Why Regular Eye Pressure Checks Are Crucial to Prevent Glaucoma
 Oct, 21 2025
Oct, 21 2025
Glaucoma Risk Estimator
Your Glaucoma Risk Calculator
Estimate your glaucoma risk based on intraocular pressure and key risk factors. Results are for educational purposes only.
Your Risk Assessment
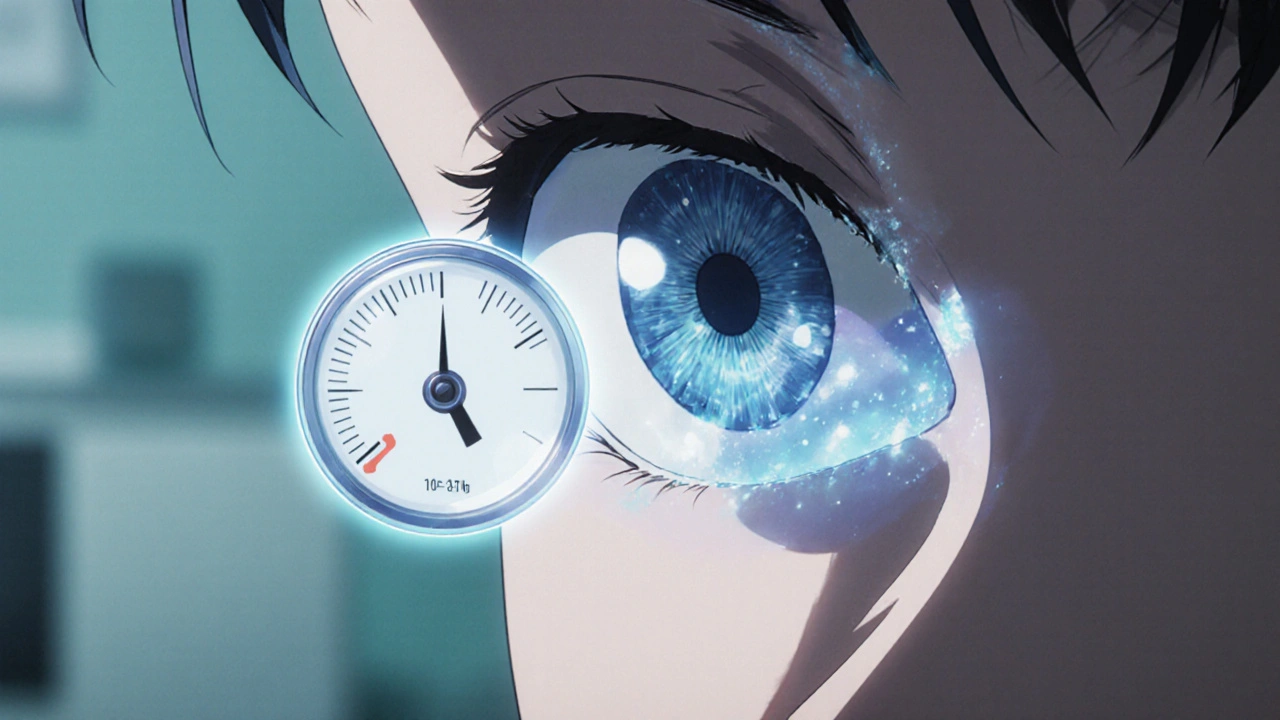
When it comes to protecting your vision, Intraocular Pressure is the fluid pressure inside the eye that keeps its shape and supports normal function is the first thing you should think about. Glaucoma is a group of eye diseases that damage the optic nerve, often because of elevated intraocular pressure (IOP). The link between the two is simple: higher IOP is the biggest risk factor for glaucoma, and catching pressure spikes early can mean the difference between a clear future and permanent vision loss. That’s why regular eye pressure checks are a cornerstone of glaucoma prevention.
What Is Intraocular Pressure?
IOP is measured in millimeters of mercury (mmHg). A healthy range typically sits between 10 and 21 mmHg. Anything consistently above 22 mmHg puts the optic nerve under stress, potentially leading to the characteristic “cupping” that signals glaucoma damage. The fluid behind the eye, called aqueous humor, is produced by the ciliary body and drains through a tiny meshwork called the trabecular meshwork. When production outpaces drainage, pressure builds up.
Why Intraocular Pressure Matters for Glaucoma
Glaucoma doesn’t announce itself with pain or obvious symptoms-most people notice vision loss only after significant damage has occurred. That silent progression is why doctors rely on IOP readings as an early warning system. A single high reading isn’t a diagnosis, but repeated spikes dramatically increase the odds of optic nerve injury.
