COPD Explained: Understanding Disease Stages and Treatment Options
 Jan, 5 2026
Jan, 5 2026
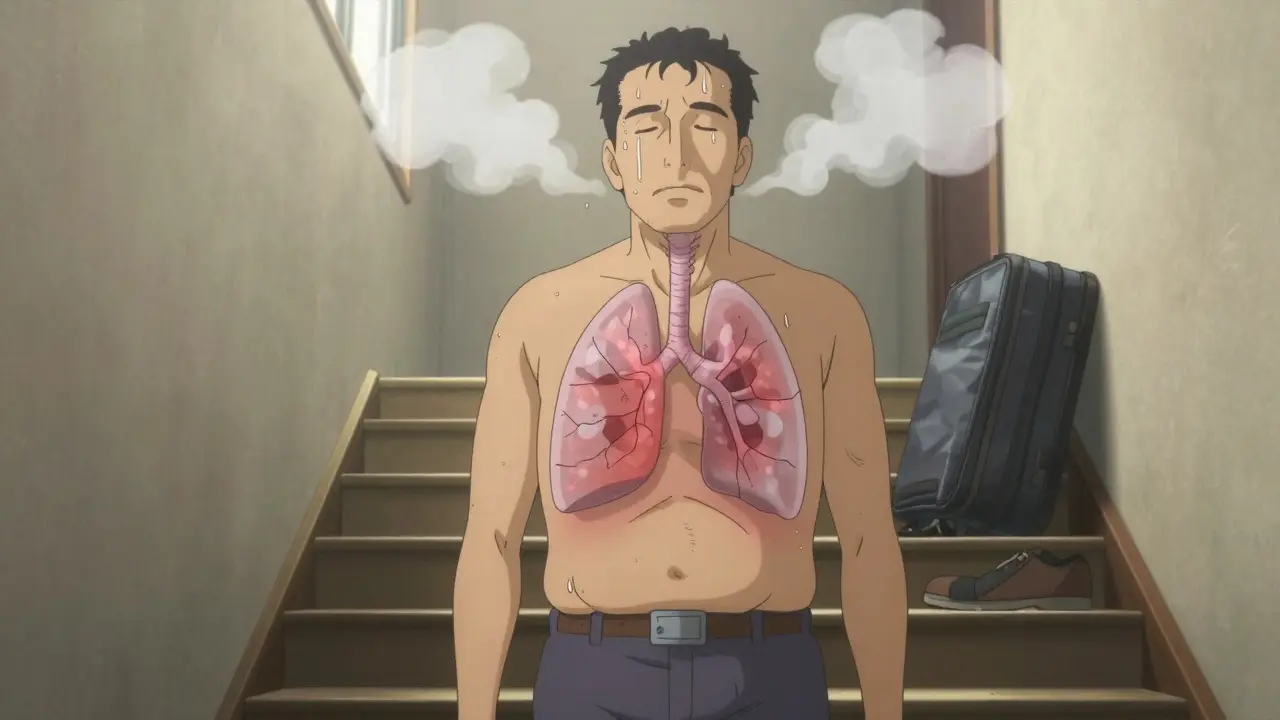
Chronic Obstructive Pulmonary Disease, or COPD, isn’t just a cough that won’t go away. It’s a serious, progressive lung condition that slowly steals your ability to breathe - and many people don’t realize they have it until it’s advanced. Around 380 million people worldwide live with COPD, and it’s the third leading cause of death globally. In the U.S. alone, it costs Medicare $29 billion a year. But here’s the truth: if you catch it early, you can slow it down. A lot. And if you’re already in later stages, there are still ways to feel better, stay out of the hospital, and keep doing the things you love.
What Exactly Is COPD?
