Generic Manufacturing Standards: How Quality Control Stops Counterfeit Drugs
 Dec, 16 2025
Dec, 16 2025
Every pill you swallow should work the way it’s supposed to. But in some places, up to 30% of medicines sold are fake. These aren’t just poor copies-they’re dangerous. They might have no active ingredient, the wrong dose, or toxic fillers. And while brand-name drugs get all the attention, generic drugs are the backbone of global healthcare-making up 90% of prescriptions in the U.S. alone. So how do we make sure they’re safe? The answer isn’t luck. It’s quality control built into every step of manufacturing.
Why Quality Can’t Be Tested at the End
You can’t inspect safety into a medicine. That’s the first rule of modern drug manufacturing. If a pill looks right, smells right, and passes a quick lab test, it doesn’t mean it’s safe. Counterfeiters have gotten good at copying the look and chemical makeup of real drugs. Some even replicate the exact active ingredient-but use the wrong crystal form. That tiny difference can mean the drug doesn’t dissolve properly in your body. You take it. Nothing happens. You get sicker. And you never know why. The U.S. Food and Drug Administration (FDA) says it plainly: “Quality cannot be tested into a finished product; it must be built into the design and manufacturing process at every single step.” That’s why the system isn’t about checking pills at the end. It’s about controlling everything before, during, and after production.The SQUIPP Framework: What Really Matters
Generic drug makers don’t just follow rules-they follow a science-backed framework called SQUIPP: Safety, Quality, Identity, Potency, and Purity. Each letter stands for a non-negotiable requirement.- Identity: Does this pill contain the right drug? Not just the right molecule, but the right form. Infrared spectroscopy and high-performance liquid chromatography (HPLC) are used to verify this with 99.9% accuracy.
- Potency: Does it have the right amount? Too little? It won’t work. Too much? It could kill. Dissolution testing checks how quickly the drug releases in simulated body fluid-must hit 80% within 30 to 45 minutes.
- Purity: Are there harmful impurities? In 2018, a batch of valsartan (a blood pressure drug) was recalled because a carcinogen formed during manufacturing. Standard tests missed it. Now, labs use mass spectrometry to catch even trace contaminants.
- Safety & Quality: Is the environment clean? Is the equipment sterilized? Is every batch documented? Clean rooms must meet ISO Class 5 standards-fewer than 3,520 particles per cubic meter. That’s like having a sterile operating room for every batch.
How Digital Systems Block Counterfeits
Physical testing alone isn’t enough. Counterfeiters can fake lab results. So now, every package gets a digital fingerprint. Under the U.S. Drug Supply Chain Security Act, every medicine package must have a unique serial number. That number is scanned at every point-from the factory to the pharmacy. If a package shows up twice, or never shows up at all, the system flags it. This track-and-trace system works with 99.99% accuracy. Most major manufacturers now use cloud-based Electronic Quality Management Systems (eQMS). These platforms track over 15,000 quality data points per batch in real time. One quality manager at Teva told a forum: “Our eQMS cut deviation resolution from two weeks to two days.” But it cost $2.3 million and took 18 months to set up. Smaller companies struggle with the price-$500,000 to $1 million just for one spectrometer.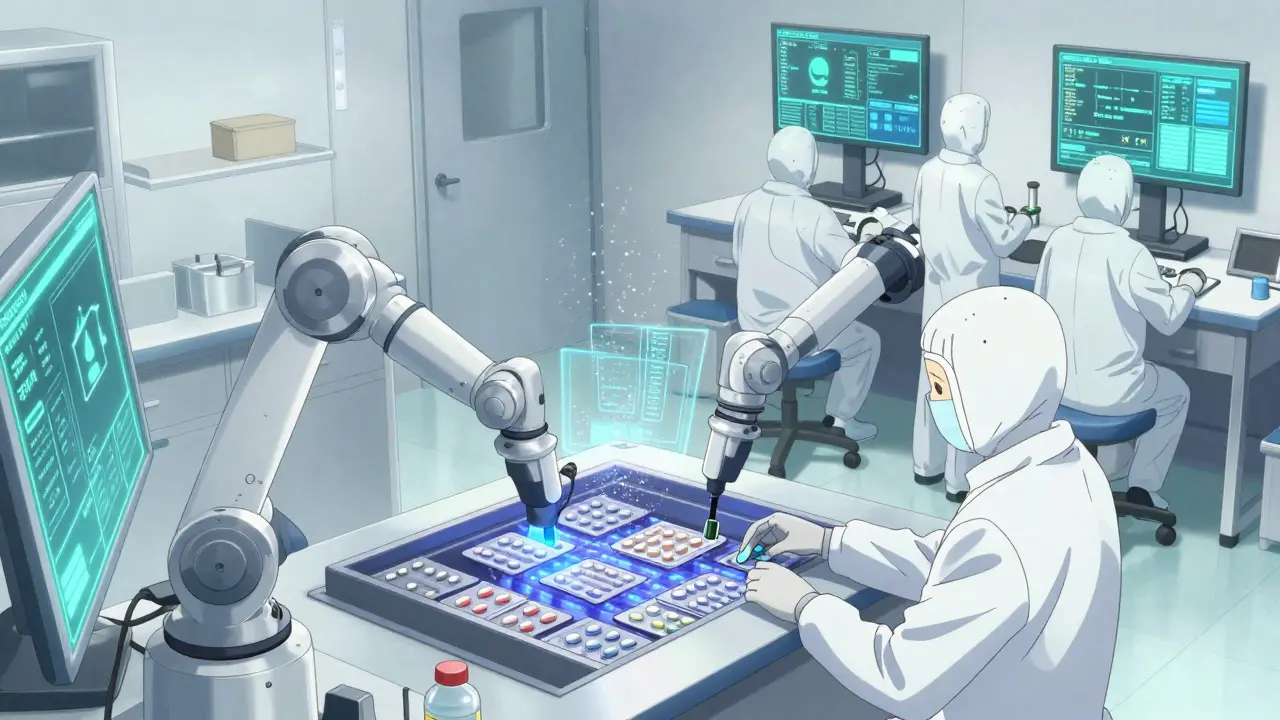
