Vitamin K Foods and Warfarin Interactions for INR Control
 Dec, 6 2025
Dec, 6 2025
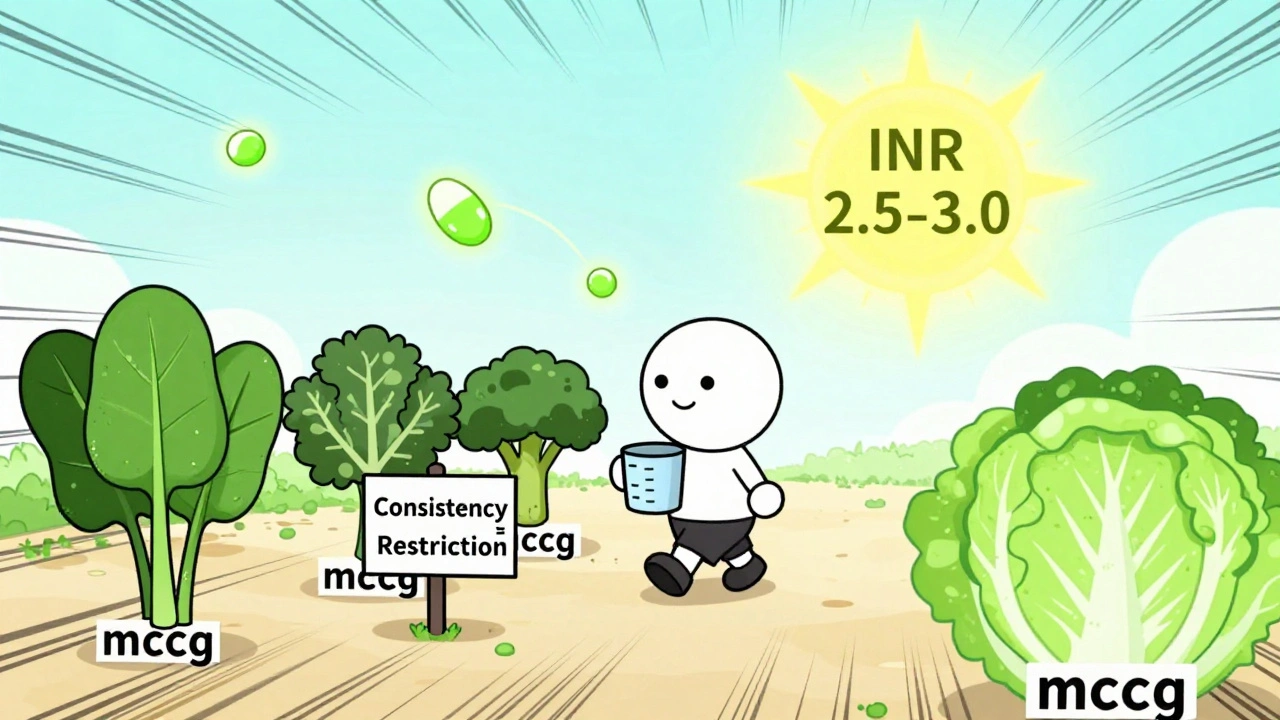
When you're on warfarin, your life doesn't stop - but your plate might need a rethink. It's not about cutting out healthy foods. It's about keeping things consistent. One day you eat a big bowl of spinach, the next day you switch to iceberg lettuce, and suddenly your INR drops. That’s not luck. That’s vitamin K at work.
Why Vitamin K Matters When You're on Warfarin
Warfarin doesn’t thin your blood. It slows down your body’s ability to make clotting factors. Those factors need vitamin K to work. So when you eat more vitamin K, your body makes more clotting factors, and warfarin becomes less effective. Eat less vitamin K? Your INR goes up. Too high, and you risk bleeding. Too low, and you risk clots.The goal? Keep your INR between 2.0 and 3.0 - or 2.5 to 3.5 if you have a mechanical heart valve. That’s the sweet spot. And the biggest thing you can control? Your daily vitamin K intake.