COPD isn’t one disease - it’s a group of lung problems that make it hard to breathe. Most often, it includes chronic bronchitis (inflamed airways with lots of mucus) and emphysema (damaged air sacs that can’t hold air properly). The main cause? Smoking. About 85 to 90% of cases are directly linked to cigarette smoke. But it’s not just smokers. Long-term exposure to air pollution, dust, chemicals, or secondhand smoke can also trigger it. And in rare cases, a genetic condition called alpha-1 antitrypsin deficiency plays a role.
What makes COPD dangerous is how quietly it creeps in. People often think shortness of breath when climbing stairs or a persistent morning cough is just part of getting older. They don’t go to the doctor. By the time they do, their lungs may already be significantly damaged. The only way to know for sure is a simple breathing test called spirometry.
How COPD Is Staged: The GOLD System
Doctors don’t just guess how bad your COPD is. They use a system called GOLD - Global Initiative for Chronic Obstructive Lung Disease - updated in 2023. It’s not just about lung numbers. It’s about how you feel and how often you get sick.
The first part is spirometry. It measures how much air you can blow out in one second - called FEV1. This number is compared to what’s normal for someone your age, height, and gender. Based on that, COPD is broken into four stages:
- Stage 1 (Mild): FEV1 is 80% or higher of normal. You might have a cough with phlegm, especially in the morning. You get winded during intense exercise, but you probably think it’s just because you’re not in shape. Many people here don’t even know they have COPD.
- Stage 2 (Moderate): FEV1 drops to 50-79%. Now, breathing becomes a problem during everyday activities - walking to the mailbox, doing dishes, or shopping. You might need to stop every few minutes to catch your breath. This is the stage where most people finally go to the doctor.
- Stage 3 (Severe): FEV1 falls to 30-49%. Breathing is hard even with light effort. Getting dressed, cooking a meal, or taking a shower can leave you gasping. You start having flare-ups - called exacerbations - more often. These can land you in the hospital.
- Stage 4 (Very Severe): FEV1 is below 30%, or below 50% with low oxygen in your blood. You’re short of breath even at rest. You might need oxygen around the clock. Simple tasks like brushing your teeth can exhaust you. Your body starts to struggle, and complications like blue lips, confusion, or heart strain become more common.
But here’s the twist: two people with the same FEV1 number can feel totally different. One might be barely affected. The other might be housebound. That’s why the GOLD system also looks at symptoms and how often you get sick. Patients are grouped into A, B, C, or D based on:
- How bad your symptoms are (measured by a short questionnaire)
- How many times you’ve been hospitalized for flare-ups in the past year
Group A: Few symptoms, low risk of flare-ups. Group D: Lots of symptoms, high risk. Your group tells your doctor what treatment to start with.

Treatment by Stage: What Actually Works
There’s no cure for COPD. But treatment isn’t about fixing your lungs - it’s about helping you live better with them. What works depends on your stage and your group.
Stage 1: Catch it early, change your life
If you’re in Stage 1, the single most powerful thing you can do is quit smoking. Studies show quitting cuts the rate of lung decline by half. That’s not a small win - it’s the difference between needing oxygen in 10 years versus 20. Short-acting inhalers like albuterol can help if you’re wheezing after exercise, but they’re not daily medicine. Focus on prevention: get the flu shot every year. Get the pneumonia vaccine. Stay active. Walk every day. Your lungs don’t need to be perfect - they just need to be used.
Stage 2: Start the routine
At this stage, you’ll likely be prescribed a long-acting inhaler - either tiotropium (Spiriva) or salmeterol (Serevent). These work for 12 to 24 hours and keep your airways open all day. You’ll also be referred to pulmonary rehab. This isn’t just exercise. It’s a 8- to 12-week program where you learn breathing techniques, how to use your inhalers correctly, and how to move without getting winded. People who complete rehab walk 54 meters farther on a 6-minute test - that’s the distance from your front door to your car. That’s independence.
And yes, get the flu shot. Again. And the pneumonia shot. If you’re still smoking, now’s the time to get help. Nicotine patches, counseling, or medications like varenicline can double your chance of quitting.
