Tricyclic Antidepressants and Antihistamines: The Hidden Danger of Anticholinergic Overload
 Dec, 20 2025
Dec, 20 2025
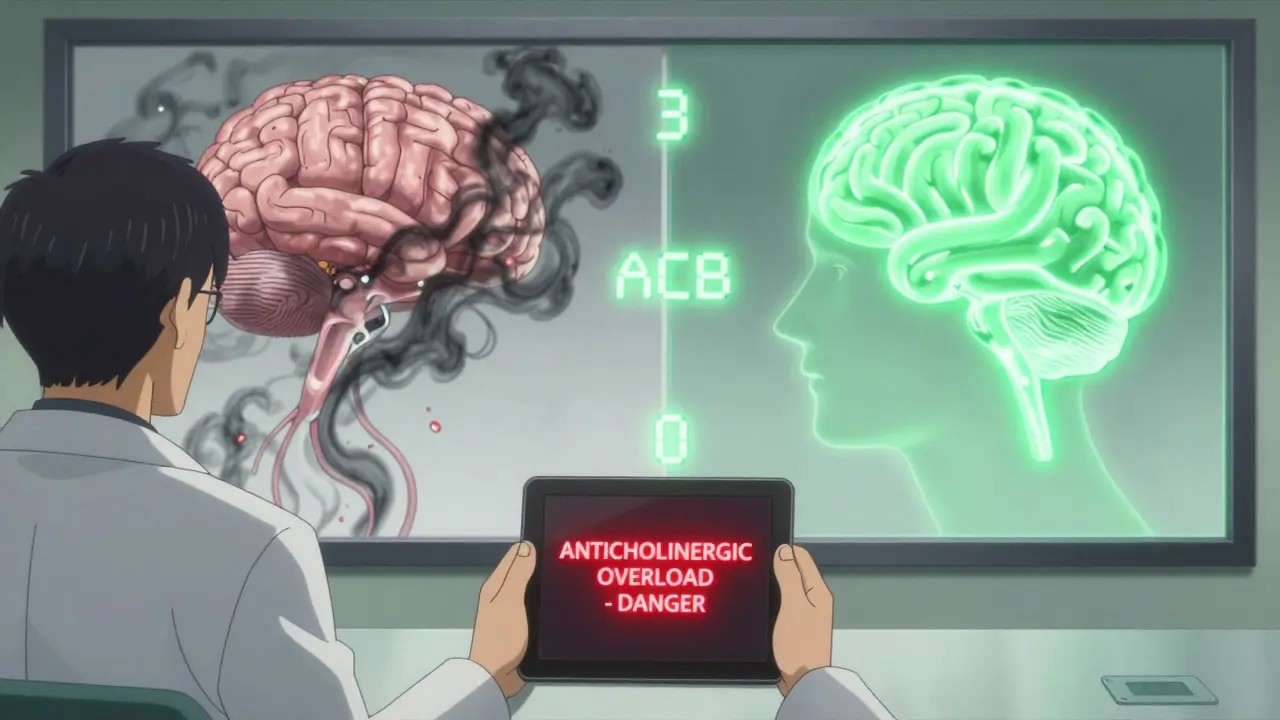
Anticholinergic Burden Calculator
Anticholinergic Burden Calculator
Enter your medications to calculate your cumulative anticholinergic burden score. Scores above 3 increase dementia risk significantly.
Current Burden Score:
Risk Level:
What This Means:
Recommendations:
Imagine taking a pill for sleep, another for depression, and not realizing together they’re quietly shutting down your brain’s ability to think clearly. This isn’t science fiction. It’s happening right now to thousands of people-especially older adults-because of a dangerous but rarely discussed drug interaction: anticholinergic overload from combining tricyclic antidepressants (TCAs) and first-generation antihistamines.
What Exactly Is Anticholinergic Overload?
Your body uses acetylcholine, a key neurotransmitter, to control everything from memory and attention to bladder function and heart rate. Anticholinergic drugs block this chemical. Individually, drugs like amitriptyline or diphenhydramine (Benadryl) can cause mild side effects-dry mouth, drowsiness, constipation. But when taken together, their effects stack up like layers of paint on a wall. The result? A system-wide shutdown of cholinergic activity. This is anticholinergic overload.It’s not just uncomfortable. It’s dangerous. In older adults, it can trigger sudden confusion, hallucinations, urinary retention, and even delirium. A 2022 study found that 52% of high-risk drug interaction alerts in patients taking TCAs involved combinations with other medications-and antihistamines were among the most common culprits.
