 3 months if it’s below 0.1, or 6-12 months if it’s between 0.1 and 0.44.
- Ask for an ECG to check for atrial fibrillation.
- If you’re over 60, request a bone density scan.
- Review all your medications - especially thyroid pills - with your doctor.
- Don’t ignore symptoms like palpitations, shortness of breath, or unexplained fatigue.
If you’re over 65 and haven’t had a thyroid test in the last year - ask for one. It’s simple. It’s cheap. And it could save your heart.

John Biesecker
December 3, 2025 AT 03:36Genesis Rubi
December 3, 2025 AT 07:15Doug Hawk
December 4, 2025 AT 08:23John Morrow
December 6, 2025 AT 02:02Kristen Yates
December 6, 2025 AT 23:24Saurabh Tiwari
December 8, 2025 AT 18:17Michael Campbell
December 9, 2025 AT 05:13Victoria Graci
December 9, 2025 AT 09:33Saravanan Sathyanandha
December 10, 2025 AT 00:30alaa ismail
December 10, 2025 AT 22:19ruiqing Jane
December 12, 2025 AT 12:58