Studies from the African Vision Research Institute (2023) show that for every 1 mmHg increase above 21, the risk of developing glaucoma rises by roughly 10 %. This risk is even steeper for people of African descent, who already face a two‑to‑three‑fold higher prevalence of the disease. Regular monitoring can catch those incremental rises before they become a permanent problem.
How Often Should You Get Checked?
The frequency of eye pressure checks depends on age, family history, and existing eye health. Here’s a quick guide:
- Under 40, no risk factors: Every 2‑3 years.
- 40‑60, family history of glaucoma: Annually.
- Over 60, or diagnosed with any eye condition: Every 6‑12 months.
- High‑risk groups (African descent, diabetes, thin corneas): Six‑monthly checks are advisable.
In Durban, many optometrists and ophthalmologists offer comprehensive eye exams that include IOP measurement as a standard part of the check‑up. If you’re unsure how often you need one, ask your eye‑care provider to assess your personal risk profile.
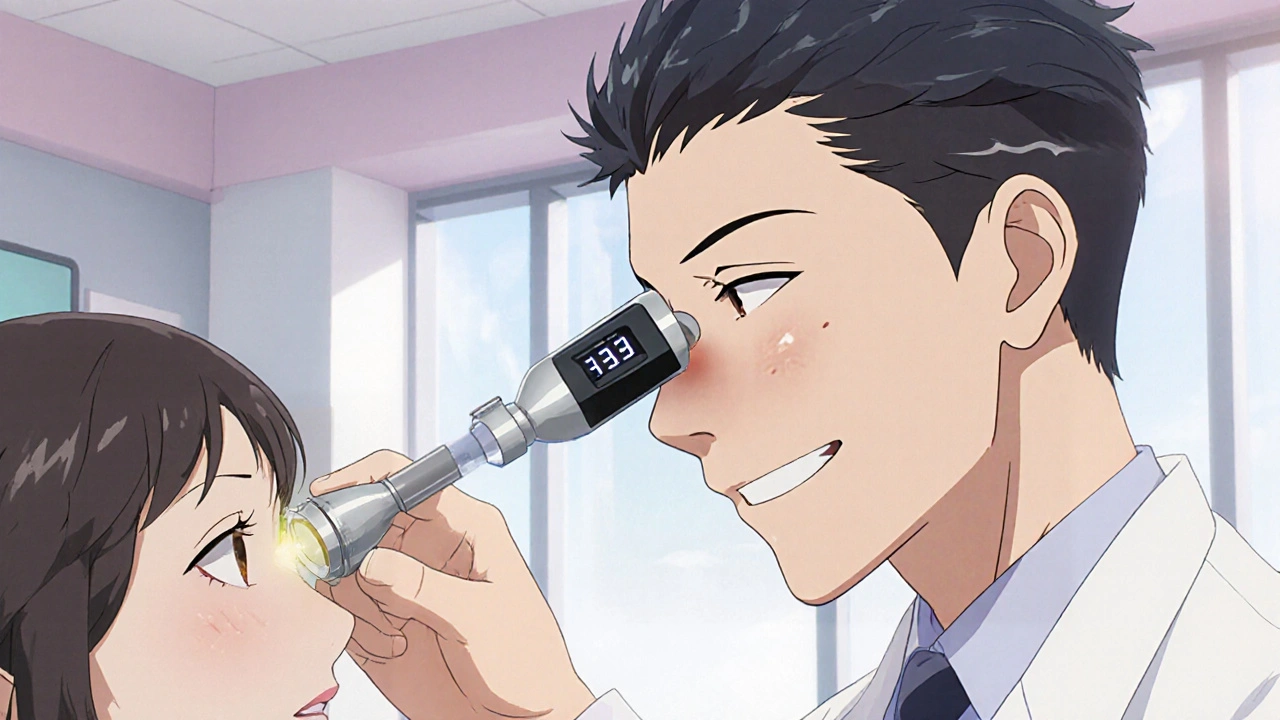
Common Methods of Measuring Eye Pressure
There are several tonometry techniques, each with its own pros and cons. Below is a quick comparison:
| Method | How It Works | Typical Accuracy | Patient Comfort |
|---|---|---|---|
| Goldmann Applanation | Flattens a tiny area of the cornea with a probe | ±1 mmHg (gold standard) | Requires numbing drops; mild discomfort |
| Non‑Contact (Air‑Puff) | Blasts a quick puff of air to flatten the cornea | ±2-3 mmHg | No contact; slight startling sound |
| Tonopen | \nHand‑held probe presses lightly on the cornea | ±2 mmHg | Minimal anesthesia; portable for clinics |
| Rebound (iCare) | Small probe bounces off the cornea | ±2-3 mmHg | Contactless; often used on children |
For most adults, the Goldmann applanation tonometer remains the most accurate, especially when tracking subtle changes over time. However, in busy community clinics across South Africa, the non‑contact method is popular because it’s quick and doesn’t require any eye drops.