Why Generic Drugs Are Held to the Same Standard as Brand-Name
There’s a myth that generic drugs are “lesser.” They’re not. The FDA requires them to prove they’re bioequivalent to the brand-name version. That means their absorption rate in the body must fall within 80-125% of the original. In some countries, the range is wider-75-133%. That’s why generics from unregulated markets are risky. The data shows it works. FDA-regulated generic drugs have a 0.02% adverse event rate. Brand-name drugs? 0.03%. The difference is statistically meaningless. The only reason generics are cheaper is because they don’t pay for advertising or patent research. The manufacturing standards? Identical.Where the System Still Fails
The system works well in the U.S., Canada, and the EU. But globally? It’s uneven. In 2022, Interpol seized $21 million in fake medicines during Operation Pangea X. Seventy-eight percent were falsely labeled as generics. Most came from unregulated factories in Asia and Africa. The FDA found only 78% compliance among Indian manufacturers and 65% in China. In contrast, U.S. facilities had 94% compliance. Even in regulated markets, problems linger. The most common FDA inspection failures? Inadequate investigation of out-of-spec results (37% of warning letters) and poor cleaning validation (29%). One lab might test a batch and say it’s fine. But if they don’t ask why a result was weird in the first place, the problem keeps happening.What’s Next: AI, Blockchain, and Molecular Tags
The fight against counterfeits is getting smarter. The FDA is investing $150 million in advanced detection tech by 2027. Companies like IBM and Siemens are pouring $1.2 billion into AI-driven quality systems that spot anomalies in real time. In Africa, the WHO is testing blockchain to verify antimalarial drugs. Farmers and clinics scan a code on the package. If it’s real, the system confirms it. If not, it alerts authorities. Future systems may use molecular taggants-tiny, invisible markers added during manufacturing that can’t be copied without knowing the exact chemical recipe. Quantum-resistant encryption for serial numbers is already required in the EU by 2026. But tech alone won’t fix this. It needs enforcement. Training. Accountability. Right now, 8-12% of a generic drug’s cost goes to quality control. That’s expensive. But not as expensive as a dead patient.What You Can Do
If you’re a patient: Buy from licensed pharmacies. Avoid websites that sell pills without a prescription. If the price seems too good to be true, it probably is. If you’re in healthcare: Demand transparency. Ask your pharmacy where their generics come from. Support policies that fund global regulatory capacity. If you’re in manufacturing: Don’t cut corners on documentation. Train your team. Invest in eQMS. The cost is high, but the cost of failure is worse.Final Thought: Trust Is Built, Not Bought
Counterfeit drugs thrive where oversight is weak. They disappear where systems are tight. The truth is, we already have the tools. We know how to make safe generics. We’ve done it for decades. The question isn’t whether we can stop counterfeits. It’s whether we have the will to make sure every pill, everywhere, meets the same standard.It’s not about brands. It’s about lives.