Why TCAs and Antihistamines Are a Toxic Pair
Tricyclic antidepressants like amitriptyline, imipramine, and clomipramine were developed in the 1950s. They work by boosting serotonin and norepinephrine, but they also strongly block muscarinic receptors-the same receptors targeted by antihistamines like diphenhydramine, hydroxyzine, and chlorpheniramine. These older antihistamines were designed to cross the blood-brain barrier to fight allergies and induce sleep. That’s exactly what makes them dangerous when paired with TCAs.Here’s the math: Amitriptyline has an anticholinergic burden score of 3 on the Anticholinergic Cognitive Burden (ACB) scale-the highest possible. Diphenhydramine scores a 2. Together? That’s a cumulative score of 5. Research shows that a score of 3 or higher doubles the risk of dementia over time. A 2015 JAMA Internal Medicine study found chronic use of drugs with an ACB score of 3+ increased dementia risk by 54%.
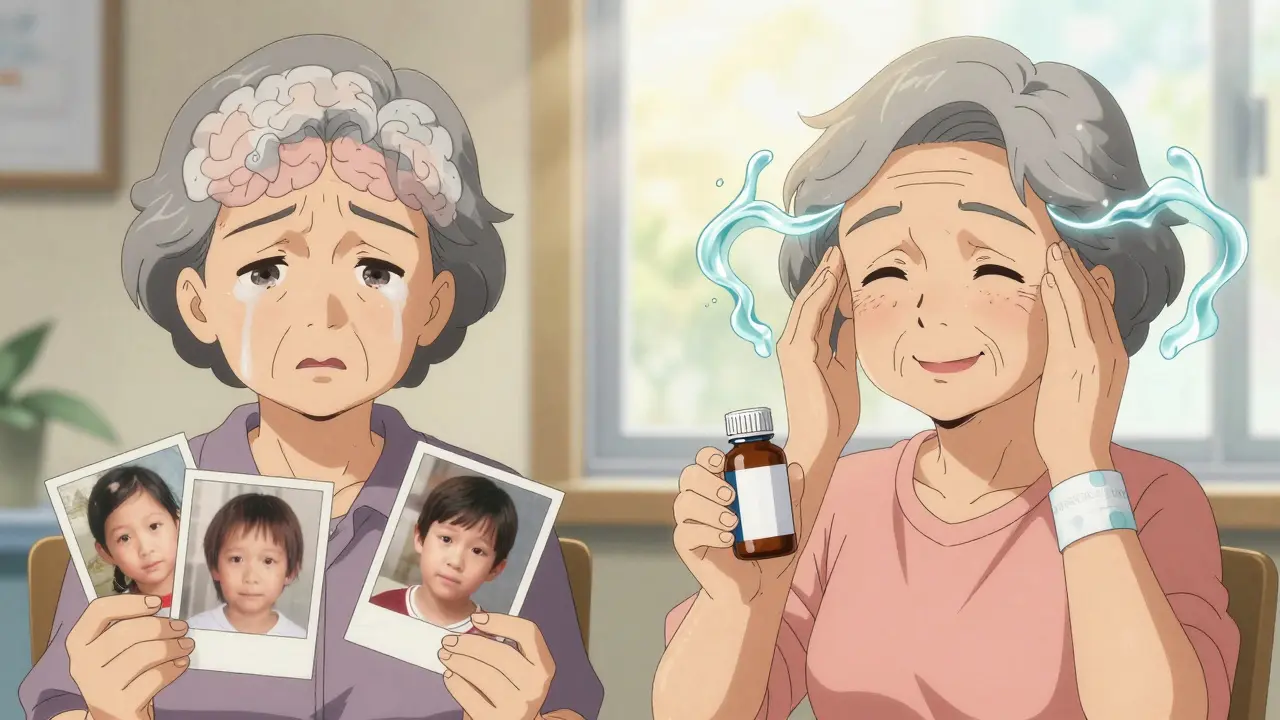
And it’s not just long-term. Even short-term use can cause acute problems. A 2023 study in the Journal of the American Geriatrics Society showed that just 30 days of combined use in patients over 65 increased delirium risk by 200%. One patient I read about-a 72-year-old woman on amitriptyline for nerve pain-was given diphenhydramine for seasonal allergies. Within three days, she couldn’t remember her grandchildren’s names. She ended up in the ER with urinary retention and confusion. Her doctors called it anticholinergic toxicity. Her meds were stopped. She recovered in a week.
