Contamination Controls: Preventing Adulteration in Generic Pharmaceuticals
 Dec, 22 2025
Dec, 22 2025
When you take a generic pill, you expect it to work just like the brand-name version. But behind that simple tablet is a complex battle against invisible threats-dust, microbes, chemical residues-that can turn a life-saving medicine into a dangerous one. Contamination control isn’t just a regulatory checkbox; it’s the line between a safe drug and a public health crisis.
Why Contamination in Generics Matters More Than You Think
Generic drugs make up 90% of all prescriptions filled in the U.S., but they account for only 22% of total drug spending. That means manufacturers are under intense pressure to cut costs. And when cost-cutting happens in the wrong place, contamination follows. The 2020 Valsartan recall wasn’t an accident-it was a warning. Nitrosamine impurities, formed during chemical synthesis, contaminated batches across 22 manufacturers. The result? $1.2 billion in losses, thousands of patients switched to alternative meds, and a global shake-up in how generics are made. The FDA doesn’t wait for disasters to act. In fiscal year 2022, 37.2% of all warning letters sent to pharmaceutical companies were for contamination violations. That’s more than any other single issue. It’s not about dirty floors. It’s about invisible particles, cross-contamination between drugs, and cleaning that looks good but doesn’t work.What Counts as Adulteration? The Legal Line
Under U.S. law (21 CFR 210.3(b)(3)), a drug is adulterated if it’s made, packed, or stored under conditions that could make it unsafe. That means even if every pill tests fine, if the environment where it was made wasn’t controlled, the whole batch is illegal. The FDA doesn’t need to find a contaminant in the final product to shut you down. They just need to prove the system failed. This isn’t theoretical. In 2022, the FDA issued a warning letter to Apotex Inc. for failing to prevent cross-contamination between two different drugs made in the same facility. The company didn’t have proper air pressure controls or cleaning validation. No one got sick. No one even knew there was a problem-until the FDA walked in.How Clean Is Clean Enough? The Numbers That Matter
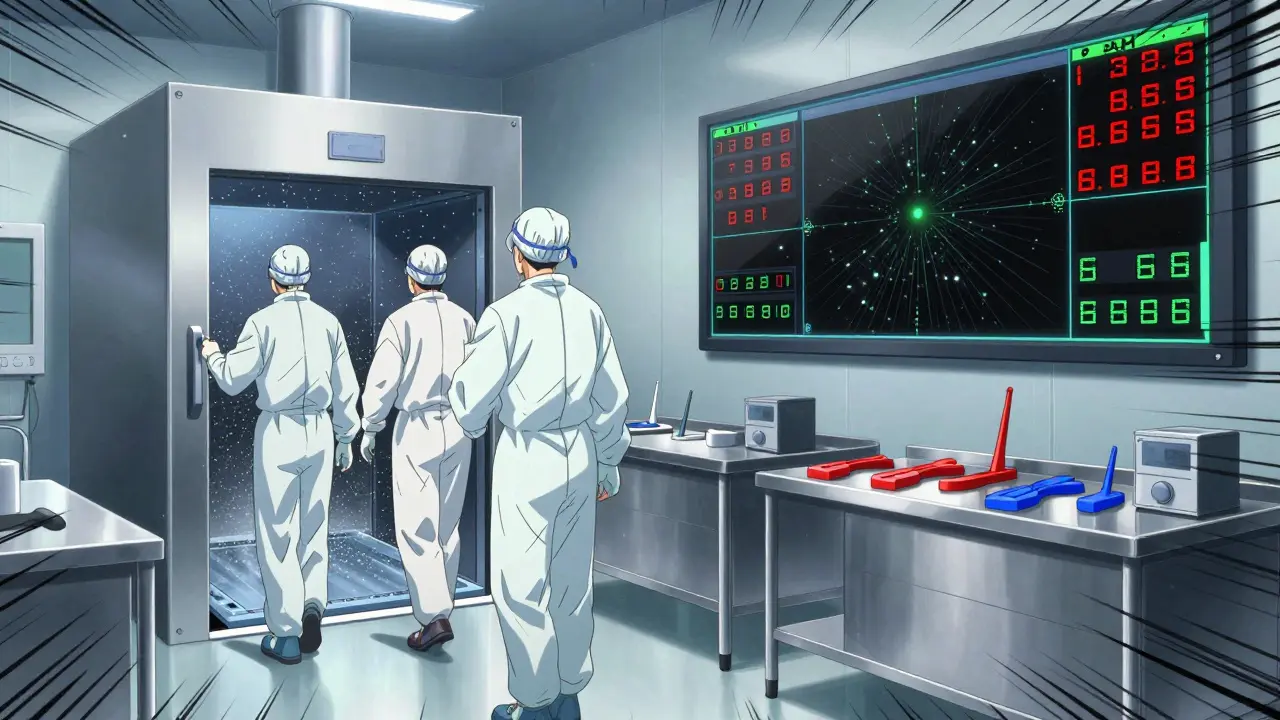
Cleanrooms aren’t just about white walls and lab coats. They’re engineered systems with strict particle limits. For sterile filling areas (like injectables), you need ISO Class 5-no more than 3,520 particles the size of a bacterium per cubic meter of air. That’s stricter than a hospital operating room. For non-sterile generics-think pills and capsules-you still need ISO Class 7 or 8 environments. But the real challenge isn’t the room. It’s what comes into it. People. Tools. Raw materials. Each one can carry contaminants. Cleaning validation sets the bar. You can’t just wipe a machine and call it clean. You have to prove it. The standard? Less than 10 colony-forming units (CFU) per 25 cm² surface for microbes. For chemical residues, it’s 10 parts per million (ppm)-or less, depending on the drug’s potency. That’s like finding one grain of salt in a full bathtub.Human Error Is the Biggest Contaminant