Understanding Your Risk Factors
Besides high IOP, several other factors raise your glaucoma risk. Knowing them helps you and your Optometrist decide how aggressively to monitor your eyes.
- Family History: If a first‑degree relative has glaucoma, your odds double.
- Age: Risk climbs after 40 and spikes after 60.
- Ethnicity: People of African or Hispanic descent develop glaucoma earlier and more aggressively.
- Thin Corneas: Measured with pachymetry; thin corneas can underestimate true IOP.
- Medical Conditions: Diabetes, hypertension, and long‑term steroid use can all influence pressure.
- Eye Injuries: Trauma can damage drainage pathways.
In the KwaZulu‑Natal region, a 2024 population study showed that 18 % of adults over 50 have undiagnosed ocular hypertension-an alarming figure that underscores the need for routine checks.

What Happens After a High Reading?
If your IOP measurement comes back above the normal range, your eye‑care professional will usually recommend a series of follow‑up tests to assess damage:
- Visual Field Test: Checks for peripheral vision loss.
- Optical Coherence Tomography (OCT): Images the retinal nerve fiber layer (RNFL) to spot thinning.
- Gonioscopy: Examines the angle where fluid drains.
Based on these results, an Ophthalmologist may prescribe eye‑pressure‑lowering drops, laser therapy, or even surgery. The goal is always to bring the pressure back into a safe range and halt further optic nerve damage.
Tips for Maintaining Healthy Eye Pressure
While genetics play a big role, lifestyle choices can make a noticeable difference:
- Stay Active: Regular aerobic exercise (walking, cycling) can lower IOP by 2‑3 mmHg.
- Watch Your Caffeine: Too much caffeine may cause short‑term spikes.
- Limit Fluid Overload: Drinking large volumes quickly can raise pressure temporarily.
- Protect Your Eyes: Wear safety glasses during sports or work to avoid traumatic spikes.
- Adhere to Medications: If prescribed drops, use them exactly as directed.
Regular eye exams also give you a chance to discuss any new symptoms-like halos around lights or eye pain-with your eye professional before they become serious.
Frequently Asked Questions
How is intraocular pressure measured?
Most clinics use a Goldmann applanation tonometer, which gently flattens a tiny part of the cornea to read pressure in mmHg. Alternatives include non‑contact air‑puff devices, Tonopen, and rebound tonometers.
Can glaucoma be cured?
Glaucoma is currently irreversible, meaning any nerve damage is permanent. However, treatment can stop further loss, preserving the vision you still have.
Do I need a prescription to get my eye pressure checked?
No. In South Africa, both optometrists and ophthalmologists can perform tonometry as part of a routine eye exam, and you don’t need a prior prescription.
What are the side effects of eye‑pressure‑lowering drops?
Common side effects include mild eye irritation, a bitter taste, or blurred vision shortly after use. Rarely, some people develop allergic reactions; your doctor can adjust the formula if needed.
Is there a link between glaucoma and other diseases?
Yes. Diabetes, hypertension, and even sleep apnea have been linked to higher glaucoma risk. Managing these conditions helps keep eye pressure in check.
Bottom line: Regular eye pressure checks are a simple, cost‑effective way to catch glaucoma early. Pair those checks with a healthy lifestyle and prompt follow‑up care, and you give your eyes the best chance to stay sharp for years to come.