Not All Antidepressants Are Created Equal
If you’re on a TCA, it doesn’t mean you’re stuck with it. Not all antidepressants carry the same anticholinergic risk. SSRIs like sertraline or escitalopram have minimal anticholinergic effects-side effects like dry mouth or constipation occur in only 5-10% of users, compared to 30-50% with TCAs.Even among TCAs, there’s variation. Nortriptyline and desipramine are less anticholinergic than amitriptyline or clomipramine. Clomipramine is unique-it’s the only TCA with strong serotonin and norepinephrine reuptake inhibition, but it’s also one of the most anticholinergic. If you’re on amitriptyline and struggling with side effects, ask your doctor if switching to nortriptyline might help.
But here’s the catch: TCAs are still first-line for neuropathic pain, fibromyalgia, and chronic insomnia. That’s why they’re still prescribed. The problem isn’t the drug itself-it’s the lack of awareness around how they interact with other common meds.
What About Antihistamines? Are They All Bad?
No. Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) barely cross the blood-brain barrier. They have an ACB score of 0. That means they don’t block acetylcholine receptors in the brain. They’re just as effective for allergies but won’t make you foggy-headed or increase your dementia risk.And if you’re using diphenhydramine for sleep? There are better options. Melatonin (0.5-5 mg) works without anticholinergic effects. Trazodone (low dose, 25-50 mg) is often used off-label for sleep and has far less anticholinergic activity than Benadryl. Doxepin is an antidepressant with sedative properties, but even then, it’s used at much lower doses for sleep-1-6 mg-and has less buildup than TCAs taken for depression.
Who’s at Risk? And How Often Does This Happen?
Elderly patients are the most vulnerable. Their livers metabolize drugs slower. Their brains are more sensitive to acetylcholine loss. But it’s not just the elderly. Anyone taking multiple CNS-acting drugs is at risk. A 2020 Elsevier study found a single patient prescribed fluoxetine, sertraline, amitriptyline, tramadol, lorazepam, and alprazolam simultaneously-six drugs, all with some level of anticholinergic or sedative effect. That’s a recipe for disaster.And it’s more common than you think. A 2021 survey by the American Geriatrics Society found 37% of pharmacists encountered anticholinergic overload cases at least once a month. Of those, nearly 3 out of 10 involved TCA-antihistamine combos. On Reddit, medical residents shared stories of elderly patients admitted with delirium traced back to Benadryl + TCA. One user on Psych Forums described ending up in the ER after combining amitriptyline and diphenhydramine for sleep.
Even more alarming: GoodRx recorded over 15,000 user queries about amitriptyline interactions in 2022. Of those, 22% specifically asked about Benadryl. People are noticing something’s wrong. But they’re not always getting the right answers from their doctors.
What Should You Do?
If you’re on a TCA and taking an over-the-counter sleep aid or allergy pill, stop and think. Check the active ingredient. If it’s diphenhydramine, chlorpheniramine, or hydroxyzine-stop. Talk to your doctor. Don’t just quit cold turkey, especially with TCAs. But do ask: Is this necessary? Is there a safer alternative?Ask for the ACB score of all your meds. Many hospitals now use it. If your doctor doesn’t know what it is, ask them to look it up. You can also use free tools like the Anticholinergic Burden Calculator from the University of Michigan. It’s simple: enter your meds, get a score.
Here’s a quick guide:
- High-risk (ACB 3): Amitriptyline, clomipramine, doxepin (high dose)
- Moderate-risk (ACB 2): Diphenhydramine, hydroxyzine, promethazine
- Low-risk (ACB 1): Carbamazepine, oxybutynin
- Safe (ACB 0): Loratadine, cetirizine, fexofenadine, melatonin
Also, ask about pharmacogenomic testing. If you’re a CYP2D6 poor metabolizer (about 7% of people), your body can’t break down TCAs properly. That makes toxicity 3.2 times more likely when you add another drug that affects the same enzyme.