You can install the best filters, the cleanest hoods, the most advanced monitoring systems-but if your staff doesn’t gown properly, it all falls apart. A 2021 study at an AstraZeneca generics facility showed that gowning compliance dropped 40% after an 8-hour shift. People get tired. They skip steps. They touch their faces. They rush. And that’s when contamination spikes. Industry experts say 83% of contamination events trace back to human behavior. That’s why training isn’t optional. It’s a daily ritual. Color-coded equipment helps-red for Drug A, blue for Drug B. Staggered shift changes reduce traffic. Air showers before entering cleanrooms cut particle counts by up to 70%. One generic manufacturer reported a 30% spike in gowning failures after switching to reusable isolation gowns. The fix? A $185,000 investment in upgraded air showers. Not because the gowns were dirty-but because they weren’t being properly decontaminated between uses.
Technology Is Changing the Game
Old-school cleaning validation took five to seven days. You’d swab a surface, send it to a lab, and wait. By the time you got results, the batch was already shipped. Now, rapid microbiological methods (RMMs) give you results in 24 to 48 hours. ATP bioluminescence systems-those handheld devices that glow when they detect organic residue-give you a reading in five minutes. They’re 95% as accurate as lab cultures, and they let you stop production before a bad batch is made. Real-time particle counters like the MetOne 3400+ monitor air quality continuously. One 2022 ISPE study found facilities using them had 63% fewer contamination incidents. Manual checks? They miss 78% of transient events-like someone opening a door or a technician adjusting a machine. But these tools aren’t cheap. A single real-time monitor costs $15,000 to $25,000. Full systems run $500,000 to $2 million. That’s why only 89% of the top 50 generic manufacturers use them-and only 37% of smaller ones.One Batch at a Time: A Simple Fix That Works
Many generic manufacturers run multiple products on the same line to save money. One machine makes blood pressure pills, then switches to diabetes meds, then to antibiotics-all in one day. That’s risky. Even with cleaning, traces can linger. That’s why some facilities switched to the “one batch at a time” model. They dedicate a line to one drug. No switching. No cleaning between batches. No chance of cross-contamination. A case study in Pharmaceutical Engineering showed this approach cut cross-contamination incidents by 53%. It costs more in equipment and space-but it saves money in recalls, retests, and regulatory headaches.The New Rules: Health-Based Exposure Limits (HBELs)
By 2025, every generic manufacturer must calculate a Health-Based Exposure Limit (HBEL) for every product they make. That’s the maximum amount of a contaminant a person can safely be exposed to over a lifetime. This isn’t about cleaning better. It’s about understanding risk. A potent cancer drug might need a limit of 1 nanogram per square centimeter. A vitamin? Maybe 10,000 nanograms. You can’t use the same cleaning standard for both. The FDA’s September 2023 draft guidance makes HBELs mandatory. The cost? Around $1.2 million per facility to implement. For small manufacturers, that’s a huge burden. But the alternative-being shut down or losing market access-is worse.