Joe Bartlett
December 18, 2025 AT 08:03Man, I don't get why Americans act like they invented medicine. We've had clean generics in the UK for decades. You just need to enforce the rules, not throw money at tech.
Anu radha
December 19, 2025 AT 04:43I work in a pharmacy in India. We get fake pills all the time. People think cheap is good. But sometimes, cheap kills.
Sachin Bhorde
December 20, 2025 AT 23:39Bro the SQUIPP framework is legit. We use HPLC + MS at my lab. If your dissolution profile ain't hitting 80% in 45 min, you're not even in the game. And yeah, those eQMS systems? Total game-changer. One client went from 200 deviations/month to 12. Life changed.
Jigar shah
December 22, 2025 AT 08:31Interesting that you mention crystal form. I read a paper last year where a generic gabapentin had the wrong polymorph. Patients reported no effect. The lab missed it because they only tested for the molecule, not the structure. That's scary.
Josh Potter
December 24, 2025 AT 01:19Y’all are overthinking this. Just scan the damn QR code. If it’s real, you’re good. If it’s not, report it. Simple. No need for $2 million systems. People just need to care.
Marie Mee
December 24, 2025 AT 01:39They're lying about the 0.02% adverse rate. The FDA hides the real numbers. I know someone who had a stroke from a generic blood pressure pill. They buried the report. Big Pharma owns the FDA. Always has.
Evelyn Vélez Mejía
December 25, 2025 AT 21:40What we're really discussing isn't chemistry or compliance-it's moral architecture. The pill is a sacrament of trust. When we permit the erosion of quality control, we don't just risk health-we unravel the social contract between healer and healed. The manufacturing floor is a cathedral. And we are its priests.
Steven Lavoie
December 27, 2025 AT 00:01It’s easy to say 'trust the system' when you’re in the U.S. But in rural India, Kenya, or Bolivia, patients have no way to verify what they’re taking. The tech exists-but it’s not deployed equitably. That’s not a failure of science. It’s a failure of justice.
BETH VON KAUFFMANN
December 28, 2025 AT 08:16Let’s be real-90% of generic manufacturers are cutting corners. The FDA inspections are a joke. They show up, get a tour, get handed curated data. Real compliance? Maybe 50%. And don’t get me started on the 'bioequivalence' loophole. 80-125%? That’s a 56% swing. That’s not medicine. That’s roulette.
Victoria Rogers
December 29, 2025 AT 02:35Why are we even talking about generics? Brand-name drugs are just overpriced monopolies. If you want safe medicine, go to Canada. Or better yet, don't take pills at all. Your body can heal itself. The system is rigged.
Linda Caldwell
December 30, 2025 AT 17:36This is why we need more community labs. Local testing. People trust their neighbors more than the FDA. I started a group in my town-we test pills with cheap UV readers. It’s not perfect but it’s better than nothing. You don’t need a million-dollar machine to save a life.
Donna Packard
December 30, 2025 AT 22:36My dad took a generic statin for 5 years. Never had a problem. He’s 82 and still hikes. If it works, why panic? Not everything needs to be perfect-just good enough.
Patrick A. Ck. Trip
January 1, 2026 AT 00:25While the technological and regulatory frameworks outlined herein represent commendable strides in pharmaceutical integrity, one must not overlook the human dimension: the overburdened quality control technicians working double shifts, the junior chemists without proper training, the regulatory agencies stretched thin by geopolitical complexity. The system’s resilience is not in its algorithms, but in the quiet dedication of those who log data at 2 a.m. with tired eyes. We must honor them-not just audit them.