What’s Changing in Medicine?
The tide is turning. In 2023, the FDA required all TCA and first-generation antihistamine labels to include clear warnings about cumulative anticholinergic effects. The American Geriatrics Society’s Beers Criteria now explicitly says: “Avoid first-generation antihistamines in older adults taking TCAs.”Electronic health records like Epic now block these combinations. If a doctor tries to prescribe diphenhydramine with amitriptyline, the system pops up a hard stop. In 92% of cases, it works. That’s progress.
And deprescribing works. A 2023 study showed that when elderly patients stopped anticholinergic drugs, their cognitive function improved by 34% in just 18 months. That’s not a small gain. That’s life-changing.
Final Thought: Your Brain Deserves Better
Medications aren’t harmless. Even common, over-the-counter ones can quietly harm you when layered on top of others. Anticholinergic overload isn’t rare. It’s preventable. If you’re on a TCA, don’t assume that a sleep aid or allergy pill is safe just because it’s available without a prescription. Ask. Check. Swap. Your memory, your focus, your independence-they’re worth protecting.Can I take Benadryl with amitriptyline?
No. Combining Benadryl (diphenhydramine) with amitriptyline significantly increases your risk of anticholinergic overload. Both drugs block acetylcholine, and together they can cause confusion, urinary retention, rapid heartbeat, and even delirium-especially in people over 65. Even if you’ve taken them together before without issues, the risk builds up over time. Switch to a non-sedating antihistamine like loratadine or cetirizine instead.
Do all antidepressants cause anticholinergic side effects?
No. Tricyclic antidepressants (TCAs) like amitriptyline and clomipramine have strong anticholinergic effects. But SSRIs like sertraline, fluoxetine, and escitalopram have very little. SNRIs like venlafaxine and duloxetine are also low-risk. If you’re experiencing dry mouth, constipation, or memory problems on a TCA, ask your doctor if switching to an SSRI is an option for your condition.
Is there a safe sleep aid to take with a TCA?
Yes. Melatonin (0.5-5 mg) is the safest choice-it doesn’t affect acetylcholine. Low-dose trazodone (25-50 mg) is also commonly used and has less anticholinergic activity than diphenhydramine. Avoid anything with diphenhydramine, doxylamine, or hydroxyzine. If sleep is still a problem, talk to your doctor about behavioral strategies or a sleep study. Don’t rely on sedating meds long-term.
How do I know if I’m experiencing anticholinergic overload?
Symptoms include sudden confusion, memory lapses, difficulty speaking, dry mouth, blurred vision, constipation, urinary retention, fast heartbeat, and feeling unusually drowsy or disoriented. If you’re on a TCA and start an antihistamine, and then notice these symptoms, stop the antihistamine and contact your doctor immediately. These signs can be mistaken for dementia or aging-but they’re often reversible if caught early.
Can anticholinergic overload cause permanent damage?
Long-term exposure increases dementia risk by up to 54%, according to JAMA Internal Medicine. But short-term overload-like a few weeks of combined use-usually causes temporary confusion or delirium that clears once the drugs are stopped. The damage isn’t always permanent, but repeated episodes can accelerate cognitive decline. The goal is prevention: avoid the combo altogether.
Are there tools to check my medication risk?
Yes. The Anticholinergic Cognitive Burden (ACB) scale is the gold standard. You can find free online calculators from the University of Michigan or the American Geriatrics Society. Just enter your meds, and it gives you a score. Anything above 3 is high risk. Also, ask your pharmacist to run a drug interaction check. Most pharmacies now have systems that flag these combos automatically.

Siobhan K.
December 22, 2025 AT 00:09Brian Furnell
December 22, 2025 AT 16:45Meina Taiwo
December 22, 2025 AT 21:33Adrian Thompson
December 23, 2025 AT 02:17Southern NH Pagan Pride
December 24, 2025 AT 09:31Jackie Be
December 24, 2025 AT 19:41John Hay
December 26, 2025 AT 07:25Peggy Adams
December 27, 2025 AT 02:53Sarah Williams
December 27, 2025 AT 20:03Jay lawch
December 27, 2025 AT 22:13Christina Weber
December 29, 2025 AT 07:41Grace Rehman
December 30, 2025 AT 19:09