What’s Next? AI, Sustainability, and Harmonization
AI is starting to predict contamination before it happens. Honeywell’s Forge Pharma system, tested at a Merck generics plant, cut false alarms by 68%. Instead of shutting down production for every spike, it tells you which ones matter. Sustainability is also driving change. Waterless cleaning technologies-using vaporized hydrogen peroxide or dry ice blasting-are cutting utility costs by 22%. GlaxoSmithKline’s pilot showed these methods work just as well as traditional washing, without the waste. And globally, regulators are moving toward alignment. ICH Q13, finalized in June 2023, integrates contamination controls into continuous manufacturing-a new way of making drugs that’s faster, cheaper, and requires tighter controls than batch production.Can Small Manufacturers Survive?
The truth is brutal. The cost of compliance is rising fast. Facilities that don’t invest in real-time monitoring, HBELs, and proper training will get caught. The FDA is increasing inspection frequency by 27% for companies with past violations. The EMA rejected 41% of generic applications in 2022 due to contamination issues. But it’s not impossible. The key isn’t doing everything. It’s doing the right things. Focus on human behavior. Use simple tools like color-coding and Dycem CleanZone mats (which reduce foot-borne contamination by 72%). Start with one high-risk product. Build your system around risk-not perfection. The cheapest way to prevent adulteration isn’t buying new machines. It’s training your team to care. Because no matter how clean the room is, if the person in it doesn’t follow the rules, the drug isn’t safe.What Happens If You Don’t Act?
One contamination event can cost millions. One warning letter can trigger a cascade of inspections. One recall can destroy trust. Generic manufacturers don’t compete on brand loyalty. They compete on price, reliability, and safety. If your product is seen as risky, buyers-hospitals, pharmacies, government agencies-will walk away. And once that happens, it’s nearly impossible to come back. The future belongs to those who treat contamination control like a core competency-not a compliance burden.What is considered adulteration in generic drug manufacturing?
Adulteration occurs when a drug is prepared, packed, or held under unsanitary conditions that could cause contamination with filth or make it injurious to health. This includes cross-contamination between drugs, microbial growth, chemical residues above safe limits, or particles from uncontrolled environments-even if the final product tests clean.
How often do contamination violations happen in generic drug manufacturing?
In 2022, contamination-related violations accounted for 37.2% of all FDA Warning Letters issued to pharmaceutical manufacturers. This makes it the single most common reason for regulatory action. One in three generic manufacturers experienced at least one contamination-related batch rejection in the past year, according to a 2023 PDA survey.
What’s the difference between contamination control for brand-name and generic drugs?
Brand-name manufacturers often spend $185 million or more on facility design to prevent contamination. Generic manufacturers, operating on tighter margins, rely more on procedural controls-strict cleaning protocols, staff training, and risk-based monitoring. While brand-name companies build physical barriers into their facilities, generics must build them into their processes.
Is real-time monitoring worth the cost for small generic manufacturers?
It depends. Real-time particle and microbial monitors reduce contamination incidents by 63% and cut investigation time by half. But they cost $500,000 to $2 million to install. For small facilities, starting with targeted use-like on high-risk lines or during validation runs-can provide value without full-scale investment. The key is using data to prioritize where to spend.
What’s the biggest mistake generic manufacturers make in contamination control?
Relying on end-product testing alone. The FDA explicitly states this is a violation under 21 CFR 211.110(a). You can’t test contamination out of a product after it’s made. Prevention must be built into the process-from facility design to staff behavior to cleaning validation.
What’s the easiest way to reduce contamination right now?
Start with Dycem CleanZone mats at entry points. They reduce foot-borne contamination by 72% based on real facility data. Combine that with color-coded equipment and a daily 10-minute gowning checklist. These low-cost changes have the highest ROI and are immediately actionable.