What Counts as High-Vitamin K Food?
Not all greens are created equal. The American Heart Association says foods with 60 micrograms (mcg) or more of vitamin K per serving are high-risk for INR swings. Here’s what’s on the list:- Cooked spinach: 889 mcg per cup
- Cooked kale: 547 mcg per cup
- Cooked broccoli: 220 mcg per cup
- Cooked Brussels sprouts: 219 mcg per cup
- Cabbage: 108 mcg per cup
- Green tea: 100+ mcg per cup (yes, even tea)
- Prune juice: 50 mcg per cup
- Chicken liver: 70 mcg per 3 oz
On the flip side, foods under 35 mcg per serving - like apples, bananas, carrots, eggs, and white rice - are safe to eat without worry. Iceberg lettuce? Just 17 mcg per cup. It’s not nutritionally impressive, but for INR stability? It’s a reliable choice.
Consistency Over Restriction
For years, doctors told people on warfarin to avoid vitamin K. That advice is outdated. The 2023 American College of Chest Physicians Guidelines say: Don’t restrict. Stabilize.It’s not about eating less vitamin K. It’s about eating the same amount every day. If you normally eat one cup of cooked broccoli (220 mcg), keep eating one cup every day. If you skip it for three days, your INR will climb. If you suddenly eat two cups, your INR will drop. That’s why 68% of INR instability events are tied to dietary changes.
One patient in Durban, who started logging every meal with a food-tracking app, went from 45% time in therapeutic range (TTR) to 92% in six months. Her secret? Exactly 1 cup of cooked broccoli, every single day. No more guessing.
How Cooking Changes Vitamin K
Boiling greens? You’re losing up to half the vitamin K. Steaming? You keep most of it. Raw spinach has more vitamin K than cooked - but if you cook it, you reduce the volume. A cup of raw spinach shrinks to 1/10th of a cup when cooked. So if you usually eat raw spinach salad (145 mcg per cup), and then switch to boiled spinach (889 mcg per cup cooked), you’re accidentally eating six times more vitamin K.Portion control matters. Use measuring cups. Don’t eyeball it. If you love kale, don’t quit it - just measure it. One cup cooked, every day. That’s the rule.
What About Supplements and Other Foods?
Vitamin K supplements? Avoid unless your doctor says otherwise. But here’s something surprising: some doctors now recommend a daily low-dose vitamin K supplement (100-200 mcg) for patients with erratic diets. A 2018 study found this brought 83% of patients back into range within a week.Other culprits? Green tea, cranberry juice, and certain herbal supplements like ginseng or garlic can also affect warfarin. They don’t have vitamin K, but they interfere with how your liver processes the drug. Stick to plain water. Avoid herbal teas unless you’ve checked with your anticoagulation clinic.
Real Stories, Real Consequences
Reddit user u/BloodThinWarrior posted: “Ate a big kale smoothie after a week of salads. My INR dropped from 2.8 to 1.9 in 48 hours. Had to up my warfarin by 20%.”Another user on MyHealth Alberta said: “I switched from spinach to iceberg lettuce because I thought I was being ‘healthy.’ My INR jumped to 4.1. I ended up in the ER with a nosebleed that wouldn’t stop.”
These aren’t rare. In a 2022 survey of 852 warfarin users, 78% linked INR swings directly to food changes. And 63% had at least one emergency visit after eating out - because restaurant meals are unpredictable. A “side of greens” could be kale, spinach, or a mystery blend. You don’t know.
How to Stay in Control
Here’s what works, based on real patient success:- Choose 1-2 high-vitamin K foods you like and eat them daily, in the same amount.
- Use a food-tracking app like CoumaDiet (rated 4.6/5 by over 1,200 users).
- Log every meal for two weeks. Look for patterns.
- Don’t change your diet before an INR test - it skews results.
- When eating out, ask for no added greens. Choose plain rice, potatoes, or grilled chicken.