Chirag Muthoo
October 21, 2025 AT 18:10Intraocular pressure (IOP) measurement constitutes a cornerstone of preventive ophthalmology. By quantifying the fluid dynamics within the ocular globe, clinicians obtain a reliable surrogate marker for optic nerve stress. Repeated IOP readings over time enable the detection of subtle trends that may precede structural damage. The normal range of ten to twenty‑one millimetres of mercury is well established through decades of epidemiological research. Values persistently exceeding twenty‑two millimetres of mercury warrant closer scrutiny, especially in individuals with known risk factors. Early identification of ocular hypertension permits timely intervention, often with topical pharmacotherapy that can lower pressure by several millimetres of mercury. Moreover, lifestyle modifications such as regular aerobic exercise and moderated caffeine intake have been shown to exert modest pressures‑reduction effects. The Goldmann applanation tonometer remains the gold standard for accuracy, offering a measurement precision of plus or minus one millimetre of mercury. While alternative tonometers provide convenience, their inherent variability necessitates consistent use for longitudinal monitoring. For patients of African descent, the prevalence of glaucoma is disproportionately high, underscoring the importance of more frequent assessments. Clinical guidelines therefore recommend six‑monthly examinations for high‑risk groups, as opposed to the biennial schedule for low‑risk individuals. Incorporating IOP measurement into routine eye examinations ensures that any upward trajectory is captured before irreversible optic nerve fibre loss occurs. Ophthalmologists and optometrists alike bear the responsibility to educate patients about the significance of these numbers. Transparent communication about the meaning of a single elevated reading mitigates unwarranted anxiety while reinforcing adherence to follow‑up testing. Ultimately, diligent IOP surveillance represents a cost‑effective strategy to preserve visual function across the lifespan.
Jasmina Redzepovic
October 21, 2025 AT 18:27When you examine the trabecular outflow facility, the data clearly indicate that tonometric variance can be attributed to corneal biomechanical properties. The ocular hypertension cohort exhibits a statistically significant elevation in pachymetric readings, which in turn skews the apparent IOP values upward. Hence, clinicians must apply correction algorithms that factor in central corneal thickness to avoid over‑diagnosis. Moreover, the aqueous humour turnover rate, mediated by the ciliary body’s secretory function, introduces another layer of complexity that is often glossed over in superficial reviews. The literature unequivocally supports a risk stratification model that integrates genetical predisposition, IOP fluctuations, and ocular perfusion pressure. In practice, this translates to a protocol that mandates six‑monthly Goldmann applanation assessments for patients with a family history of primary open‑angle glaucoma. Failure to adhere to such a regimen may precipitate irreversible retinal nerve fibre layer thinning, as evidenced by longitudinal OCT cohorts. Finally, the economic implications of widespread non‑contact tonometry must be weighed against its convenience, especially in resource‑limited settings where the cost‑benefit ratio may not favour mass screening.
eric smith
October 21, 2025 AT 18:43Oh, because we all have the luxury of strolling into the clinic twice a year just to get a puff‑of‑air reading, right? Sure, let’s all pretend that a single high number means we need a lifetime of drops, laser, and surgery. The sarcasm is real when the “gold standard” is only guaranteed if you sit still and tolerate numbing drops. But hey, who needs perspective when you can have a catchy headline?
Eryn Wells
October 21, 2025 AT 19:00Hey everyone! 😊 Let’s remember that regular eye‑pressure checks aren’t just a medical recommendation – they’re a community‑care habit. 🌍 If you’re lucky enough to have access to an eye‑clinic, make that appointment and bring a friend along. 🙌 It’s especially important for those of us with family histories or who belong to higher‑risk groups. And don’t forget to ask your optometrist about the different tonometry options; some are quicker, some are more comfortable. 💡 A little knowledge goes a long way in keeping our vision bright for years to come.
Kathrynne Krause
October 21, 2025 AT 19:17Wow, what a fantastic reminder! 🎉 I love how this post breaks down the why and how of eye‑pressure monitoring in a way that actually fires you up to book that appointment. 🚀 Knowing that a simple test can spot trouble before it steals your sight is a game‑changer. Let’s all champion our eye health and spread the word – the more we talk about it, the fewer people will be caught off‑guard by glaucoma. Keep sharing these nuggets of wisdom, and let’s keep our world in focus! 🌟
Angela Koulouris
October 21, 2025 AT 19:33Your eyes are a precious window; treating them with care is essential. A steady routine of IOP checks builds a protective shield against hidden damage. If you ever feel uncertain, reach out to a trusted eye professional – they’re there to guide you. Remember, prevention is always simpler than correction, and small steps now lead to lasting clarity later.
erica fenty
October 21, 2025 AT 19:50IOP monitoring, essential; risk stratification, crucial; adherence, vital; check‑ups, regular; lifestyle, impactful; education, ongoing; outcomes, improved.
Xavier Lusky
October 21, 2025 AT 20:07They don’t tell you that the industry profits from over‑diagnosis.
Kimberly Lloyd
October 21, 2025 AT 20:23In the grand tapestry of our lives, vision is the thread that weaves moments together. Regular eye‑pressure checks are like gentle pauses that allow us to appreciate each stitch before any knot appears. By tending to our sight with quiet diligence, we honor the subtle beauty of the world around us and ensure that our inner landscapes remain clear and vibrant.