What’s the 2025 deadline for contamination controls, and why does it matter?
By 2025, all generic manufacturers must implement Health-Based Exposure Limits (HBELs) for every product, as required by FDA draft guidance. HBELs determine how clean a surface must be based on the toxicity of the drug residue. Missing this deadline risks regulatory action, facility shutdowns, and loss of market access. It’s not optional-it’s existential.
Next Steps for Manufacturers
If you’re running a generic drug facility, here’s what to do now:- Identify your highest-risk products-those with potent APIs or high exposure potential.
- Calculate or obtain HBELs for those products. Don’t wait for the FDA to ask.
- Map your cleaning validation process. Are you using real-time data or old lab results?
- Review your gowning compliance logs. Is there a drop-off after 8 hours?
- Install Dycem mats at all cleanroom entrances. It’s under $10,000 and has proven results.
- Train your team on why contamination control isn’t about rules-it’s about protecting patients.

Adarsh Dubey
December 23, 2025 AT 10:05The FDA is overreaching. If a pill works and doesn't kill anyone, why are we spending millions on air showers and color-coded gowns? This isn't rocket science. We're turning medicine into a luxury good while people go without because it's too expensive.
Paula Villete
December 25, 2025 AT 08:38So let me get this straight-we’re spending $2 million on real-time monitors so we don’t have to trust our workers… but we’re still paying them minimum wage to gown up for 8-hour shifts? And we’re shocked when they stop caring?
Maybe the real contamination is in our priorities. We optimize for profit, then panic when the system designed for profit fails. The fix isn’t more tech-it’s paying people enough to care.
Usha Sundar
December 26, 2025 AT 07:10Dycem mats work. Just install them.
claire davies
December 26, 2025 AT 10:24What strikes me most isn’t the tech or the regulations-it’s the quiet dignity of the people who show up every day to gown up, swab surfaces, and watch air counters like they’re guarding a sacred space.
These aren’t just factory workers. They’re the unsung pharmacists of our modern age. They don’t get medals, but they’re the reason your insulin doesn’t come laced with someone else’s chemotherapy residue.
And yet we treat them like disposable cogs. We cut training hours, reuse gowns without proper decon, and call it ‘efficiency.’
It’s not a cost center. It’s a covenant. We promise patients safety. They promise us their labor. But who’s keeping their side of the bargain?
siddharth tiwari
December 27, 2025 AT 21:14you think this is about safety? nah. its about big pharma pushing out small guys. the fda is just their puppet. why do you think only 89% of top 50 use the fancy monitors? because the little guys cant afford to be framed. theyll shut down a plant over 1 cfu and say ‘see? unsafe!’ while the big boys get waivers. its all rigged. and dont get me started on HBELs-thats just a fancy way to say ‘pay us more or go away’.
Georgia Brach
December 28, 2025 AT 04:53Let’s not romanticize this. The ‘one batch at a time’ model is economically unsustainable. It’s a boutique solution for a mass-market problem. You can’t run 500 different drugs on 500 dedicated lines and still sell pills for $2. This isn’t a quality issue-it’s a market failure. We’ve commoditized medicine so thoroughly that we’ve made compliance impossible without subsidies or monopolies. The real adulteration is in the economic model.
Diana Alime
December 28, 2025 AT 16:51so like… i just read this whole thing and my brain is like ‘wait, so we’re paying $25k for a machine that glows if there’s a speck of dust… but we’re still letting people touch their faces in the cleanroom?’
why are we doing this like it’s a sci-fi movie and not a pharmacy? we’re not building a spaceship. we’re making aspirin. can we just… not overcomplicate this? someone’s gonna die because someone didn’t wash their hands. not because the air had 3521 particles.
Bartholomew Henry Allen
December 29, 2025 AT 06:23Adarsh Dubey’s comment is dangerously naive. This isn’t about cost. It’s about national security. A contaminated generic drug is a biological weapon in the hands of foreign manufacturers. The U.S. cannot afford to rely on foreign supply chains with lax standards. The FDA’s actions are not overreach-they are essential defense. If you don’t understand that, you don’t understand America.