- Get your INR checked monthly. More often if your dose changes.
Structured dietary education cuts INR instability by 37%. That’s not magic. That’s science. And it’s available at most anticoagulation clinics.
What About DOACs? Are They Better?
Direct oral anticoagulants (DOACs) like apixaban and rivaroxaban don’t interact with vitamin K. That’s why they’re now used in 68% of new prescriptions. But they’re not for everyone.Warfarin is still the only option for:
- People with mechanical heart valves (98% use warfarin)
- Patients with antiphospholipid syndrome (87% use warfarin)
- Those with kidney failure or who can’t afford DOACs
If you’re on warfarin, vitamin K management isn’t a burden - it’s your tool for safety. You don’t need to be perfect. You just need to be consistent.
What If Your INR Is Off?
If your INR is too high (over 3.5), your doctor might reduce your warfarin dose or give you a small amount of vitamin K. If it’s too low (under 2.0), they might increase your dose - but only after checking your diet. Never adjust your dose yourself.And if you’re traveling, plan ahead. Pack your usual foods. Bring a small food scale. Avoid buffet meals. Keep a written log of what you ate. Your anticoagulation clinic can help you prepare.
Can I eat leafy greens while on warfarin?
Yes - but only if you eat the same amount every day. A cup of cooked spinach daily is fine. Eating spinach one day and lettuce the next is not. Consistency beats restriction.
Does cooking destroy vitamin K in vegetables?
Boiling reduces vitamin K by 30-50%. Steaming, sautéing, or eating raw keeps more of it. But portion size matters more than cooking method. A cup of raw spinach has less vitamin K than a cup of boiled spinach because boiling shrinks the volume. Always measure cooked portions.
Should I take a vitamin K supplement?
Only if your doctor recommends it. Some patients with erratic diets are given 100-200 mcg daily to stabilize INR. But self-supplementing can be dangerous. Always talk to your anticoagulation team first.
How long does it take for vitamin K to affect INR?
It usually takes 2-4 days for a change in vitamin K intake to show up in your INR. That’s why you need to avoid big dietary shifts before your blood test. Your INR reflects what you ate over the past few days, not just yesterday.
Is it safe to eat out on warfarin?
It’s risky unless you plan ahead. Ask for your vegetables to be served on the side, or skip them. Choose grilled meats, plain rice, or potatoes. Avoid soups with greens, salads with unknown dressings, and dishes labeled “steamed vegetables.” Restaurants rarely know the vitamin K content of their sides.
What if I forget to eat my usual vitamin K food one day?
Don’t panic. One missed day won’t cause a crisis. But don’t make it a habit. If you miss it, eat a small portion of a low-vitamin K food like carrots or apples. Don’t compensate by eating extra greens the next day. Keep your weekly average steady.
Can I switch from warfarin to a DOAC to avoid this?
Maybe - but not always. DOACs don’t interact with vitamin K, but they’re not suitable for everyone. People with mechanical heart valves or antiphospholipid syndrome must stay on warfarin. Talk to your doctor about your options - but don’t assume switching is easy or always better.

Ashley Farmer
December 6, 2025 AT 13:12Just wanted to say this post saved my life. I was swinging between INR 1.8 and 4.2 every week until I started measuring my broccoli. Now I eat exactly one cup, steamed, every single night. No more ER visits. No more panic. It’s not glamorous, but it works.
Also, if you’re new to this - don’t feel guilty about iceberg lettuce. It’s boring, sure. But it’s your friend.
Jennifer Anderson
December 7, 2025 AT 22:35omg i just realized i’ve been eating raw spinach salads every morning and then switching to kale smoothies on weekends… no wonder my last INR was 4.5 😭
thanks for the wake up call. going to start logging with coumadiet rn. also… why does no one tell you this stuff before you get prescribed warfarin???
Sadie Nastor
December 8, 2025 AT 03:58🥬 I used to think I was being ‘healthy’ by eating tons of greens… turns out I was just playing Russian roulette with my blood.