Stage 3: Managing the flare-ups
Now you’re on combination therapy - usually two long-acting inhalers together (LAMA + LABA). If you’ve had two or more flare-ups in a year, your doctor will add an inhaled steroid. This reduces swelling and lowers your chance of hospital visits by 37%, according to a 2022 study in JAMA.
Supplemental oxygen may be needed if your blood oxygen drops below 88% at rest. Many people resist this, thinking it means they’re “done.” But oxygen isn’t giving up - it’s letting you live. You can still walk, travel, and spend time with family. Portable oxygen units have gotten smaller. Some even work on battery power for 4 to 6 hours.
Don’t ignore your mental health. Anxiety and depression are common at this stage. Talking to a counselor or joining a support group helps more than you’d think.
Stage 4: Living with limited air
Continuous oxygen therapy (15+ hours a day) is the standard. Studies show this can improve survival by 44% if your oxygen is very low. You’ll likely need a home oxygen concentrator and a portable unit for outings.
If you’re under 65 and otherwise healthy, lung volume reduction surgery might be an option. It removes the most damaged parts of your lungs, letting the healthier parts work better. One trial showed a 15% improvement in 2-year survival.
Lung transplant is the last resort - only for those under 65 with FEV1 under 20%. It’s complex, expensive, and requires lifelong immune-suppressing drugs. But for some, it’s the only way to breathe freely again.
The Real Challenges: What No One Talks About
Medications cost a lot. Spiriva can run $350 to $400 a month without insurance. Many people skip doses because they can’t afford them. Some drug companies offer assistance programs - ask your pharmacist.
Inhaler technique? Most people use them wrong. One study found 70 to 80% of COPD patients make mistakes - pressing the canister too early, not holding their breath, not rinsing after steroids. A single 10-minute session with a respiratory therapist can fix this.
And oxygen? It’s life-saving, but it’s also limiting. Most portable tanks last 4 to 6 hours. You can’t leave home for long without planning. Battery life matters. You need backup tanks. And you’ll learn to live with the tubing, the noise, the stares.
Worst of all? Many doctors don’t talk about what’s coming. They focus on inhalers and oxygen, but not on end-of-life planning. Advance directives, hospice options, and comfort care aren’t signs of giving up - they’re tools to keep you in control.

What’s New in COPD Care (2026)
Treatment isn’t standing still. In 2023, the FDA approved Breztri Aerosphere - a single inhaler that combines three medications. No more juggling three different devices. That’s a game-changer for adherence.
New drugs like ensifentrine are in late-stage trials. Early results show a 13% improvement in lung function - better than most existing meds.
And technology? Apps like Kyna COPD use AI to predict flare-ups by tracking your cough, breathlessness, and sleep patterns. It’s 82% accurate. If your phone tells you a flare-up is coming, you can start steroids early - and avoid the hospital.
Researchers are also looking at genetics. The COPDGene study found 82 gene variants linked to how fast COPD progresses. In the future, treatment might be tailored to your DNA - not just your FEV1.
What You Can Do Today
Whether you’re in Stage 1 or Stage 4, here’s what works:
- Quit smoking - no exceptions. It’s the only thing that changes your disease’s path.
- Get vaccinated - flu, pneumonia, and COVID-19. Every year.
- Do pulmonary rehab - even if you think you’re too tired. It works.
- Learn your inhaler - ask for a demo from your pharmacist or nurse.
- Track your symptoms - write down when you feel worse. It helps your doctor adjust your treatment.
- Connect with others - the COPD Foundation has local support groups and a 25,000-member online community. You’re not alone.
- Plan ahead - talk to your family about what you want if things get worse. It’s not morbid. It’s empowering.
COPD doesn’t have to be a death sentence. It’s a chronic condition - like diabetes or high blood pressure. You manage it. You live with it. And with the right tools, you can still live well.

Katelyn Slack
January 5, 2026 AT 17:15i just found out my dad has stage 2 copd and honestly i had no idea it was this serious. i always thought it was just "smokers cough". now i get why he’s always so tired. thanks for explaining the stages so clearly.