Now I eat 1 cup of cooked broccoli every day like clockwork. My INR’s been stable for 8 months. 🙌
Also, if you’re scared to eat greens at all - you don’t have to quit them. Just make them predictable. Consistency > restriction. I cried when I finally understood that.
Also also - thank you for mentioning prune juice. I had no idea that was a culprit 😅
Sangram Lavte
December 9, 2025 AT 01:51As someone from India who’s been on warfarin for 5 years, I can confirm: Indian cooking is a minefield. Spinach curry? High. Fenugreek leaves? Higher. Even some dal preparations use dried spinach.
My trick? Stick to plain rice, roti, and boiled eggs. Avoid any dish labeled ‘saag’ unless I know exactly what’s in it. And yes - green tea is a no-go. I switched to ginger tea. Tastes better anyway.
Consistency is everything. Not restriction. This post nailed it.
Oliver Damon
December 9, 2025 AT 16:50From a pharmacokinetic standpoint, the delayed INR response (2–4 days) aligns with the half-life of vitamin K-dependent clotting factors, particularly factor VII (t½ ~6h) and factor II (t½ ~60–72h). The observed lag reflects the turnover rate of hepatic synthesis under warfarin-mediated VKOR inhibition.
What’s clinically significant is that dietary vitamin K doesn’t immediately alter INR - it modulates the *recovery kinetics* of the coagulation cascade. Hence, abrupt dietary shifts create a temporal mismatch between drug concentration and substrate availability.
This is why ‘consistency’ isn’t just advice - it’s a kinetic imperative. The 68% instability statistic? That’s not anecdotal. That’s biochemistry.
Ernie Blevins
December 10, 2025 AT 02:55So let me get this straight. You’re telling me I can’t eat a salad without getting my blood checked? And I have to measure my broccoli like I’m baking a cake?
And the government lets drug companies sell this crap? This is why I hate modern medicine. You’re not sick - you’re a lab rat with a pill schedule.
Also, I heard the FDA hides the truth about vitamin K. They don’t want you to know you can just take a supplement and skip the whole ‘eating right’ thing. Just saying.
David Brooks
December 11, 2025 AT 12:16THIS. THIS. THIS.
I was on warfarin for 3 years and thought I was doing great - until I ate one bowl of sautéed kale and ended up in the ER with a hematoma on my thigh. I thought I was being ‘healthy.’ Turns out I was being a dumbass.
Now I eat the same 1 cup of broccoli every day. I even have a little measuring cup I keep next to my stove. I’m not proud. I’m alive.
If you’re reading this and you’re on warfarin - stop guessing. Start measuring. Your future self will thank you. 🙏
Nicholas Heer
December 13, 2025 AT 01:59Who controls the food labels? Who decided broccoli = 220 mcg? What if the USDA is lying? What if the ‘1 cup’ measurement is just a corporate lie to sell measuring cups and apps?
And why is green tea on the list? Who decided that? Are they scared of tea? Is Big Pharma trying to make us drink water only?
I checked my local grocery store - their spinach has ‘organic vitamin K boost’ on the label. That’s not natural. That’s manipulation.
Also, why do all these ‘experts’ say ‘consistency’? Consistency with what? With their agenda? I’m done trusting doctors. I’m switching to DOACs. Even if it costs $500 a month. I’d rather be broke than controlled.
Kurt Russell
December 14, 2025 AT 06:27Hey - if you’re reading this and you’re stressed about vitamin K, STOP.
You don’t need to be perfect. You just need to be consistent. One cup of broccoli. Every day. Same time. Same way.
I used to be the guy who ate 5 different salads a week. Now? I eat one. Steamed. With a splash of olive oil. And I log it. And guess what? My INR hasn’t been out of range in 14 months.
You got this. It’s not about restriction. It’s about rhythm. Find your rhythm. Stick to it. And don’t let anyone make you feel guilty for eating iceberg lettuce. It’s not a crime. It’s a survival tactic. 💪