Melanie Clark
January 5, 2026 AT 19:04they’re lying to you about copd its not just smoking its the fluoridated water and the 5g towers poisoning your lungs they dont want you to know the truth the pharmaceutical companies are making billions off your suffering
Harshit Kansal
January 6, 2026 AT 10:57my uncle in delhi has copd and he still smokes 20 cigarettes a day. he says its his only joy left. i told him to quit but he just laughs. its sad but also kind of brave in a messed up way.
Saylor Frye
January 7, 2026 AT 16:07the gold system is outdated. they’re still using fev1 like its 2005. real medicine now looks at exhaled nitric oxide levels, cytokine profiles, and microbiome shifts. if your doctor hasn’t mentioned these, they’re practicing paleomedicine.
Tiffany Adjei - Opong
January 8, 2026 AT 03:38you say quitting smoking is the only thing that helps but what about all the non-smokers with copd? what about the factory workers? the people breathing diesel fumes for 30 years? you’re blaming the victim. this whole post is just corporate propaganda dressed up as medical advice.
Lily Lilyy
January 9, 2026 AT 02:22you can do this. even if you’re in stage 4, your spirit is stronger than your lungs. take one breath at a time. every step you take, every smile you give, every hug you hold-that’s your victory. you are not defined by your fev1. you are loved. you are enough.
Mukesh Pareek
January 9, 2026 AT 19:53the pharmacokinetic profile of inhaled corticosteroids in copd patients demonstrates suboptimal bronchial deposition due to altered airflow dynamics, particularly in group d phenotypes. adjunctive therapy with phosphodiesterase-4 inhibitors may modulate neutrophilic inflammation more effectively than lama/laba monotherapy.
Ashley S
January 10, 2026 AT 01:03why are we even talking about this? no one cares about copd unless it’s you or your grandpa. they’re just giving people inhalers so they can keep working instead of paying them disability. this whole system is rigged.
Gabrielle Panchev
January 11, 2026 AT 13:24you mentioned that 70-80% of people use inhalers incorrectly-but did you ever consider that maybe the inhalers are designed poorly? why do they require such precise coordination between pressing and inhaling? why not make a simple, breath-actuated device that works for everyone? this isn’t rocket science, it’s lazy engineering. and then they charge $400 a month for it. it’s criminal.
Katie Schoen
January 13, 2026 AT 07:22my mom’s on oxygen and she still dances in the kitchen while making soup. she says the tubing is just her new fashion accessory. honestly? she’s the most alive person i know. if you’re breathing, you’re still winning.
Stuart Shield
January 14, 2026 AT 00:39i used to work in a coal town in wales. saw a lot of men with copd. they’d sit on their porches, coughing like a broken engine, but they’d still wave at neighbors, tend their roses, tell jokes. there’s dignity in that. it’s not about fixing the lungs-it’s about honoring the person inside them.
Indra Triawan
January 14, 2026 AT 18:58isn’t it ironic that we treat copd like a medical problem when it’s really a spiritual one? our lungs are the mirror of our breath, and our breath is the mirror of our soul. when we ignore our inner silence, our bodies scream back through wheezes and gasps. perhaps the real cure is not in inhalers, but in stillness.
Susan Arlene
January 15, 2026 AT 18:25my cousin quit smoking after 40 years and now she walks 2 miles every morning. she says her lungs feel like they finally remember how to breathe. it took her a year to stop coughing but she says it was worth it. just saying.
Tom Swinton
January 17, 2026 AT 00:10I just want to say-this post is so important. I’ve been in stage 3 for three years now, and I didn’t know about pulmonary rehab until last month. I did the program, and I can tell you-it changed everything. I’m not cured, but I’m not helpless anymore. I can carry my groceries. I can play with my grandkids without stopping. If you’re reading this and you’re scared, don’t be. Just take the first step. Ask your doctor. Show up. You’re not alone. I’m right here with you.